By Sulaiman Uppal
Fifth year medical student, University of Oxford
|
This is the winning essay from the 2021 BOA Medical Student Essay Prize As a medical student, what would encourage you to consider a career in T&O and what are the perceived barriers to such a career? |
Introduction
Choosing a specialty to pursue is a decision medical students grapple with throughout medical school. Currently, the General Medical Council recognises 65 specialties and 31 sub-specialties within the fields of medicine and surgery1, creating a heavy burden of choice. Trauma and Orthopaedics (T&O) is a popular and increasingly competitive specialty choice, with consistently more applications than posts available at specialty training level 3 (ST3)2 (Figure 1).
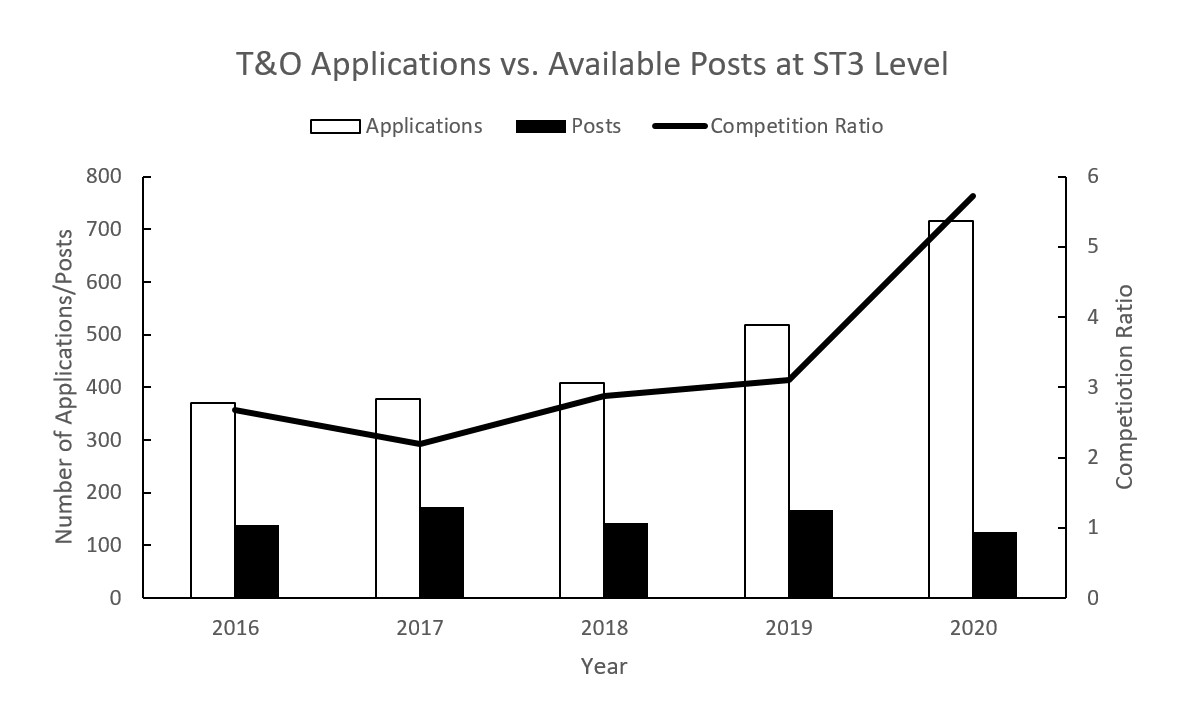
Figure 1: T&O Applications vs. Available Posts at ST3 Level.
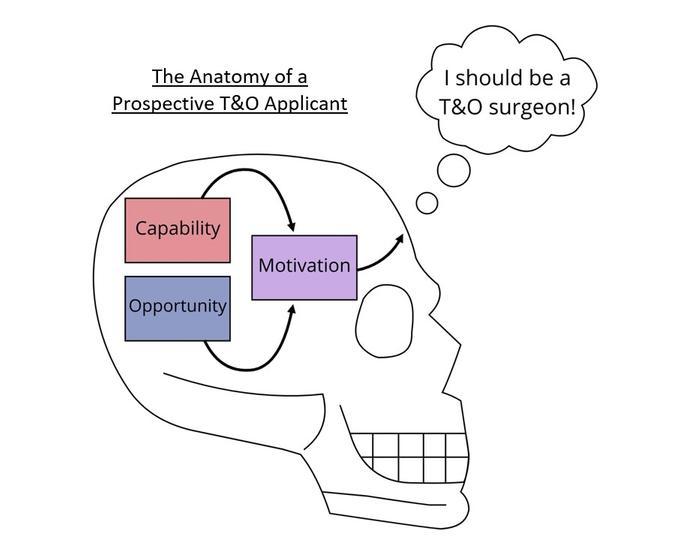
Why some choose T&O, whilst others do not, is in essence a question of human behaviour. It is a highly multifaceted decision; therefore, adopting a systematic approach is the best way to analyse the relevant factors. The COM-B system, a framework developed in the field of behavioural science, is a model based on the relationship between three key components: capability, opportunity and motivation3 (Figure 2). Adapting this model to analyse the interplay of these components provides a useful skeleton on which to assess the drivers and barriers to a career in T&O.
Capability
Capability describes an individual’s ability to perform the tasks required of T&O surgeons. Manual dexterity is required in all surgical careers, including T&O. A study found that medical students interested in surgical careers perceived their own manual dexterity as higher than those who were not. However, when manual dexterity was measured objectively in both groups, no significant difference was found – suggesting self-perception of dexterity may be a greater driver of surgical career choice than objective manual dexterity4. Furthermore, gender differences in visuospatial skills and gaming experience5,6 can mean that, on average, male medical students initially acquire surgical skills quicker6–8. This may discourage female medical students early on by impacting their self-perception of dexterity. However, providing feedback, one-to-one training and more practice eliminates these differences8–10, so a barrier for female medical students may simply be the standard surgical teaching environment.
T&O surgeons often endure physical strain, with one study finding 67% of T&O surgeons suffer work-related musculoskeletal disorders11. Another study found that 75% of medical students experienced musculoskeletal pain during surgical rotations and 31% reported that if surgery was less physically demanding, they would be more likely to consider it as a career12. T&O can be psychologically demanding as well; despite reporting high levels of career satisfaction, T&O surgeons also report a high burnout rate13–15. Burnout is a major concern for medical students16, so the stresses of a career in T&O, both physical and psychological, may be perceived as a significant barrier.
Opportunity
Opportunity, in this context, refers to factors external to a medical student that might influence their decision to pursue T&O. Strong evidence suggests that opportunities for positive surgical experiences are a key driver of interest in surgery, especially active involvement in operative procedures17. Student involvement may cause patient safety concerns, but a study following over 6,000 spinal surgeries found that medical student involvement did not significantly increase length of stay, infection or readmission18. Additionally, interest can be cultivated with improved preclinical education19 and involvement in surgery interest groups20.
Diversity issues and negative stereotypes can also pose a significant barrier to interest in T&O21. The stereotypical T&O surgeon is a strong but stupid man (efforts have been made to disprove their stupidity22) who strives to maintain an intimidating ‘boys’ club’ environment23–25. This perception can make T&O especially unattractive to female medical students26, which is further exacerbated by the low proportion of female consultants in T&O, at only 7%27. Positive role models drive specialty selection28, so the lack of female role models may contribute to a vicious cycle discouraging even more women from applying29. However, negative perceptions of T&O in medical students diminish after T&O rotations30, suggesting that social connotations and even ‘badmouthing’31 of T&O feed perceptions that create a significant barrier to medical student application.
Motivation
Motivation describes all mental processes that would energise and direct a medical student towards T&O. Motivation can be automatic and based on emotional impulses, but when making a complex decision, the key form of motivation is reflective. Reflective motivation involves future plans and evaluations of factors contained within capacity and opportunity. Multiple studies have found lifestyle factors to be the main determining factor for medical students when selecting a specialty32–34. ‘Lifestyle’ is a deceptively complex term and encapsulates different ideas about future plans, stress and work-life balance. T&O is perceived as an exciting, high-income specialty that provides instant gratification35, but also as stressful and requiring long hours34. The weighting of these factors tends to vary by gender, with male medical students prioritising income potential whilst female medical students are more likely to be deterred by work-life balance concerns34,36. For female medical students, these concerns may relate to family planning which is often subject to unfair bias37,38. It is important, however, to recognise that these are generalisations made across large samples and individual priorities may well differ. For all medical students, career planning involves contemplating future priorities, which in turn affects motivation in the present.
Conclusion
Using the COM-B system as a guide, the milieu of factors that affect the decision to choose T&O can be explored and categorised. For the motivation to pursue T&O to arise, drivers within capacity and opportunity must outweigh the barriers. These are summarised in Table 1. Overall, the main driver of pursuing T&O is interest seeded by positive role models and opportunities to meaningfully participate in procedures. The barriers converge on the idea of lifestyle, an amalgamation of interacting factors including working life, future plans and stress. Unfortunately, female medical students often perceive more barriers than their male counterparts – these issues must be addressed to allow a more diverse workforce to flourish. More opportunities for experience in T&O with positive role models and improved teaching environments may help correct this imbalance. T&O is a rewarding but challenging specialty, and for capable medical students motivated with the right opportunities, it can become a ‘bone’-a fide career.
|
Drivers and Barriers to a Career in T&O |
|
| Drivers | Barriers |
| Perceived Manual Dexterity | Physical and Psychological Demands |
| Experience in T&O surgery with positive involvement | Diversity Issues |
| Preclinical education | Negative Stereotypes |
| Positive role models | Learning style incompatible with standard teaching style |
| Action-packed job with gratifying patient outcomes | ‘Badmouthing’ |
| High job satisfaction | Stress and long hours |
| Potential for high income | Bias against parenthood/pregnancy |
References
- General Medical Council (2021). GMC approved postgraduate curricula. Available at: www.gmc-uk.org/education/standards-guidance-and-curricula/curricula.
- NHS Health Education England (2021). Competition Ratios. Available at: https://specialtytraining.hee.nhs.uk/Competition-Ratios.
- Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42.
- Lee JY, Kerbl DC, McDougall EM, Mucksavage P. Medical students pursuing surgical fields have no greater innate motor dexterity than those pursuing nonsurgical fields. J Surg Ed. 2012;69(3):360-3.
- Shane MD, Pettitt BJ, Morgenthal CB, Smith CD. Should surgical novices trade their retractors for joysticks? Videogame experience decreases the time needed to acquire surgical skills. Surg Endosc. 2008;22(5):1294-7.
- Enochsson L, Isaksson B, Tour R, Kjellin A, Hedman L, Wredmark T, Tsai-Felländer L. Visuospatial skills and computer game experience influence the performance of virtual endoscopy. J Gastrointest Surg. 2004;8(7):876-82; discussion 882
- Thorson CM, Kelly JP, Forse RA, Turaga KK. Can we continue to ignore gender differences in performance on simulation trainers? J Laparoendosc Adv Surg Tech A. 2011;21(4):329-33.
- Donnon T, DesCôteaux JG, Violato C. Impact of cognitive imaging and sex differences on the development of laparoscopic suturing skills. Can J Surg. 2005 Oct; 48(5):387-93.
- Strandbygaard J, Bjerrum F, Maagaard M, Winkel P, Rifbjerg Larsen C, Ringsted C, et al. Instructor feedback versus no instructor feedback on performance in a laparoscopic virtual reality simulator: A randomized trial. Ann Surg. 2013;257(5):839-44.
- White MT, Welch K. Does gender predict performance of novices undergoing Fundamentals of Laparoscopic Surgery (FLS) training? Am J Surg. 2012;203(3):397-400; discussion 400.
- AlQahtani SM, Alzahrani MM, Harvey EJ. Prevalence of musculoskeletal disorders among orthopedic trauma surgeons: An OTA survey. Can J Surg. 2016;59(1):42-7.
- Sergesketter AR, Lubkin DT, Shammas RL, Krucoff KB, Peskoe SB, Risoli Jr T, et al. The Impact of Ergonomics on Recruitment to Surgical Fields: A Multi-institutional Survey Study. J Surg Res. 2019;236:238-46.
- Balch CM, Shanafelt TD, Sloan JA, Satele DV, Freischlag JA. Distress and career satisfaction among 14 surgical specialties, comparing academic and private practice settings. Ann Surg. 2011;254(4):558-68.
- Sargent MC, Sotile W, Sotile MO, Rubash H, Barrack RL. Quality of life during orthopaedic training and academic practice. Part 1: Orthopaedic surgery residents and faculty. J Bone Joint Surg Am. 2009;91(10):2395-405.
- Rodrigues H, Cobucci R, Oliveira A, Victor Cabral J, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: A systematic review and meta-analysis. PLoS One. 2018;13(11):e0206840.
- Chau M, Aziz F. Factors Affecting the Interest in a Surgical Career among Medical Students at a Nonurban, Tertiary Care Academic Institution. Ann Vasc Surg. 2020;68:57-66.
- Marshall DC, Salciccioli JD, Walton S, Pitkin J, Shalhoub J, Malietzis G. Medical Student Experience in Surgery Influences Their Career Choices: A Systematic Review of the Literature. J Surg Educ. 2015;72(3):438-45.
- Abecassis ZA, Hopkins B, Win P, Yerneni K, Karras CL, Frankel HG, et al. Impact of medical student involvement on outcomes following spine surgery: A single center analysis of 6485 patients. J Clin Neurosci. 2019;69:143-148.
- McKinley SK, Sell NM, Saillant N, Coe TM, Lau T, Cooper CM, et al. Enhancing the Formal Preclinical Curriculum to Improve Medical Student Perception of Surgery. J Surg Educ. 2020;77(4):788-98.
- Song JSA, McGuire C, Vaculik M, Morzycki A, Plourde M. Cross sectional analysis of student-led surgical societies in fostering medical student interest in Canada. BMC Med Educ 2019;19:77.
- Curlewis K, Thornhill C, Leung B, Hamilton L, Ricketts D, Rogers B. The effects of sex, race and the hidden curriculum on medical students’ career choices: lessons for orthopaedics. RCS Bulletin. 2020;102(6):e7-e11.
- Subramanian P, Kantharuban S, Subramanian V, Willis-Owen SAG, Willis-Owen CA. Orthopaedic surgeons: As strong as an ox and almost twice as clever? Multicentre prospective comparative study. BMJ 2011;343:d7506.
- Oxtoby K. Do the classic specialty stereotypes still hold true for today’s doctors? BMJ 2013;347:f7454.
- Munro C, Nabavi N, Medical stereotypes: Just good fun or a barrier to diversity in our workforce? - The BMJ Opinion. Available at: https://blogs.bmj.com/bmj/2020/11/18/medical-stereotypes-just-good-fun-or-a-barrier-to-diversity-in-our-workforce.
- Hill EJR, Bowman KA, Stalmeijer RE, Solomon Y, Dornan T. Can i cut it? Medical students’ perceptions of surgeons and surgical careers. Am J Surg. 2014;208(5):860-7.
- Gargiulo DA, Hyman NH, Hebert JC. Women in surgery: Do we really understand the deterrents? Arch Surg. 2006;141(4):405-7; discussion 407-8.
- NHS Digital (2019). Medical and Dental staff by gender specialty and grade AH2667. Available at: https://digital.nhs.uk/data-and-information/find-data-and-publications/supplementary-information/2019-supplementary-information-files/medical-and-dental-staff-by-gender-specialty-and-grade-ah2667.
- Yoon JD, Ham SA, Reddy ST, Curlin FA. Role Models’ Influence on Specialty Choice for Residency Training: A National Longitudinal Study. J Grad Med Educ. 2018;10(2):149-54.
- Faucett EA, McCrary HC, Milinic T, Hassanzadeh T, Roward SG, Neumayer LA. The role of same-sex mentorship and organizational support in encouraging women to pursue surgery. Am J Surg. 2017;214(4):640-4.
- Rahman R, Zhang B, Humbyrd CJ, LaPorte D. How Do Medical Students Perceive Diversity in Orthopaedic Surgery, and How Do Their Perceptions Change After an Orthopaedic Clinical Rotation? Clin Orthop Relat Res. 2021;479(3):434-44.
- Hunt DD, Scott C, Zhong S, Goldstein E. Frequency and effect of negative comments (“Badmouthing”) on medical students’ career choices. Acad Med. 1996;71(6):665-9.
- Sutton PA, Mason J, Vimalachandran D, McNally S. Attitudes, motivators, and barriers to a career in surgery: A national study of uk undergraduate medical students. J Surg Educ. 2014;71(5):662-7.
- Rao RD, Khatib ON, Agarwal A. Factors Motivating Medical Students in Selecting a Career Specialty. J Am Acad Orthop Surg. 2017;25(7):527-35.
- Whitaker J, Hartley B, Zamora R, Duvall D, Wolf V. Residency Selection Preferences and Orthopaedic Career Perceptions: A Notable Mismatch. Clin Orthop Relat Res. 2020;478(7):1515-25.
- Schroeder J, Zisk-Rony RY, Liebergall M, Tandeter H, Kaplan L, Weiss YG, Weissman C. Medical students’ and interns’ interest in orthopedic surgery: The gender factor. J Surg Educ. 2014;71(2):198-204.
- Baldwin K, Namdari S, Bowers A, Keenan MA, Levin LS, Ahn J. Factors affecting interest in orthopedics among female medical students: A prospective analysis. Orthopedics. 2011;34(12):e919-32.
- Bohl DD, Iantorno SE, Kogan M. Inappropriate Questions Asked of Female Orthopaedic Surgery Applicants from 1971 to 2015: A Cross-sectional Study. J Am Acad Orthop Surg. 2019;27(14):519-26.
- Mulcahey MK, Nemeth C, Trojan JD, O’Connor MI. The Perception of Pregnancy and Parenthood among Female Orthopaedic Surgery Residents. J Am Acad Orthop Surg. 2019;27(14):527-32.
