Congress 2023 E-Poster Abstracts
Every year the BOA Annual Congress receives a wide range of abstract submissions covering all the sub-specialty in Trauma and Orthopaedics. This year is no different with over 600+ submissions. Below is the list of selected E-Poster abstracts for this year's Annual Congress in Liverpool.
Categories
Foot and Ankle - Poster Abstracts
28 - Removal of metalwork after Lisfranc fracture-dislocation internal fixation: A retrospective study from a major trauma centre with more than two years of follow-up
Sherif Ahmed Kamel1,2, Mayur Mohan1, Wagih Moussa1, Syed Anjum1
1University Hospital of Southampton NHS, Southampton, United Kingdom. 2Ain Shams University, Cairo, Egypt
Abstract
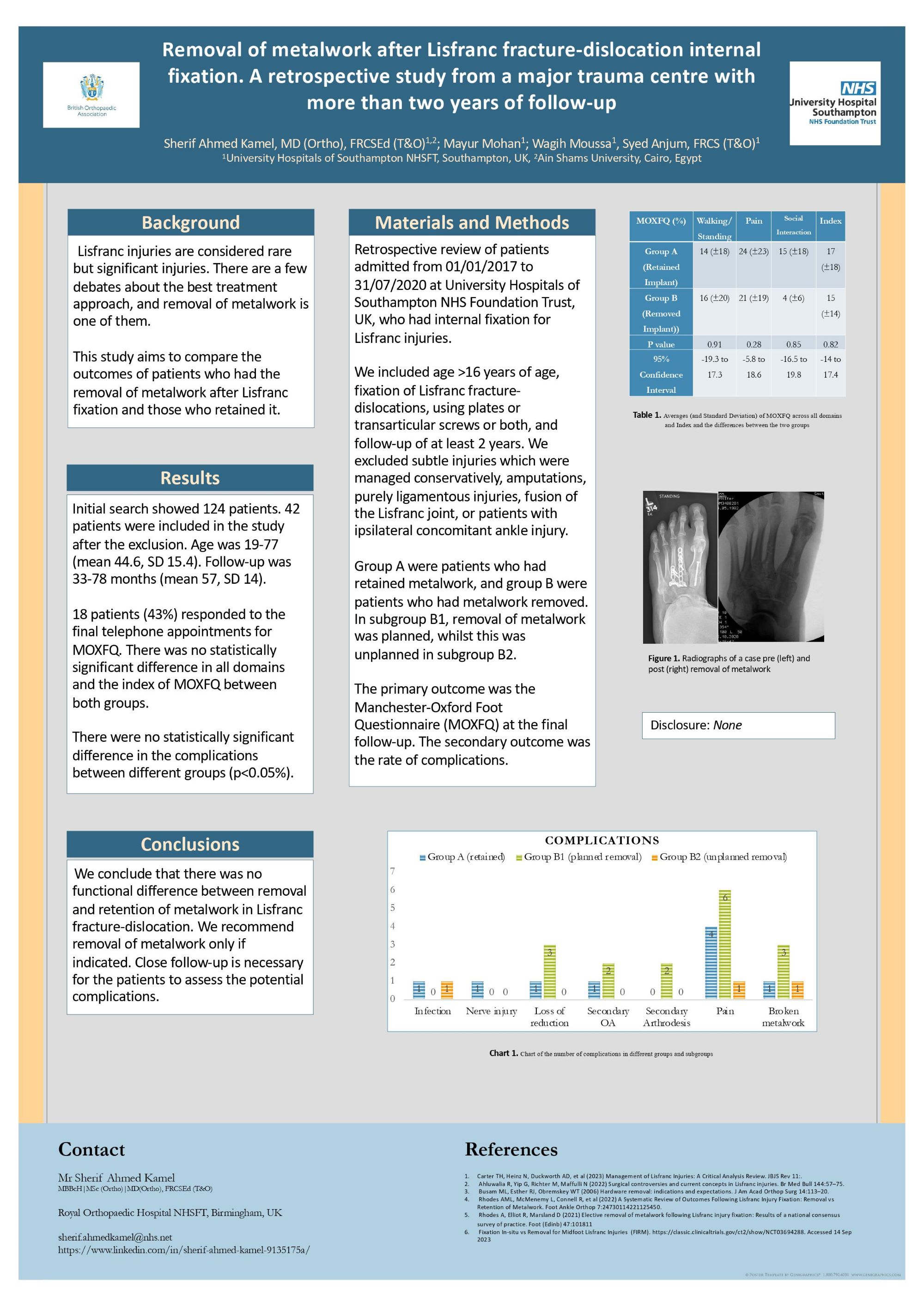
Background: Lisfranc injuries are considered rare but significant injuries. There are a few debates about the best treatment approach, and removal of metalwork is one of them. This study aims to compare the outcomes of patients who had the removal of metalwork after Lisfranc fixation and those who retained it.
Materials and Methods: Retrospective review of patients admitted from 01/01/2017 to 31/07/2020 at University Hospitals of Southampton NHS Foundation Trust, UK, who had internal fixation for Lisfranc injuries. We included age >16 years of age, fixation of Lisfranc fracture-dislocations, using plates or transarticular screws or both, and follow-up of at least 2 years. We excluded subtle injuries which were managed conservatively, amputations, purely ligamentous injuries, fusion of the Lisfranc joint, or patients with ipsilateral concomitant ankle injury. Group A were patients who had retained metalwork, and group B were patients who had metalwork removed. In subgroup B1, removal of metalwork was planned, whilst this was unplanned in subgroup B2. The primary outcome was the Manchester-Oxford Foot Questionnaire (MOXFQ) at the final follow-up. The secondary outcome was the rate of complications.
Results: Initial search showed 124 patients. 42 patients were included in the study after the exclusion. Age was 19-77 (mean 44.6, SD 15.4). Follow-up was 33-78 months (mean 57, SD 14). 18 patients (43%) responded to the final telephone appointments for MOXFQ. There was no statistically significant difference in all domains and the index of MOXFQ between both groups. There were no statistically significant difference in the complications between different groups (p<0.05%).
Conclusion: We conclude that there was no functional difference between removal and retention of metalwork in Lisfranc fracture-dislocation. We recommend removal of metalwork only if indicated. Close follow-up is necessary for the patients to assess the potential complications.
45 - Anterior talofibular ligament laxity is protective of deep deltoid laxity development in AAFD. A cadaver based study
Zhikai Li1, Zhiheng Li2, Gavin Jarvis3, Stephanie Potten1, Cecilia Brassett1, Chandra S Pasapula4
1University of Cambridge, Cambridge, United Kingdom. 2Wilson's School, Sutton, United Kingdom. 3University of Sunderland, Sunderland, United Kingdom. 4Queen Elizabeth Hospital King's Lynn, King's Lynn, United Kingdom
Abstract
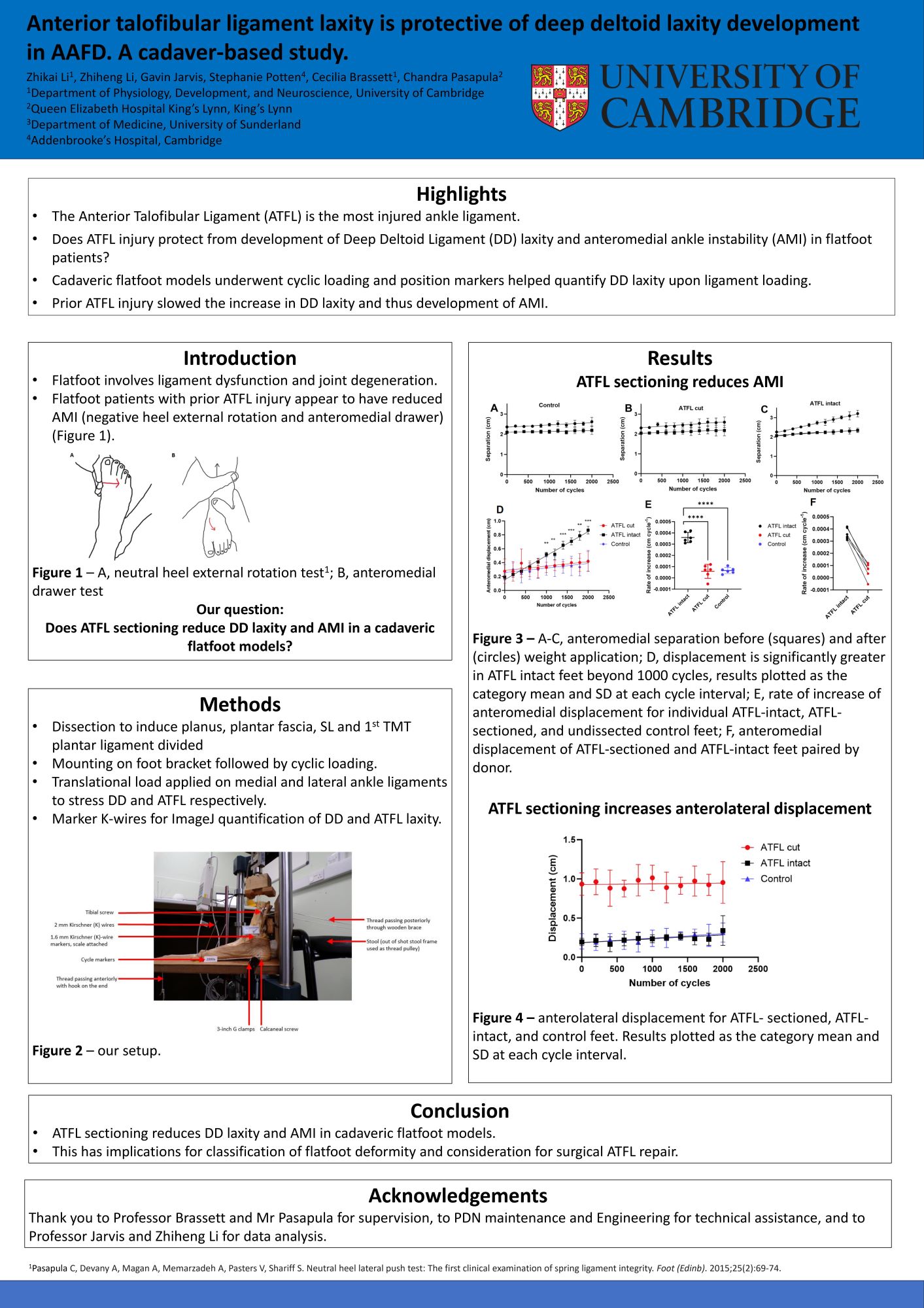
Background: Adult Acquired Flatfoot Deformity (AAFD) starts with failure of the medial longitudinal arch and subsequent ligamentous and joint degeneration. Progression to deep deltoid ligament (DD) laxity and anteromedial ankle instability (AMI) prior to complete DD rupture is poorly understood. Clinical observations indicate reduced AMI in the presence of anterior talofibular ligament (ATFL) laxity/rupture (a common ligament injury), a yet uncharacterised paradoxical stabilising effect which we aim to investigate in a cadaveric study.
Methods: Unstable planus was induced in 12 cadaveric feet from 6 donors and paired feet were randomly assigned to having ATFL sectioned or intact. Jig-mounted feet underwent 2000 cycles of cyclic loading between 1200N and 1500N, and photos were taken with markers on the medial malleolus, fibula, and the talus before and after antero-posterior force application to quantify anteromedial and anterolateral ankle displacement, which reflects DD and ATFL laxity respectively.
Results & Findings: In ATFL-intact feet, anteromedial displacement increased by 3.46 ± 0.41 µm/cycle (mean ± SD; p = 0.000005; two-tailed, one-sample t-test). In ATFL-sectioned feet, displacement increased 0.61 ± 0.66 µm/cycle (p = 0.072), an 82% reduction in DD laxity development (p = 0.00006; two-tailed, paired t-test). There was minimal change in anterolateral displacement (ATFL-intact: 0.50 ± 0.50 µm/cycle¯¹ (p = 0.06); ATFL-sectioned: -0.04 ± 0.90 µm.cycle¯¹ (p = 0.17). Absolute anterolateral displacement increased in ATFL-sectioned feet by 7.40 ± 0.12 mm (p = 0.00002).
Conclusions & Implications: These results corroborate clinical findings of a paradoxical stabilising effect of ATFL injury on DD and reduced AMI in AAFD. They have significant implications in determining which feet progress to DD laxity and ultimately, DD rupture. Patients with AAFD may need counselling regarding the development of DD laxity after surgical ATFL repair. Current classifications may require modification to reflect this phenomenon.
411 - Tendon to Tendon Versus Tendon to Bone Transfers in Charcot-Marie-Tooth pes cavovarus correction
Ella McCarthy1, Gilles van Eetvelde1, Muhammad Chatoo1, Shelain Patel1,2, Nicholas Cullen1, Karan Malhotra1,2, Matthew Welck1,2
1Royal National Orthopaedic Hospital, Stanmore, United Kingdom. 2University College London, London, United Kingdom
Abstract
Background: Charcot-Marie Tooth (CMT) commonly presents with a cavovarus foot deformity. Surgical correction involves bony correction and a tendon transfer, most commonly the tibialis posterior. Commonly used methods of transfer include tendon-to-tendon or tendon-to-bone. Although differences between these techniques have been evaluated for patients with foot drop, no previous studies have specifically compared their results following surgery for CMT. Our aim was to compare subjective outcomes and complications between these techniques of tendon transfer in patients with CMT.
Methods: This was a single-centre retrospective series over a 10-year period. We included patients with CMT undergoing an identical flexible cavovarus foot correction comprising a calcaneal osteotomy, a 1st metatarsal dorsiflexion osteotomy and a tibialis posterior tendon transfer. We excluded patients under 18 years and those who had previous surgery. Subjective assessment was done using a questionnaire based on the Stanmore score and using the MOxFQ patient reported outcome score.
Results: 42 patients were included with mean follow-up of 60 months (12-134 months). 31 had tendon-to-bone transfers and 11 had tendon-to-tendon. The MOxFQ significantly improved in both groups, but there was no difference in improvement between the groups (p>0.05). Patients in their 30s had a greater improvement in MOxFQ-Walking than older patients regardless of procedure (p=0.002). The only subjective differences noted between groups were: balance was better in the tendon-to-tendon group (p=0.037), whilst tendon-to-bone had less requirement for orthotics (p=0.027). there was no overall significant difference in subjective improvements in power or range of movement between groups. There was no significant difference in complications or recurrence rates (p>0.05).
Conclusions: We did not demonstrate any clinically meaningful differences in outcome between transferring the tibialis posterior to tendon or bone in CMT cavovarus foot correction. The choice of tendon transfer can therefore be at the discretion of the surgeon, guided by patient specific factors.
466 - Static versus Dynamic Fixation of the Ankle Syndesmosis: a Systematic Review and Meta-Analysis
Reuben Varghese Philip1, Aryan Mohajerani1, Alan Norrish1,2
1Academic Orthopaedics, Trauma and Sports Medicine, School of Medicine, University of Nottingham, Queen’s Medical Centre, Nottingham, United Kingdom. 2Department of Orthopaedic Trauma, Nottingham University Hospitals NHS Trust, Queen’s Medical Centre, Nottingham, United Kingdom
Abstract
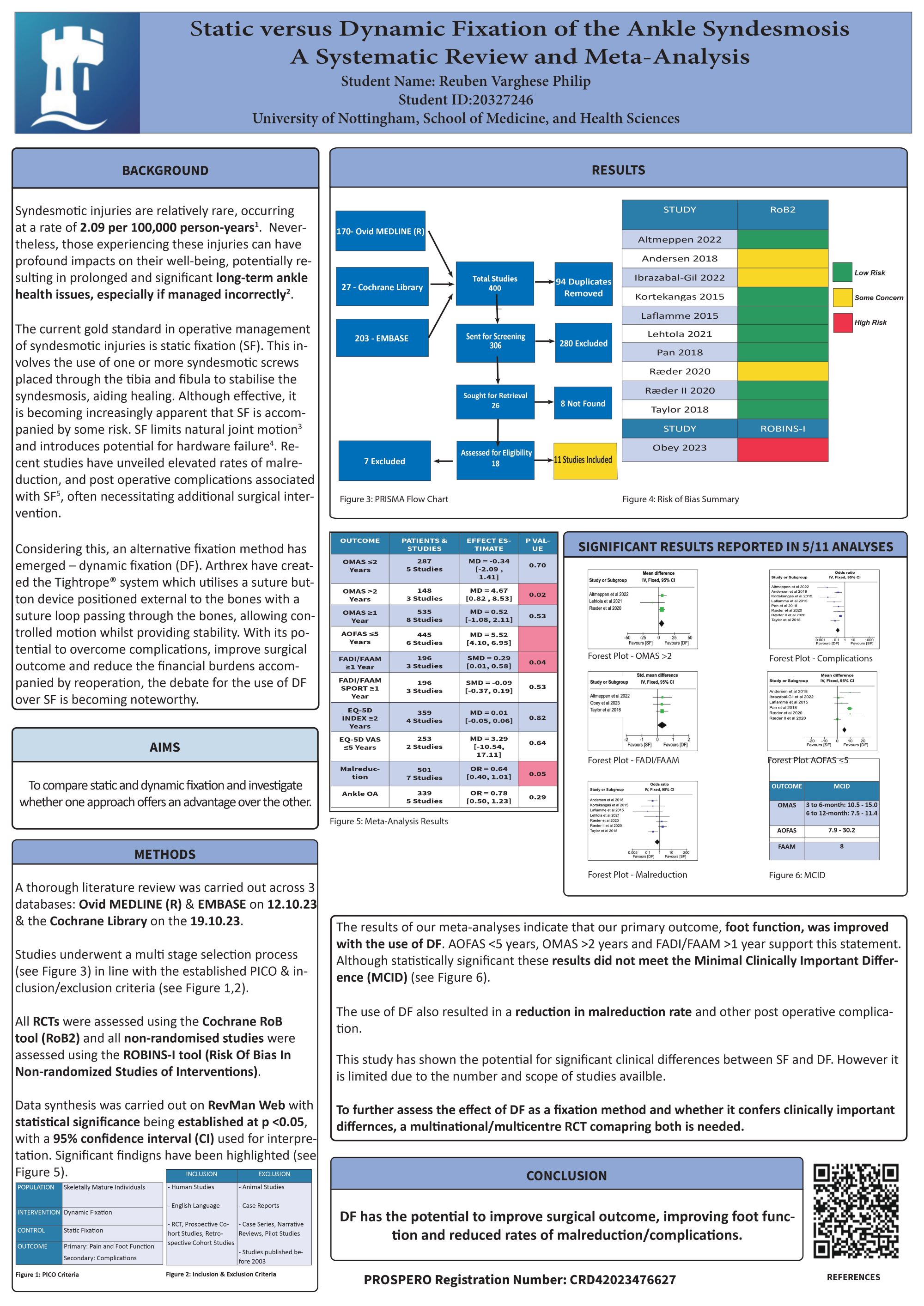
Background: Current best practise for Syndesmotic injury management is debated. This study aims to assess and compare both static (SF) and dynamic fixation (DF) through a systematic review and meta-analysis.
Methods: The PRISMA guidelines were used and the study was registered with PROSPERO ( CRD42023476627). The primary outcome of this study was ankle function and pain, assessed using patient-reported outcome measure scores: OMAS, AOFAS, FADI/FAAM, EQ-5D Index/VAS. The secondary outcome assessed was malreduction and postoperative complications.
Results: In total 11 studies were included for meta-analysis, involving 791 patients: 395 – DF, 396 – SF. OMAS >2 years post-surgery was significantly better in the DF vs SF group (4.67 MD, 95%CI 0.82 to 8.53, P=0.02, I2=12%). AOFAS ≤ 5 years post-surgery was significantly better in the DF vs SF group (5.52 MD, 95%CI 4.10 to 6.95, P<0.00001, I2=87%). FADI/FAAM score ≥1 year post surgery was significantly better in the DF vs SF group, (0.29 MD, 95%CI 0.01 to 0.58, P=0.04, I2=0%). Rates of malreduction were significantly less in the DF vs SF group (0.64 OR, 95%CI 0.40 to 1.01, P=0.05, I2=65%). Overall, complication rates were significantly less in the DF vs SF group (0.15 OR, 95%CI 0.10 to 0.24, P<0.00001, I2=69%).
Conclusion: This study provides clinical evidence that supports DF over SF. In particular, DF confers better function, reduced malreduction and fewer complications. This meta-analysis suggests that funding would be justified to support fully powered, large-scale randomised controlled trials to confirm whether DF can have clinically important differences over SF for patients undergoing syndesmotic fixation.
Impact: Dynamic fixation of the syndesmosis with suture fixation may have improved clinical outcomes over static fixation of syndesmotic injuries with one or more screws.
670 - Comparing the Efficacy of Bohler Iron Off Loader Casts Versus Total Contact Casts in Treating Diabetic Foot Ulcers
Sharan Sambhwani1, Vidhi Adukia1, Latika Ahuja2, Michael Pierides1, Sayyied Kirmani1
1Kettering General Hospital, Kettering, United Kingdom. 2University of West England, Bristol, United Kingdom
Abstract
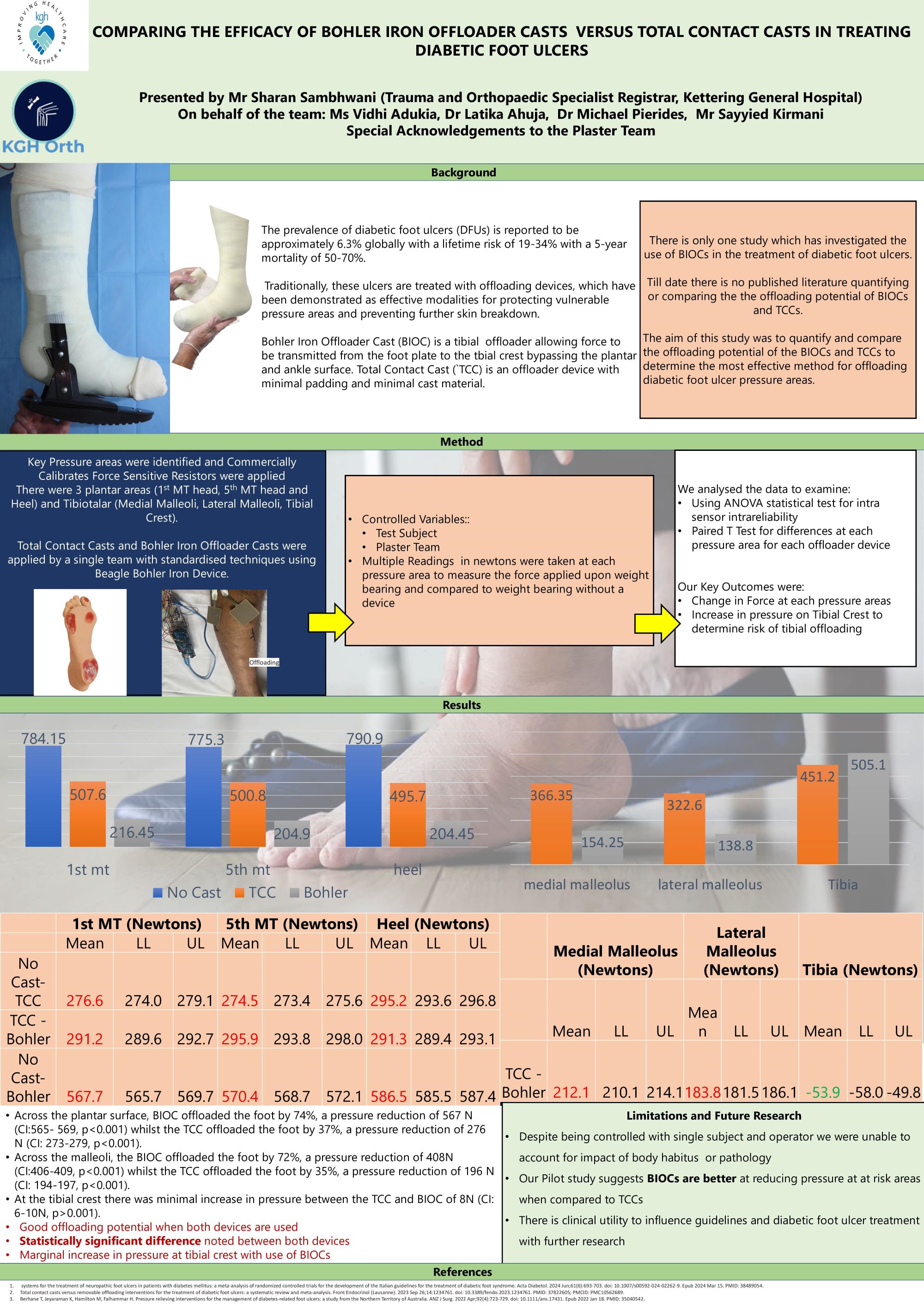
Background: The prevalence of diabetic foot ulcers is reported to be approximately 6.3% globally. Traditionally, these are treated with offloading devices, such as Bohler iron offloader casts (BIOCs) or total contact casts (TCCs), both of which are effective modalities for protecting vulnerable pressure areas and preventing further skin breakdown. Till date there are no published research quantifying their offloading potential in treating ulcers.
The aim of this study was to quantify and compare the offloading potential of the BIOCs and TCCs to determine the most effective method for offloading diabetic foot ulcer pressure areas.
Methods: Readings were taken at 6 pressure areas ( 1st and 5th metatarsal heads, heel, both malleoli and tibial crest) using commercially calibrated sensors applied on the skin using both TCC and BIOC. Results were compared using ANOVA statistical tests and paired T tests.
Results: Across the plantar surface, BIOC offloaded the foot by 74%, a pressure reduction of 567 N (CI:565- 569, p<0.001) whilst the TCC offloaded the foot by 37%, a pressure reduction of 276 N (CI: 273-279, p<0.001). Across the malleoli, the BIOC offloaded the foot by 72%, a pressure reduction of 408N (CI:406-409, p<0.001) whilst the TCC offloaded the foot by 35%, a pressure reduction of 196 N (CI: 194-197, p<0.001). At the tibial crest there was minimal increase in pressure between the TCC and BIOC of 8N (CI: 6-10N, p>0.001).
Conclusion: This study is the first of its kind, providing quantitative data demonstrating that both the BIOC and TCC are effective offloading devices that can be used to protect pressure areas in patients with diabetic foot ulcers as a mode of treatment. However, the results suggest that BIOCs have a greater offloading potential when compared with the TCC and therefore could result in better clinical outcomes, for which further research is planned.
General Orthopaedics - Posters
166 - Chronic Liver Disease and Hip Fracture Risk: A Comprehensive Meta-Analysis of Over One Million Patients

Eslam Abdelhady1, Mohamed A. Khalafallah2, Atef Abdelrahman Hassan3, Abdelaziz Hamoda4, Duncan Muir5, Mohamed A Imam6
1Faculty of medicine, Mansoura University, Mansoura, Egypt. 2Faculty of medicine, Alexandria University, Alexandria, Egypt. 3Faculty of medicine, Al-Azhar University, Cairo, Egypt. 4Faculty of medicine, Al-Alzhar Damiettaa University for Boys, Cairo, Egypt. 5East Surrey Hospital, Redhill, Redhill, United Kingdom. 6Ashford and Saint Peters NHS Trust, Chertsey, United Kingdom
Abstract
Background: Chronic liver disease (CLD) is a major health problem that affects approximately 4% of the global population. It can lead to many health complications including osteoporosis which can in-turn lead to hip fractures. However, studies investigating the hip fracture risk in CLD patients have yielded contradictory results.
Methods: A systematic review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) checklist. An electronic search of online databases (PubMed, Web of Science, Scopus, and Cochrane Library) was performed, identifying studies reporting hip fracture risk in CLD. Primary outcome was hip fracture prevalence in patients with CLD.
Results: Three studies with a total of 1,128,658 patients were identified. CLD showed no effect on increasing hip fracture risk compared to the non-CLD group, with a pooled hazard ratio of 1.34 (95% confidence interval (CI) 0.86, 2.09; P =0.20). Studies exhibited significant heterogeneity due to methodological differences. After sensitivity analysis and individual study removal, the overall hazard ratio was 1.04 (95% CI 0.93, 1.16; P =0.53), and the results were statistically insignificant.
Conclusion: CLD does not increase the risk of hip fracture, however further research is needed to investigate different types of CLD and hip fracture association. Guidelines should be developed to address hip fracture prevention in the CLD population.
256 - Management and Outcome of Native Joint Septic Arthritis: a single centre UK study
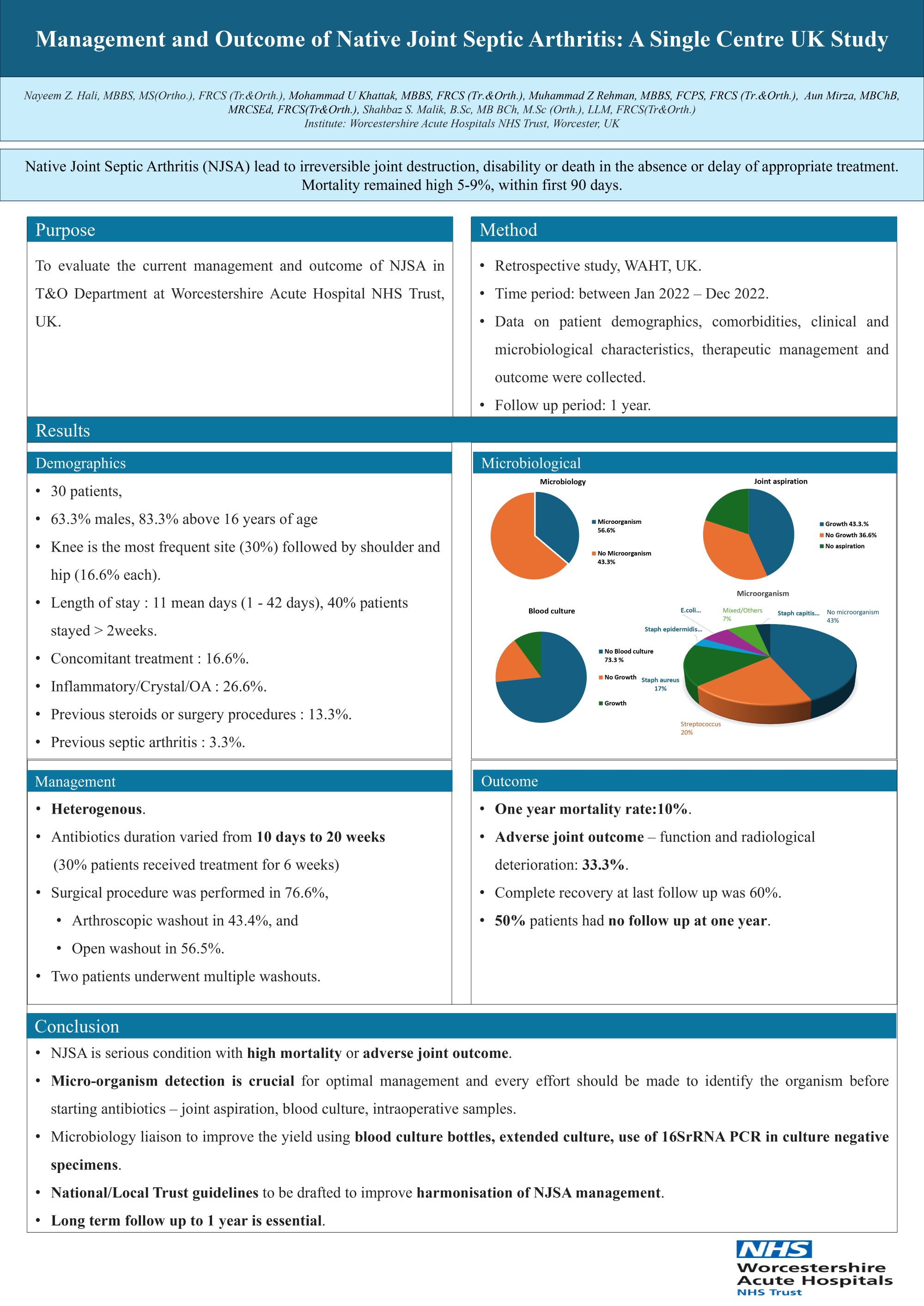
Nayeem Hali, Mohammad Khattak, Mohamed Shaalan, Muhammad Zain-Ur-Rehman, Aun Mirza, Shahbaz Malik
Worcestershire Acute Hospitals NHS Trust, Worcester, United Kingdom
Abstract
Background: Native Joint septic arthritis (NJSA) lead to irreversible joint destruction, disability or death in the absence or delay of appropriate treatment. Mortality remained high 5-9%, within first 90 days. The purpose of this study is to evaluate the current management and outcome of NJSA in T&O department at Worcestershire Acute Hospitals NHS Trust (WAHT), UK.
Method: This was a retrospective study performed at WAHT, UK. Data on patient demographics, comorbidities, clinical and microbiological characteristics, therapeutic management and outcome were collected between January 2022 to December 2022 with follow up to one year.
Results: Overall, 30 patients were included, 63.3% were males and 83.3% were above 16 years. Knee was the most frequent site (30%) followed by shoulder and hip (16.6% each). Staphylococcus and streptococcus were the common pathogens (20% each) and no microorganisms were found in 43.3%. Management was heterogenous. Antibiotics duration varied from 10 days - 20 weeks ( 30% patients received treatment for 6 weeks). Surgical procedure was performed in 76.6%, arthroscopic washout in 43.4% and open washout in 56.5%. Two patients underwent multiple washouts. One year mortality rate was 10%, adverse joint outcome - functional and radiological deterioration in 33.3%, complete recovery at last follow up was 60%. However, 50% patients had no follow up at one year.
Conclusion: NJSA is a serious condition with high mortality or adverse joint outcome. Microorganisms detection is crucial for optimal management and every effort should be made to identify the organism before starting antibiotics – joint aspiration, blood culture, intraoperative samples. Microbiology liaison to improve the yield through the use of blood culture bottles, extended culture, use of 16SrRNA PCR in culture negative specimens. National / Local Trust guidelines to be drafted to improve harmonisation of NJSA management. Long term follow up is essential.
502 - Cumulative patient risk profiling for lower limb arthroplasty: A large data machine learning model
Frank Davis1, Joideep Phadnis1, Sandeep Chauhan1,2, Jan Gosiewski2, James Farrant-Jayawant2, Benedict Rogers1
1University Hospital of Sussex, Brighton, United Kingdom. 2Definition Health, Brighton, United Kingdom
Abstract
Background: Numerous clinical factors have affected adverse outcomes in lower limb arthroplasty. The combined effect of multiple factors on patient reported outcome scores (PROMs) remains unclear. Greater stratification of cumulative risks will afford better decision making by both clinicians and patients. Statistical algorithms, learning from continuously collected patient data, enable machine learning to provide predictive analysis of multiple risk factors. This study, one of the first using large data machine learning, aims to improve patient risk profiling for lower limb arthroplasty
Methods: This multi-centre study prospectively collected data using a digital pre-operative assessment tool - LifeBox - as part of routine clinical practice. Ethical approval not necessary, as determined by the Health Regulation Agency (HRA) decision tool (1). Clinical data relevant to pre-operative screening, including the Oxford Knee Score (OKS) and Oxford Hip Score (OHS), creating a dataset of 36,000 data points. Patient data was correlated to post-operative pain, measured using a 0 and 100 score. Statistical analysis on these data points were performed with K-Fold cross-validation and Shapley Additive exPlanations (SHAP) values to determine feature importance.
Results: Excluding osteoarthritis and using SHAP values, the following predict poor outcomes after arthroplasty surgery:
- Multiple co-morbidities
- Osteoarthritis of other joints
- Use of a walking aid
- Depression
- Ex Smoker
Discussion: This large data model of patient risk factors, using predictive analysis machine learning, demonstrates, with high statistical power, associations with inferior outcomes. The number of co-morbidities per se affords the greatest prediction. Previous smoking, use of walking aids, depression are highlighted as a further 3 independent negative risk factors.
Conclusion: Utilising machine learning on large data models, affords superior risk stratification for patients undergoing lower limb arthroplasty. Further modelling, using similiar methods, will improve risk profiling with the associated clinical, financial and medicolegal benefits.
References
527 - C7 motor fascicle transfer to spinal accessory nerve for trapezius reanimation: a case series from the Peripheral Nerve Injury Unit at the Royal National Orthopaedic Hospital
Kapil Sugand1,2, Anthony Kinnair1, Edward Karam1, James Bennett1, Anna Panagiotidou1, Tom Quick1, Marco Sinisi1, Mike Fox1
1RNOH, Stanmore, United Kingdom. 2Imperial College, London, United Kingdom
Abstract
Background: Spinal accessory nerve (SAN) paresis is disabling, painful and associated with visual stigma. We aimed to reanimate trapezius using the motor fascicle from the C7 nerve root.
Methods: Surgical technique consisted of an anterior oblique supraclavicular approach along Langer's lines, divided omohyoid, exposure of upper and middle trunks prior to identifying C7 nerve. An epineurotomy was done to confirm a motor fascicle, preferably a fascicle innervating latissimus dorsi on stimulation which was cut distally. The SAN was then identified and cut proximally. Neurorrhaphy was performed with use of 9/0 nylon suture and fibrin glue. Since the data were non-parametric, the median, median absolute deviation, ranges and Bonett Price 95% confidence intervals were calculated.
Results: 5 patients were selected for surgery over an 18-year period. All right-handed, 3 males and 2 females had a median age of 40 years (±8; IQR: 33-48; 95% CI: 27-53), waited for a median time of 22 days (±17; IQR: 7-101; 95% CI: 0-197) until first clinic appointment and decision to surgery, median time of 38 days (±37; IQR: 1-66; 95% CI: 0-101) until surgery from presentation, first clinic follow-up at 12 weeks, and a median follow-up time of 38 months (±3; IQR: 36-40; 95% CI: 4-73). Commonest causes were iatrogenic and RTA. Patient outcomes at first follow up at 3 months included improved pain in 4 patients and shoulder forward flexion to 110 degrees documented in 1 patient. There was neurophysiological evidence of reinnervation by 10 months in 1 patient. By time of discharge shoulder forward flexion was possible between 110-150 degrees in 3 patients while 1 patient has yet to attend her 3-month follow-up.
Conclusion/Findings: C7 motor fascicle transfer to SAN is a useful and effective procedure for reanimating the unilateral trapezius to improve range of movement and neuropathic pain.
545 - Safety of same-day discharge knee arthroplasty surgery: An analysis of Hospital Episode Statistics data for England
Oliver Adebayo, Tim Briggs, William Gray
1. Getting It Right First Time programme, NHS England and NHS Improvement, London, United Kingdom
Abstract
Background: Same-day discharge total knee arthroplasty (TKA) , although still only performed regularly in a few hospital trusts in England is becoming more common. As elective surgical services recover from the COVID-19 pandemic a movement towards same-day discharge TKA surgery may help reduce waiting lists. However, evidence is needed to show that same-day discharge TKA is safe. We aimed to use a nationwide administrative data source to investigate the safety of same-day discharge TKA.
Methods: We extracted data from the Hospital Episodes Statistics database for the six years from 1st April 2017 to 31st March 2023. Patients undergoing primary elective TKA aged ≥ 17 years were included. The primary outcome was emergency readmission within 30 days of surgery. Propensity score matching was used to compare outcomes for those operated on as same-day discharge and those with an overnight stay after adjusting for demographic, frailty, comorbidity and procedural covariates.
Results: Data was available for 398,771 patients, of whom 3,718 (0.9%) were discharged on the same-day that they were admitted. Rates of same-day discharge increased from 0.5% in 2017/18 to 1.6% in 2022/23. There was a significantly increased odds of all-cause 30-day readmission in same-day discharge patients across the entire six year (coefficient 0.018, 95% confidence interval 0.011 to 0.025) but not for 2022/23 (coefficient 0.009, 95% confidence interval -0.001 to 0.020). However, complication rates were significantly lower with same-day discharge across the six-years and for 2022/23 only. Comparing trusts with > 5% and 0% same-day discharge rates for 2022/23 outcomes were either no different or better in same-day discharge patients.
Conclusions: Same-day discharge TKA is safe and outcomes have improved as the practice has become more common. Same-day discharge TKA may help to improve patient outcomes and increase the efficiency of the procedure.
621 - Outcome of DAIR in TJI: A Retrospective analysis of our results from 2015
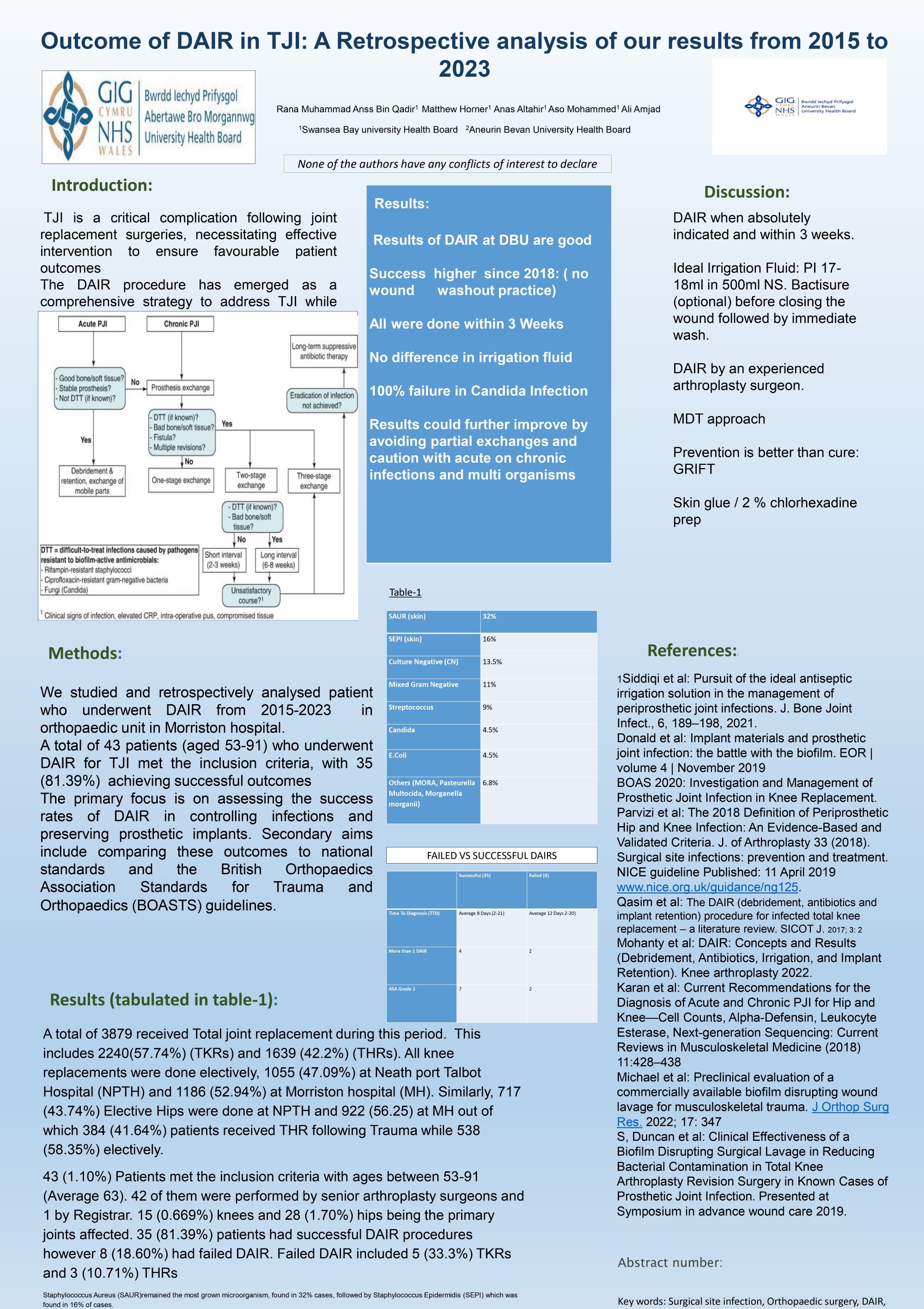
Rana Muhammad Anss Bin Qadir1, Ali Amjad2, Anas Altahir1, Aso Mohammed1
1Swansea Bay University Health Board, Swansea, United Kingdom. 2Aneurin Bevan University Health Board, Newport, United Kingdom
Abstract
Background: Prosthetic joint infection (PJI) is one of the most feared and challenging complications following total joint arthroplasty. Aim of this study is to analyse the effectiveness of debridement and implant retention (DAIR) in our patients with PJI (hips and knees) and evaluate outcomes with follow-up of not less than one year.
Patients and Methods: Patients in whom DAIR was performed were identified from our IT digital and clinical portals between 2015 and 2023. Adherence to criteria for DAIR was assessed according to BOAST standards published previously.
Results: DAIR was performed as part of a curative procedure in 28 hips and 15 knees (total 43 cases) with confirmed diagnosis of PJI within 3 weeks of presentation of symptoms. The mean age was 63 years (53 to 91), including 18 women and 25 men. Patients followed up by the treating team with clinical outcome measured using OKS/OHS + radiological assessment. Mean follow up was 18 months (1-6 years). 35 of the patients (81%) had a successful DAIR outcome compared to 8 failed DAIR (5 knees, 3 hips). Of the 8 failed DAIR (19%): 2 patients’ PJI were confirmed Candida, 2 had “partial modular component exchange, 2 were acute on chronic infections, 1 with confirmed multiresistance organisms from soft tissue biopsies obtained during the DAIR and one patient had a flare up of infection 2 years after the DAIR procedure following a dental procedure.
Conclusion: Prompt surgical treatment with DAIR, following strict diagnostic and therapeutic criteria, in patients with suspected periprosthetic joint infection, can lead to high rates of success in eradicating the infection.
692 - Retrospective Analysis of Orthopaedic Complications at a District General Hospital Over an 11-Year Period
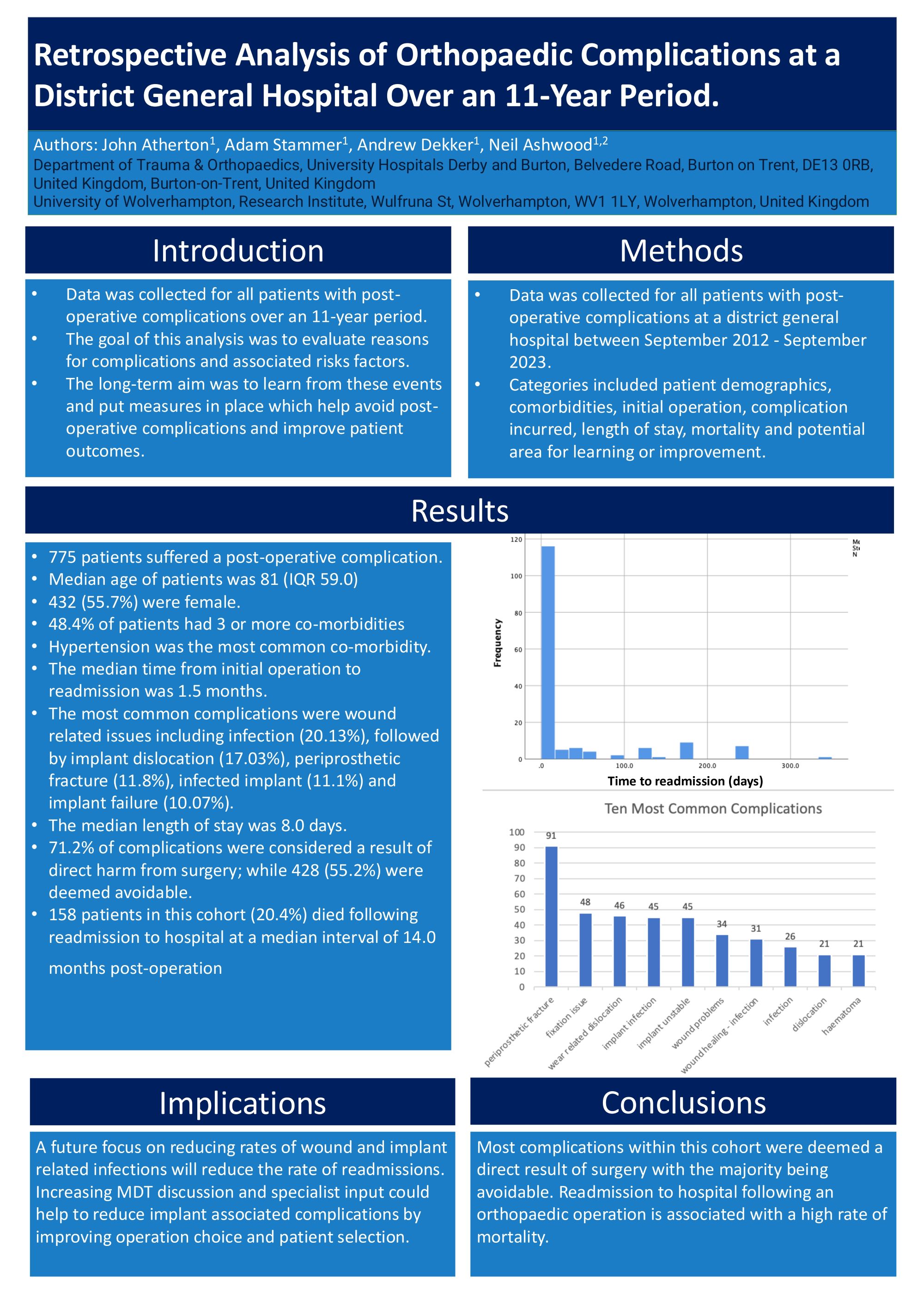
Adam Stammer1, Andrew Dekker1, Neil Ashwood1,2, John Atherton1
1Department of Trauma & Orthopaedics, University Hospitals Derby and Burton, Belvedere Road, Burton on Trent, DE13 0RB, United Kingdom, Burton-on-Trent, United Kingdom. 2University of Wolverhampton, Research Institute, Wulfruna St, Wolverhampton, WV1 1LY, Wolverhampton, United Kingdom
Abstract
Background: Data was collected for all patients with post-operative complications over an 11-year period. The goal of this analysis was to evaluate reasons for complications and associated risks factors. The long-term aim was to learn from these events and put measures in place which help avoid post-operative complications and improve patient outcomes.
Methods: Data was collected for all patients with post-operative complications at a district general hospital between September 2012 - September 2023. Categories included patient demographics, comorbidities, initial operation, complication incurred, length of stay, mortality and potential area for learning or improvement.
Results: 775 patients suffered a post-operative complication. The median age of patients was 81 (IQR 59.0) and 432 (55.7%) were female. 48.4% of patients had 3 or more co-morbidities, the most common being hypertension. The median time from initial operation to readmission was 1.5 months. The most common complications were wound related issues including infection (20.13%), followed by implant dislocation (17.03%), periprosthetic fracture (11.8%), infected implant (11.1%) and implant failure (10.07%). The median length of stay was 8.0 days. 71.2% of complications were considered a result of direct harm from surgery; while 428 (55.2%) were deemed avoidable. 158 patients in this cohort (20.4%) died following readmission to hospital at a median interval of 14.0 months post-operation.
Conclusions / findings: Most complications within this cohort were deemed a direct result of surgery with the majority being avoidable. Readmission to hospital following an orthopaedic operation is associated with a high rate of mortality.
Implications: A future focus on reducing rates of wound and implant related infections will reduce the rate of readmissions. Increasing MDT discussion and specialist input could help to reduce implant associated complications by improving operation choice and patient selection.
Knee - Poster Abstracts
32 - Medium-Term Outcome Of Medial Patellofemoral Ligament Reconstruction Using Synthetic Graft
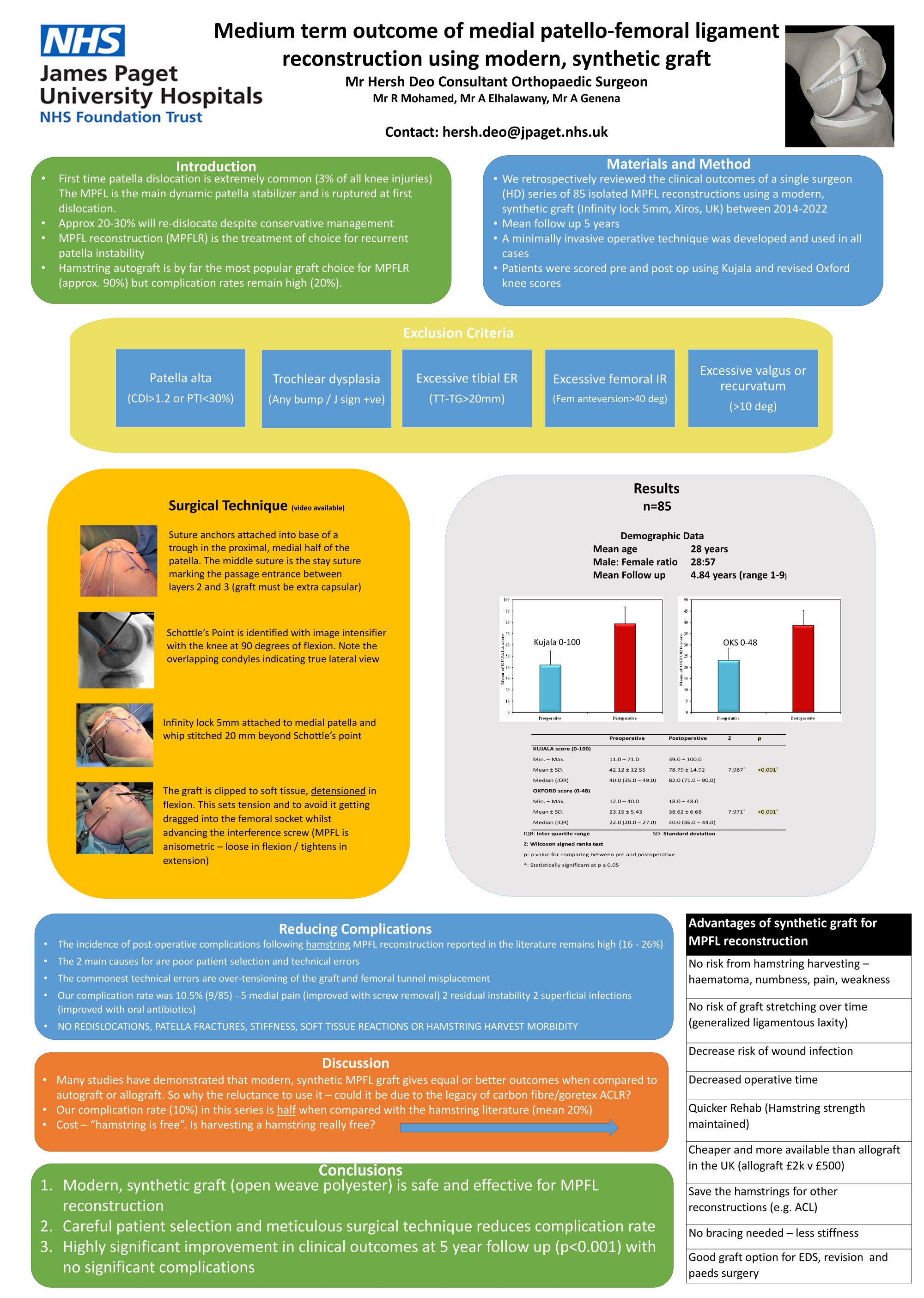
Hersh Deo, Ahmed Elhalawany
James Paget University Hospital, Norfolk, United Kingdom
Abstract
Background: Recurrent patella instability is a common and debilitating condition which affects mainly adolescents and young adults. Medial patellofemoral ligament (MPFL) reconstruction is the most popular surgical treatment for recurrent patella instability.
The most common graft choice in the literature is ipsilateral hamstring tendon (gracilis or semitendinosis) but the complication rate remains high (11–26%). Conversely, there are very few papers on the use of modern, synthetic grafts.
Objectives: Assessment of the medium-term function and clinical outcome of medial patellofemoral ligament reconstruction using synthetic graft
Study Design & Methods: A total of 85 patients who underwent MPFL reconstruction using a modern, synthetic graft (Xiros, UK) from 2014 to 2022 were retrospectively reviewed. Exclusion criteria were patella alta, malalignment, trochlea dysplasia and significant pain between episodes of instability. The author has developed an operative technique which is anatomic, minimally invasive and reproducible. Pre- and post-operative Kujala and Oxford knee scores were collected and analysed.
Results: The male to female ratio was 27:58, the average age was 28 years, and the follow-up range was 1–9 years (mean follow-up 4.84 years). We found a statistically significant improvement in mean Kujala and Oxford knee scores (P < 0.001) postoperatively. No major complications such as knee stiffness, soft tissue reaction, re-dislocation, or patella fracture were identified in the series. There were nine minor complications (10.6%): five cases of medial knee pain, two cases of residual instability and two of superficial infection.
Conclusions: This study demonstrates that modern, synthetic graft is a viable option for MPFL reconstruction. The technique described, achieves good clinical outcomes with low complication rates when compared with the published literature.
48 - Can we preoperatively predict chronic pain risk following Total Knee Replacement? A retrospective study at a secondary care hospital

Bhavesh Santani, Diego Leopoldo Vergara Janadoni, Abhina George, Shubhabrata De, Ashwin Unnithan, Ulfat Sardar, Venancio Manipol, Rakshya Upreti
Ashford and St Peter's Hospitals, Chertsey, United Kingdom
Abstract
Background: Annually, up to 20% of patients develop chronic post-surgical pain following Total Knee Replacement (TKR), imposing a significant financial burden, with over £700 million per year is spent on its management. Chronic pain can profoundly impact patients’ biopsychosocial well-being. This study aims to correlate pre-operative risk factors with the development of chronic post-surgical pain.
Methodology: This was a single-centre retrospective cohort study on patients who had a TKR in 2019-2021. The study identified patients experiencing chronic post-surgical pain, including those referred to pain specialists. Patient characteristics and pre-operative risk factors with significant correlation with chronic pain post TKR were identified. ROC curve analysis facilitated the development of a predictive score for pre-operative chronic pain risk.
Results: Out of 900 patients, 15% (131) developed chronic post-surgical pain after TKR, with 23% (30) of these referred to specialist pain management. Common characteristics among these patients included being aged 70-79 years, female, and having a high BMI. Identified risk factors for developing chronic pain included mental health conditions, preoperative opioid use, primary pain conditions and diabetes. From these findings, the MeOPD score was developed, which categorises patients into high and low risk pre-operative groups: MeOPD score= Mental health Conditions (2) + Preoperative Opioid Use (1) + Pain conditions (2) + Diabetes(1)
Conclusion & Implications: Patients scoring 3 or higher on the MeOPD score should be referred for specialist risk counselling regarding the potential development of chronic pain after TKR. This will reduce the cost for the investigation and management of chronic pain; up to £1,290,000 may have been saved if applied to the 131 TKR patients with chronic post-surgical pain. Additionally, the MeOPD score might help shorten waiting lists by providing patients with more informed risk counselling, potentially leading some to opt out for surgery.
168 - Survivorship of 500 Cementless Total Knee Arthroplasties in Patients under 55
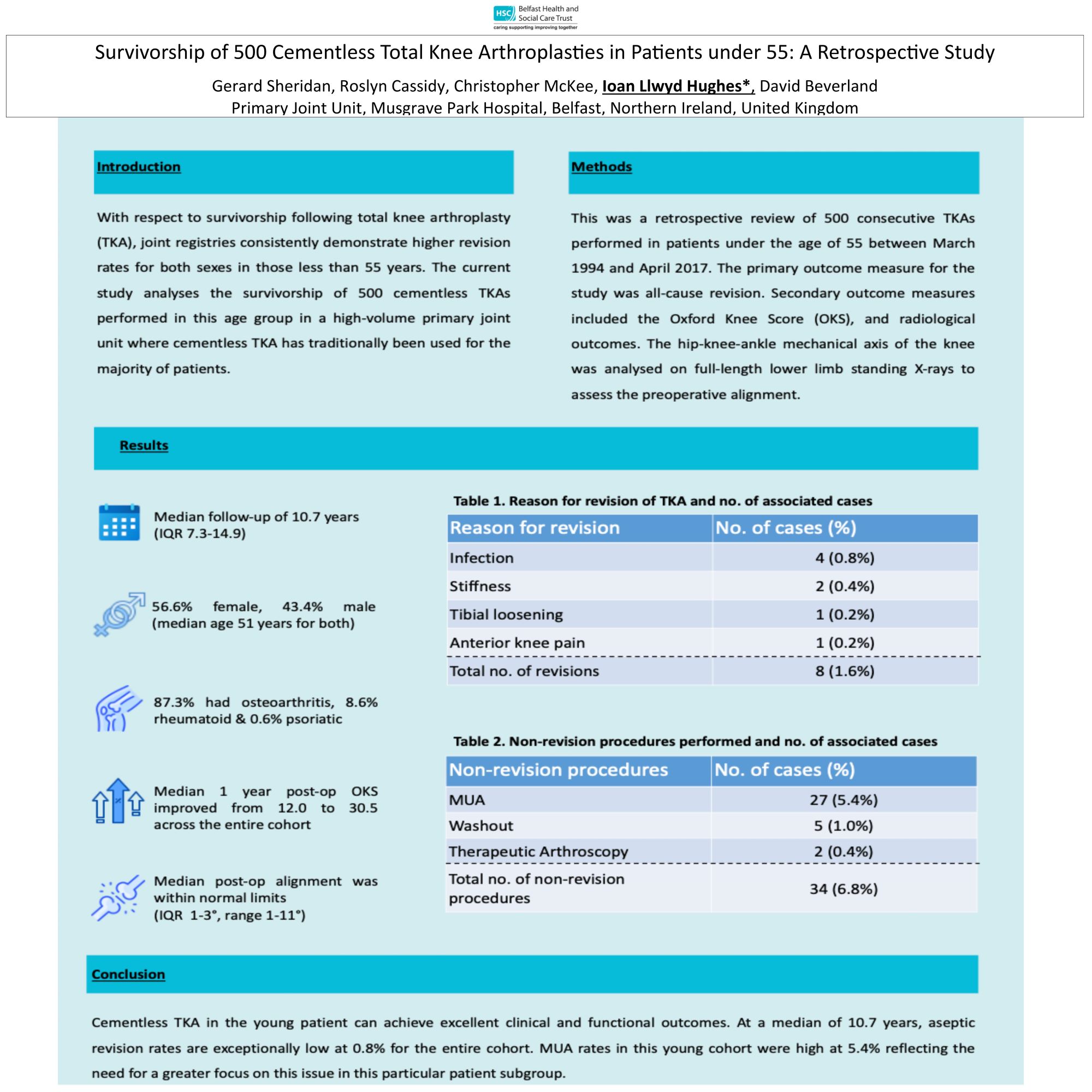
Gerard Sheridan1, Roslyn Cassidy2, christopher mckee2, Janet Hill1, David Beverland2, Ioan Hughes3
1Belfast, Belfast, United Kingdom. 2belfast, belfast, United Kingdom. 3Caerdydd, Caerdydd, United Kingdom
Abstract
Introduction: With respect to survivorship following total knee arthroplasty (TKA), joint registries consistently demonstrate higher revision rates for both sexes in those less than 55 years. The current study analyses the survivorship of 500 cementless TKAs performed in this age group in a high-volume primary joint unit where cementless TKA has traditionally been used for the majority of patients.
Methods: This was a retrospective review of 500 consecutive TKAs performed in patients under the age of 55 between March 1994 and April 2017. The primary outcome measure for the study was all-cause revision. Secondary outcome measures included clinical, functional and radiological outcomes.
Results: The all-cause revision rate was 1.6% (n=8) at a median of 55.7 months. Four were revised for infection, 2 for stiffness, 1 for aseptic loosening of the tibial component and 1 patella was resurfaced for anterior knee pain. The aseptic revision rate was 0.8% (n=4). Twenty-seven (5.4%) patients underwent a manipulation under anaesthetic (MUA). Including those who underwent MUA, 6.8% (n=34) underwent other non-revision procedures.
Conclusion: Survivorship in our unit in this young patient cohort was excellent with an aseptic revision rate of 0.8% at 59.7 months using a fully cementless construct. The MUA rate was higher than expected.
Keywords: TKA; Young; Cementless; Manipulation under anaesthetic
251 - Early Mechanical Failure of Hinge Knee Prothesis
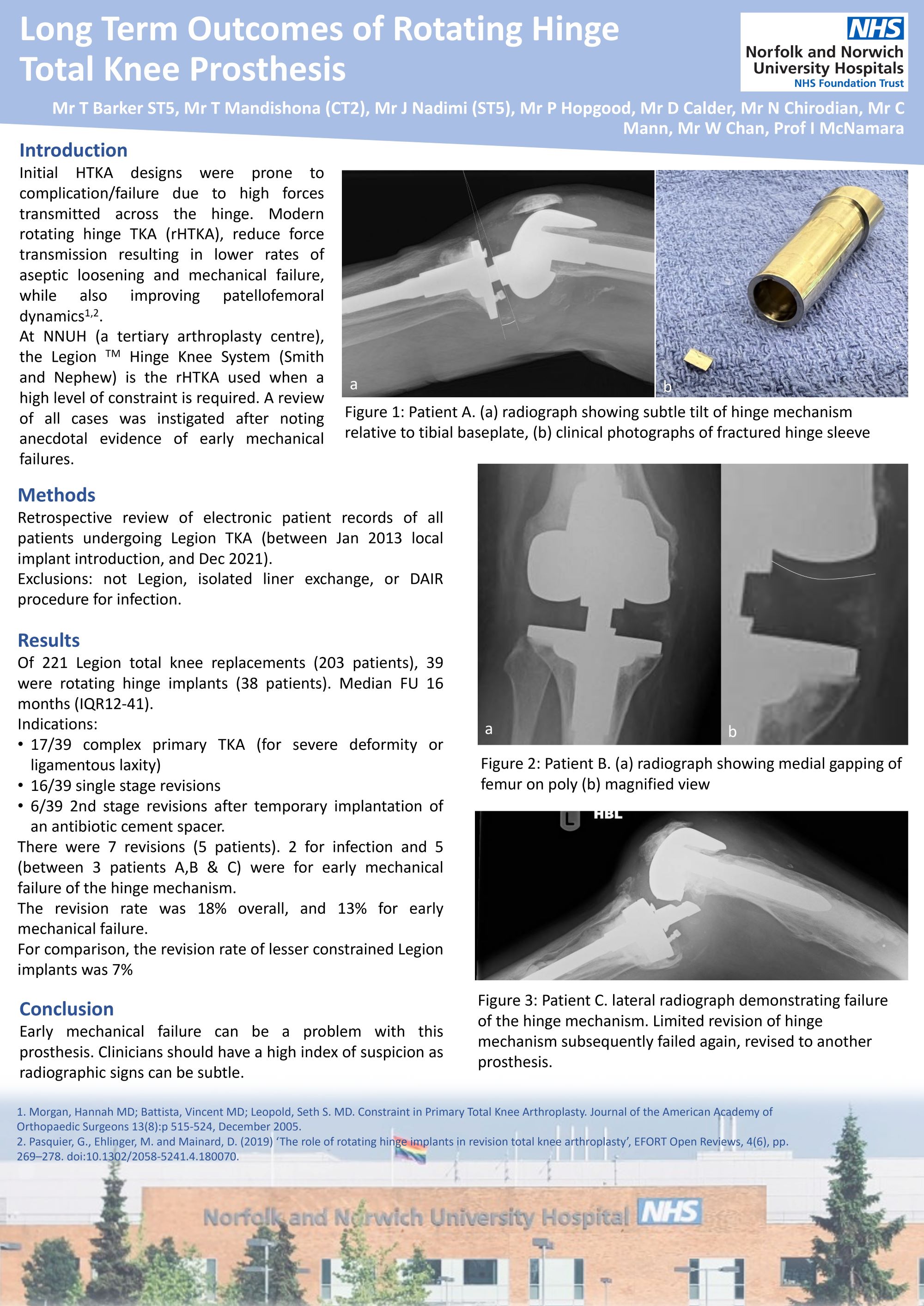
Thomas Barker1, Phil Hopgood2, David Calder2, Warwick Chan2, Nish Chirodian2, Iain McNamara2
1Colchester Hospital, Colchester, United Kingdom. 2Norfolk and Norwich Hospital, Norwich, United Kingdom
Abstract
Hinge TKAs can be an effective treatment for knee arthritis in the setting of collateral ligament instability/incompetence either in primary or revision settings, however they are associated with a high complication rate. The Legion knee system is used at our institution, and after anecdotal evidence of early mechanical failure, we identified a need to audit local outcomes for this implant.
Electronic records were interrogated for patients who had undergone revision TKA, or TKA using the Legion system between 2013-2022. Clinical notes and imaging were reviewed for indication and subsequent revision. Roentographic analysis was then performed on subsequently revised implants.
We identified 247 cases. After review of notes/imaging, there were 26 exclusions (first stage, other implant, DAIR, revision of polyethylene component) leaving 221 procedures in 203 patients with a median radiographic follow up of 24 months (IQR:13-47). Of 39 hinge implants (median FU 16 months, IQR:12-41), 17 were complex primary TKAs for arthritis with ligamentous instability/incompetence, 15 were single-stage revision TKAs with instability, and 6 were 2-stage revisions of infected TKAs. One underwent a DAIR procedure for infection (4 weeks post complex primary). Five were revised (12.8%), one for infection (24 months after 2 stage revision for infection) and 4 for fractured hinge mechanism at 7, 19, 58 and 74 months. Of 183 Legion knees implanted without a hinge (median FU 25 months, IQR:13-49), the revision rate was 7%.
Previously published works have identified a high risk of complications in hinged knee replacements. This study confirms this, and raises concerns over the strength of the hinge mechanism used in the Legion system. Clinicians should have a high index of suspicion for failure in these cases. This study in limited by the retrospective nature, and may be underreporting revision rate since only local records were reviewed
273 - Clinical outcomes following DAIR procedures for Hip and Knee PJI.
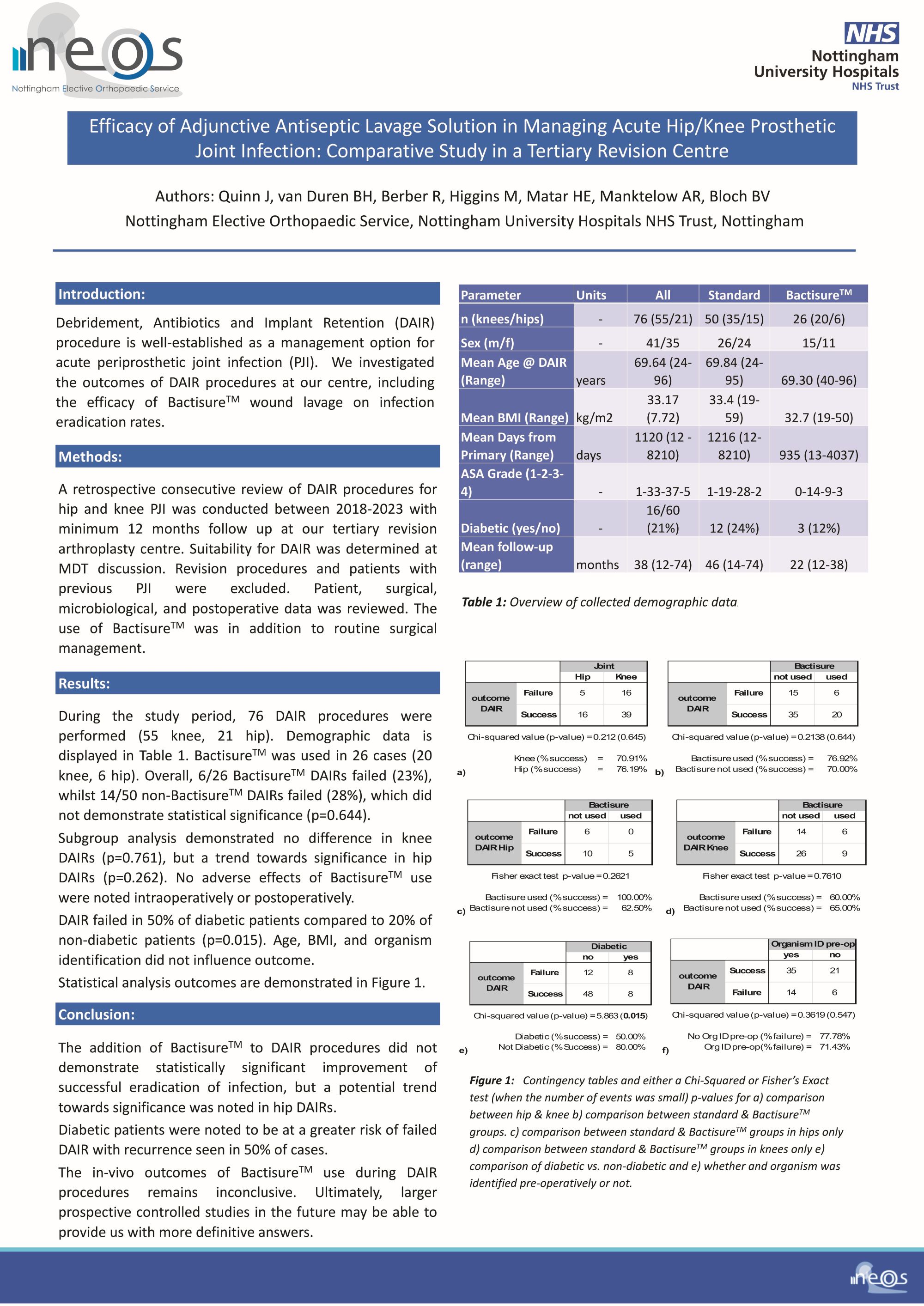
Jonathan Quinn, Bernard Van Duren, Ben Bloch
Nottingham University Hospital, Nottingham, United Kingdom
Abstract
Background: Debridement, Antibiotics and Implant Retention (DAIR) procedure is well established as a management option for acute periprosthetic joint infection (PJI). We investigated the outcomes of DAIR procedures at our centre, including the efficacy of BactisureTM wound lavage on infection eradication rates.
Methods: A retrospective review of DAIR procedures for hip and knee PJI was conducted. Inclusion criteria: patients from 2018-2023 inclusive, receiving care by subspecialist revision arthroplasty surgeons at a major revision unit (NUH). Suitability for DAIR was determined at MDT discussion. Revision procedures and patients with previous PJI were excluded. Patient, surgical, microbiological and postoperative data (minimum 6 months) was obtained and analysed. The use of BactisureTM was in addition to routine surgical management, including copious lavage and chlorhexidine wash following debridement and removal of modular components.
Results: During the study period, 76 DAIR procedures were performed (55 knee, 21 hip). Bactisure was used in 26 cases (20 knee, 6 hip). Overall, 6/26 bactisure DAIRs failed (23%), whilst 14/50 non-bactisure DAIRs failed (28%), which did not demonstrate statistical significance (p=0.644). Subgroup analysis demonstrated no difference in knee DAIRs (p=0.761), but a trend towards significance in hip DAIRs (p=0.262). No adverse effects of Bactisure use were noted intraoperatively or postoperatively. DAIR failed in 50% of diabetic patients compared to 20% of non-diabetic patients (p=0.015). Age, BMI, and organism identification did not influence outcome.
Conclusions: The addition of Bactisure to DAIR procedures did not demonstrate statistically significant improvement of successful eradication of infection, but a trend towards significance was noted in hip DAIRs. Diabetic patients failed DAIR in 50% of cases.
Implications: The in-vivo outcomes of Bactisure use during DAIR procedures remains unclear.
Disclosure: The institution receives financial support from Zimmer.
274 - Five-year outcomes of a cementless, rotating-platform total knee replacement performed with a gap-balance technique
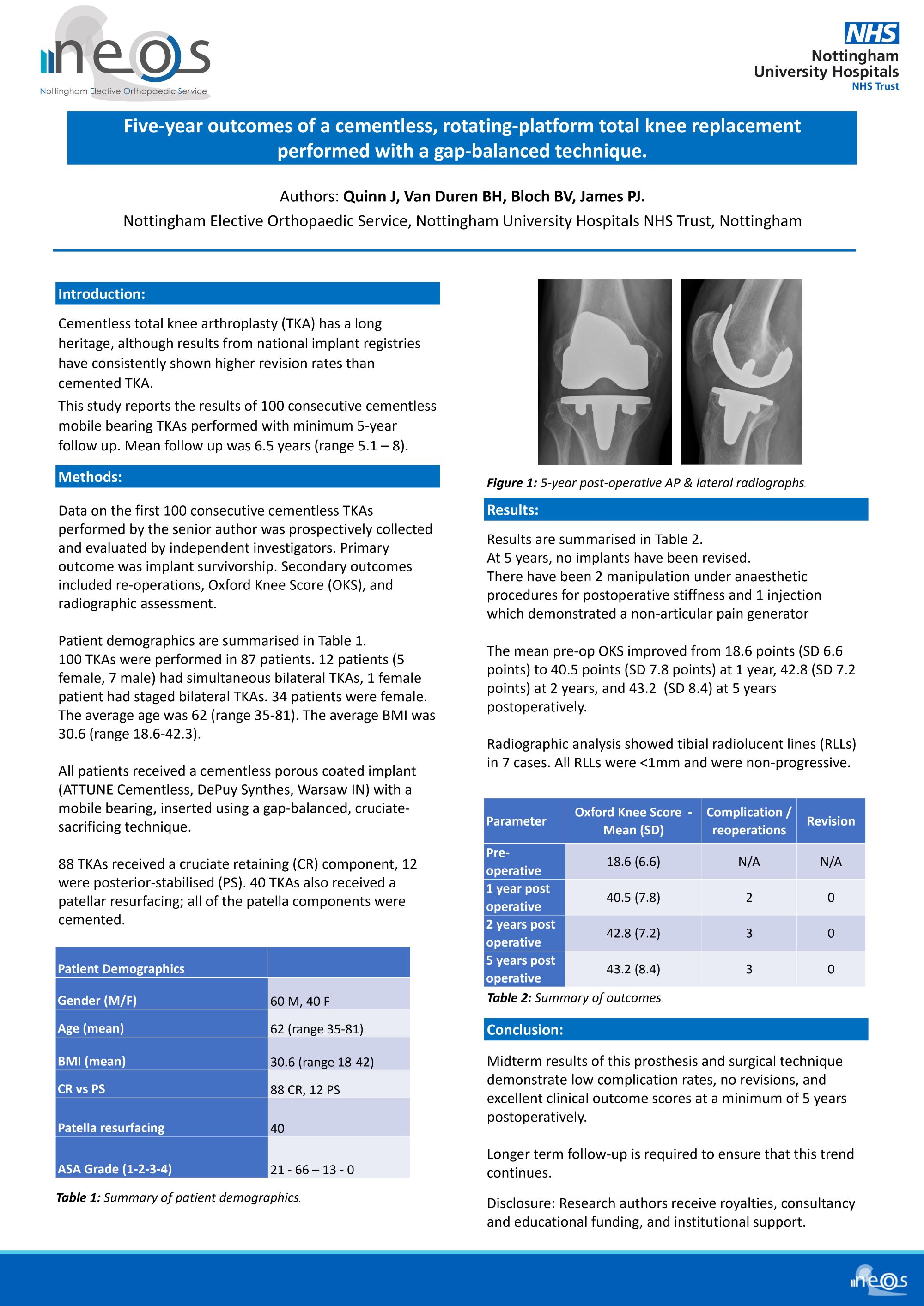
Jonathan Quinn, Bernard Van Duren, Ben Bloch, Peter James
Nottingham University Hospital, Nottingham, United Kingdom
Abstract
Background: Cementless total knee arthroplasty (TKA) has a long heritage, although results from national implant registries have consistently shown higher revision rates than cemented TKA. This study reports the results of 100 consecutive cementless mobile bearing TKAs performed with minimum 5-year follow up. Mean follow up was 6.5 years (range 5.1 – 8).
Methods: Data on the first 100 consecutive cementless TKAs performed by the senior author was prospectively collected and evaluated by independent investigators. Primary outcome was implant survivorship. Secondary outcomes included re-operations, Oxford Knee Score (OKS), and radiographic assessment. 100 TKAs were performed in 87 patients. 12 patients (5 female, 7 male) had simultaneous bilateral TKAs, 1 female patient had staged bilateral TKAs. 34 patients were female. The average age was 62 (range 35-81). The average BMI was 30.6 (range 18.6-42.3). All patients received a cementless porous coated implant with a mobile bearing, inserted using a gap-balanced, cruciate-sacrificing technique. 88 TKAs received a cruciate retaining (CR) component, 12 were posterior-stabilised (PS). 40 TKAs also received a patellar resurfacing; the all patella components were cemented.
Results: At 5 years, no implants have been revised. There have been 2 manipulation procedures for postoperative stiffness, 1 injection demonstrating non-articular pain generator. 1 patient is deceased. The mean pre-op OKS improved from 18.6 points to 40.5 points at 1 year and 42.8 at 5 years. Radiographic analysis showed tibial radiolucent lines (RLLs) in 7 cases. All RLLs were <1mm and were non-progressive.
Conclusion: Midterm results of this prosthesis and technique demonstrate low complication rates, no revisions, and excellent clinical scores.
Implications: This technique and prosthesis demonstrates reliable midterm results.
Disclosure: Research authors receive royalties, consultancy and educational funding, institutional support.
295 - Fifteen Year Results of Cementless Medial Oxford Unicompartmental Knee Replacement
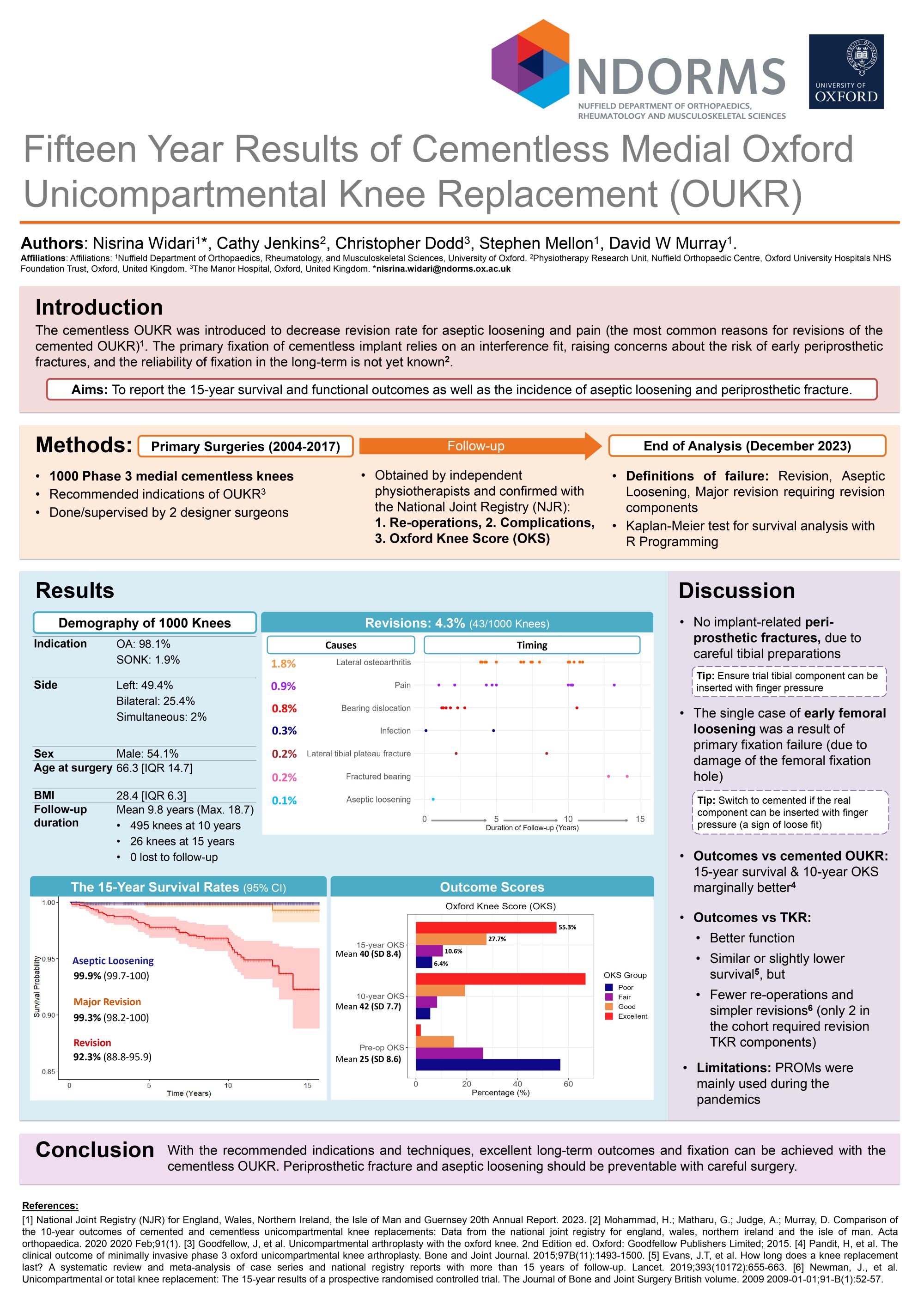
Nisrina Widari1, Cathy Jenkins2, Christopher Dodd3, Stephen Mellon1, David Murray1
1Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), Oxford, United Kingdom. 2Physiotherapy Research Unit (PRU), Nuffield Orthopaedic Centre, Oxford, United Kingdom. 3The Manor Hospital, Oxford, United Kingdom
Abstract
Background: The cementless Oxford Unicompartmental Knee Replacement (OUKR) was introduced to minimise the risk of aseptic loosening. There is a concern that the fixation may fail in the long term or that the interference fit of the cementless tibial keel may cause early periprosthetic fractures. The aim is to determine the 15-year survival and functional outcome as well as the incidence of aseptic loosening and periprosthetic fracture.
Methods: 1000 consecutive cementless OUKR were implanted between 2004 and 2017 for the recommended indications of antero-medial osteoarthritis(981) or avascular necrosis(19) and independently followed-up. Mean follow-up was 10 years (maximum 19-years). Survival was assessed using various endpoints. The primary outcome measure was the Oxford Knee Score (OKS, range 0–48).
Results: There were 52(5.2%) re-operations at a mean of 6-years (SD4.3). 43(4.3%) of these were revisions. The most common causes for revision were lateral compartment arthritis (1.8%), pain (0.9%), bearing dislocation (0.8%) and infection (0.3%). There was one aseptic loosening, which was a femoral component within the first year. There were two lateral plateau fractures following trauma. The 15-year survival for revision was 92%(CI88.8-95.9), for major revision needing revision components was 99%(CI98.2-100) and for all re-operations was 91%(CI87.6-94.9). The mean OKS was 42(SD7.7) at 10-years and 40(SD8.4) at 15-years. Failure rate did not increase with age at surgery (Mantel log-rank test, p=0.9).
Conclusion: Cementless OUKR has excellent long-term functional outcomes and survival when the recommended indications and techniques are used. Long-term fixation was reliably achieved with only a single case (0.1%) of loosening. This was a failure of primary fixation of a femoral component due to damage to the fixation hole at surgery. There were no early periprosthetic fractures.
Disclosure: Personal and Institutional Support has been provided to one or more authors by Zimmer Biomet.
300 - Early Subsidence Associated with Tilting of The Tibial Component in Cementless Oxford Unicompartmental Knee Replacement
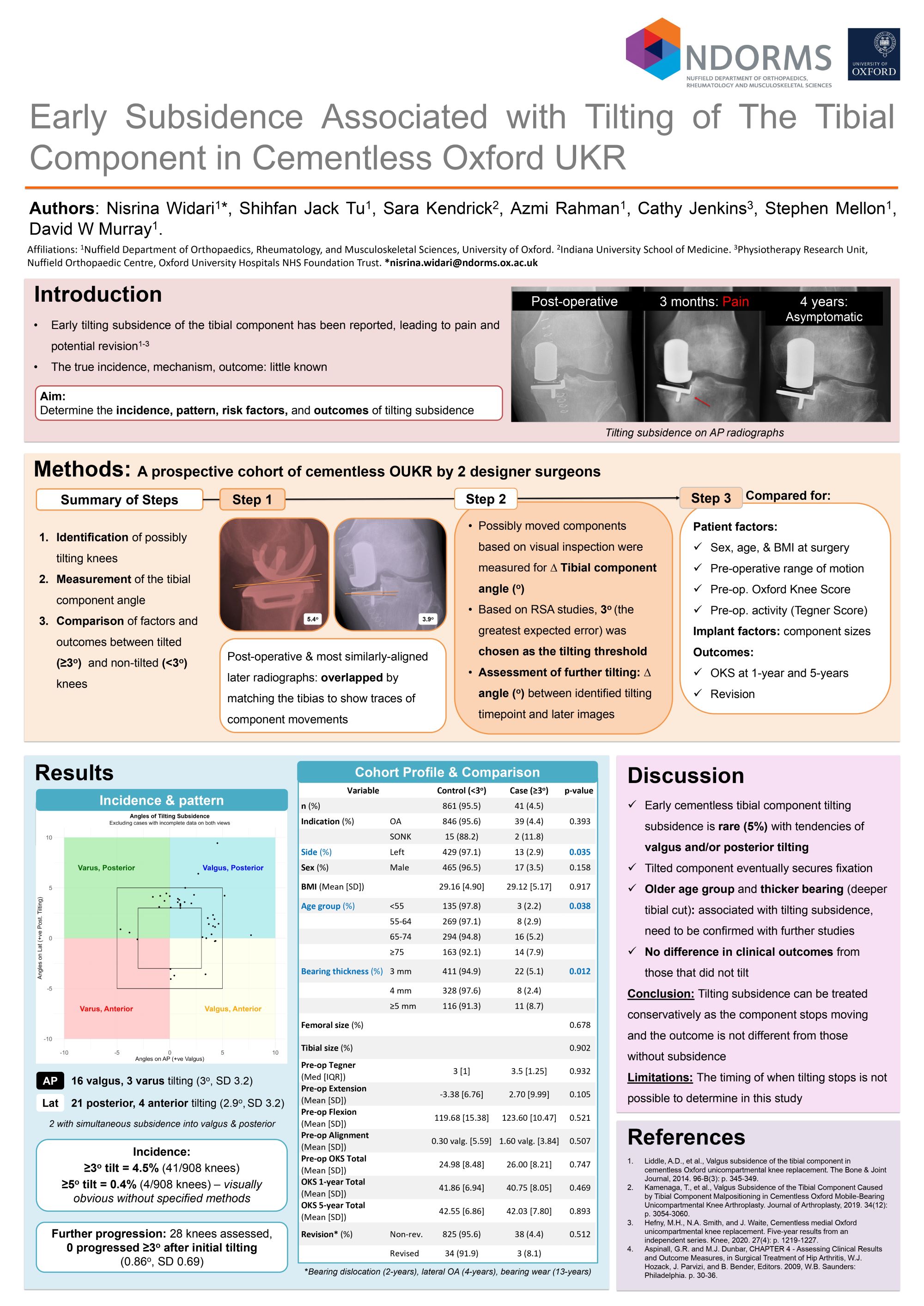
Nisrina Widari1, Jack Tu1, Sara Kendrick2, Azmi Rahman1, Giuseppe Diodato Santoro3, Xiaoyi Min1, Cathy Jenkins4, Stephen Mellon1, David Murray1
1Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS), Oxford, United Kingdom. 2Indiana University School of Medicine, Indianapolis, USA. 3Universitá degli studi di Milano, Scuola di specializzazione in Ortopedia e Traumatologia, Milan, Italy. 4Physiotherapy Research Unit, Nuffield Orthopaedic Centre, Oxford, United Kingdom
Abstract
Introduction: Tilting subsidence of the tibial component is a poorly understood complication of the cementless Oxford Partial Knee. The aim is to determine the incidence, pattern, risk factors, and outcome of tilting.
Methods: 438 cementless OUKR between 2004-2017 with accurately aligned post-operative and subsequent antero-posterior(AP) and lateral radiographs were identified. The tibias of x-rays pairs were overlapped and changes in component angles were measured. To determine the accuracy, radiographs of 15 patients of radiostereometric analysis (RSA) were measured in the same manner. Identified cases with tilting were optimally matched based on several factors with a 1:1 ratio with a group of control with <2o tilt. Several radiographic features on the post-operative images were measured on FIJI and compared between the two groups.
Results: Based on the RSA data 3o tilt, the greatest expected error, was defined as the tilting threshold. Six AP and 13 lateral radiographs had tilting subsidence (4.3%). All tilted into valgus (4.4oSD1.7) or tilted posteriorly (3.9oSD1). After the initial tilting no knees progressed further. Between the tilted and non-tilted groups, there were no significant differences in patient, implant, and surgeon factors, 1 year Oxford Knee Score (45 IQR9 v45 IQR12) and revision (10.5%v2.9%). In comparison to the matched control group, tilted cases had greater degrees of mediolateral (-0.6v-0.2mm) and posterior (-0.1v0.4mm) underhanging, deeper vertical overcut (0.7v0.2mm), more externally rotated femoral component relative to the tibial component (5.4v4.9o), and more medial tibial cut relative to the medial tibial spine (1.6v2 mm). However, these differences were not statistically significant.
Conclusion: Tilting subsidence is rare(4%) and has a tendency into valgus or posteriorly. If treated conservatively, the components stop tilting with no difference in clinical outcomes from those that did not tilt. Undersized components, deep vertical overcut, and component malpositioning could potentially play a role in tilting subsidence.
381 - Metal Release in Contemporary Primary Total Knee Replacements: An Under-Recognised Clinical Issue
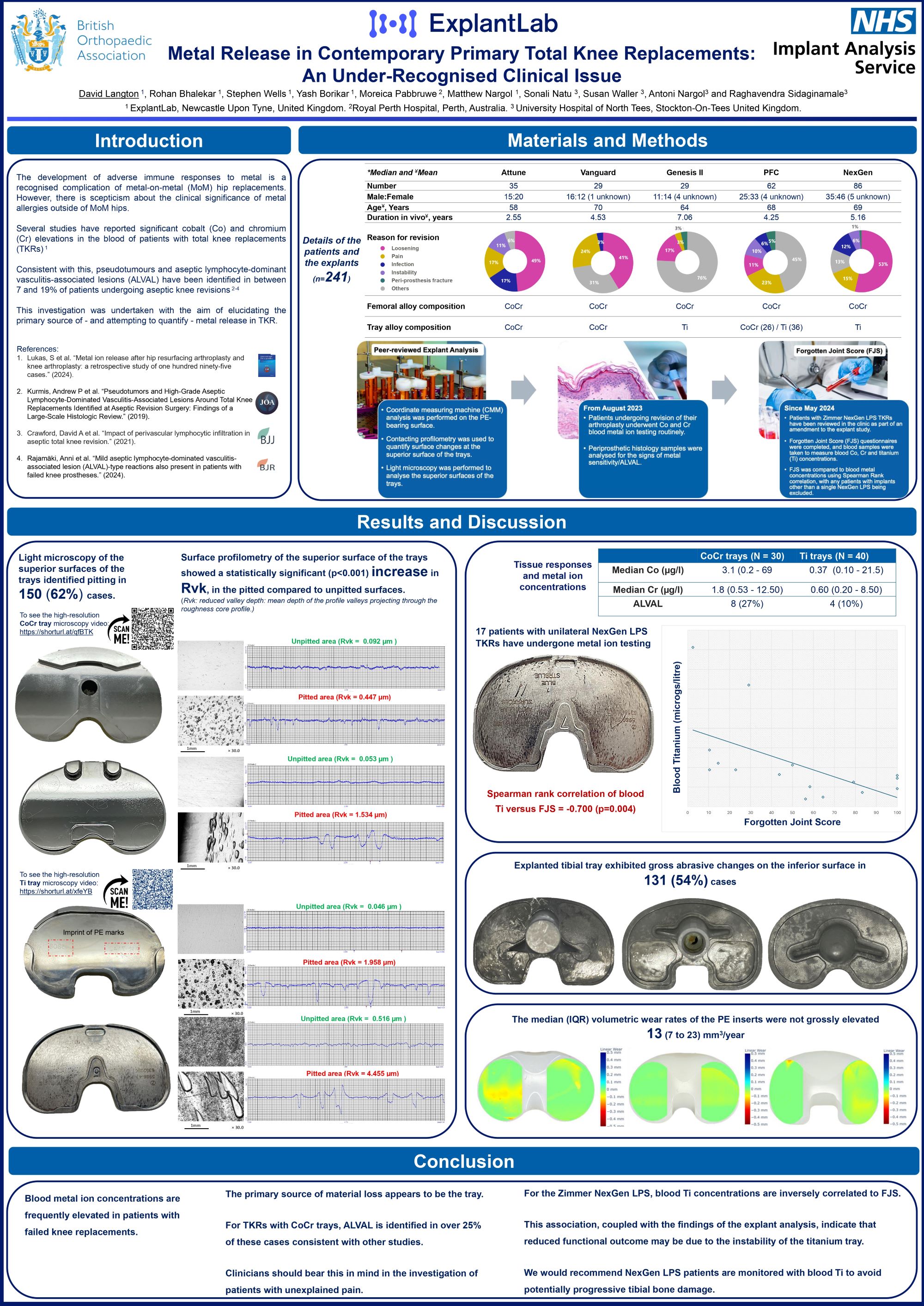
David Langton1, Rohan Bhalekar1, Stephen Wells1, Moreica Pabbruwe2, Matthew Nargol1, Sonali Natu3, Susan Waller3, Raghavendra Sidaginamale3
1ExplantLab, Newcastle Upon Tyne, United Kingdom. 2Royal Perth Hospital, Perth, Australia. 3University Hospital of North Tees, Stockton-On-Tees, United Kingdom
Abstract
Background: While adverse reactions to metal debris (ARMD) have been extensively documented in metal-on-metal hips, ARMD in total knee replacements(TKRs) is insufficiently acknowledged. Studies have reported elevated blood cobalt (Co) and chromium (Cr) concentrations in patients who have undergone TKRs. Histological examination of tissue samples from patients with failed TKR has revealed evidence of metal sensitivity/ALVAL in up to 44%of cases. This research aims to identify the source of metal release in TKRs.
Methods: A total of 241 explanted fixed-bearing TKRs (Attune, Genesis II, NexGen, PFC, and Vanguard) were analysed using peer-reviewed techniques. Coordinate-measuring machines were used to quantify the changes in the wear and deformation of PEs, while visual and light microscopy were employed to examine Ti/CoCr trays. Surface-roughness measurements (Rvk) were utilised to quantitatively evaluate the impact of pitting on tray surfaces.
Results: Microscopic examination of the superior surface exhibited pitting on 150(62%) trays, with a statistically significant increase in Rvk(p<0.05) for each design, indicating material removal from pits. Additionally,120(50%) trays exhibited polishing on the inferior surface, indicative of abrasive wear. Median (IQR) wear rate for PE bearing surfaces was measured at 14(6to20)mm³/year. In 40 patients, median(range)Co and Cr concentrations were 2.5µg/l(0.2–69.4) and 1.7µg/l(0.5-12.5),respectively. Of the tissue samples analysed from 30 patients, 6 exhibited a"mild" ALVAL infiltrate. All corresponding“ALVAL” explants were found to be pitted and/or show evidence of loosening of the tray. Multiple-regression-modelling showed that tibial insert backside deformation was significantly associated with Rvk of the superior surface of the trays with central locking mechanism, i.e. Vanguard(p=0.046), Attune(p=0.008)and NexGen(p=0.021).
Conclusion: This study provides further evidence that the generation of metal particles was predominantly from the metal tray, which may explain elevated metal ions after TKRs.
477 - Clinical Application of Limb Dimension Index Allows for Better Identification of Patients at Higher Risk of Longer Operating Times and In-Patient Stay
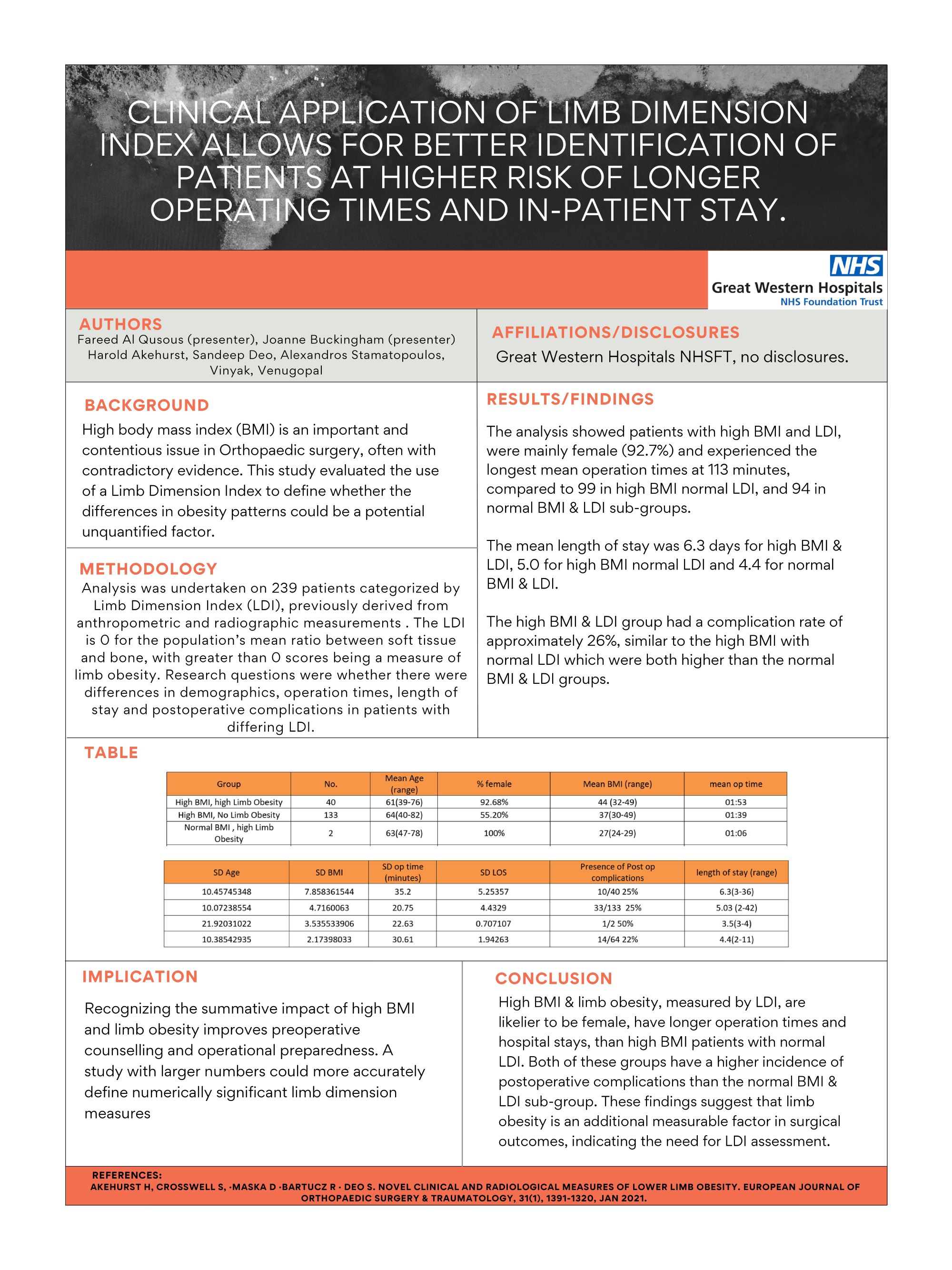
Harold Akehurst1, Sunny Deo2, Alexandros Stamatopoulos2, Fareed Al Qusous2, Joanne Buckingham2
1Gloucestershire Hospital (NHS), Gloucestershire, United Kingdom. 2Great Western Hospital (NHS), Swindon, United Kingdom
Abstract
Background: High body mass index (BMI) is a key issue in Orthopaedic surgery. Limb obesity has been less extensively studied. This research evaluates the use of a Limb Dimension Index on surgical procedures independent of BMI.
Methods: Analysis was undertaken on 238 patients categorized by Limb Dimension Index (LDI), previously derived from anthropometric and radiographic measurements . The LDI is 0 for the population’s mean ratio between soft tissue and bone, with greater than 0 scores being a measure of limb obesity. Research questions were whether there were differences in demographics, operation times, length of stay and postoperative complications in patients with differing LDI.
Results: The analysis showed patients with high BMI and LDI, were mainly female (92.7%) and experienced the longest mean operation times at 113 minutes, compared to 99 in high BMI normal LDI, and 94 in normal BMI & LDI sub-groups. The mean length of stay was 6.3 days for high BMI & LDI, 5.0 for high BMI normal LDI and 4.4 for normal BMI & LDI. The high BMI & LDI group had a complication rate of approximately 26%, similar to the high BMI with normal LDI which were both higher than the normal BMI & LDI groups.
Conclusion: High BMI & limb obesity, measured by LDI, are likelier to be female, have longer operation times and hospital stays, than high BMI patients with normal LDI. Both of these groups have a higher incidence of postoperative complications than the normal BMI & LDI sub-group. These findings suggest that limb obesity is an additional measurable factor in surgical outcomes, indicating the need for LDI assessment.
Implication: Recognizing the summative impact of high BMI and limb obesity improves preoperative counselling and operational preparedness. Further studies are recommended to validate these observations and refine surgical protocols accordingly.
507 - Does change in Coronal Plane Alignment of the Knee classification following Total Knee Arthroplasty influence patient-reported outcomes and survivorship?
A review of 1062 cases with 10 years follow-up
Ghaith Al-Abbasi, David Wallace, Fahd Mahmood, Nick Ohly, Jon Clarke
Golden Jubilee University National Hospital, Clydebank, United Kingdom
Abstract
Background: Alignment strategy in total knee arthroplasty (TKA) remains controversial. Restoration of native Coronal Plane Alignment of the Knee (CPAK) phenotype is a strategy suggested to achieve optimum patient satisfaction. The aim of this study was to investigate the influence of changes in CPAK classification on patient-reported outcome measures (PROMs) and survivorship in a large cohort of manual mechanically aligned (MA) cemented TKAs.
Methodology: This was a retrospective analysis of 1062 consecutive cemented cruciate retaining (CR) single radius TKAs using an MA philosophy at a single institution. Pre- and post-operative hip-knee-ankle radiographs were classified using the CPAK classification. Oxford Knee Score (OKS) and patient satisfaction (4-point Likert scale) were collected prospectively. Implant survival data was obtained from our national arthroplasty database and cross-referenced with local data. We compared the outcomes of patients who maintained or changed their CPAK classification following TKA. Satisfaction was analysed using chi-square test, and OKS was analysed using Mann-Whitney test.
Results: Pre-operatively, most patients were CPAK type-I (38.8%). 85.5% of patients changed their CPAK type post-operatively, with CPAK type-V observed in 41.2% of these. Significantly better satisfaction (p=0.033) and OKS (p=0.021) were observed at one-year follow-up in patients who changed CPAK type, although the difference was below OKS minimally important clinical difference. There was no difference in satisfaction (p=0.73) and OKS (p=0.26) at one year between CPAK V and non-V classifications. Post-operative CPAK type had no correlation with satisfaction and OKS. 12 TKAs (1.1%) were revised within 10 years (3 septic).
Conclusion: In this large cohort of MA-TKA, excellent survivorship was observed at 10 years, with no demonstrable difference in outcome related to the final CPAK phenotype or change in phenotype.
Implication: A mechanical alignment TKA philosophy (CPAK type-V target) appears to be a satisfactory TKA technique, regardless of pre- or post-operative alignment category.
516 - Sustained Efficacy of nSTRIDE® Therapy in the Treatment of Knee Osteoarthritis: A Longitudinal Analysis of WOMAC and OKS Outcomes
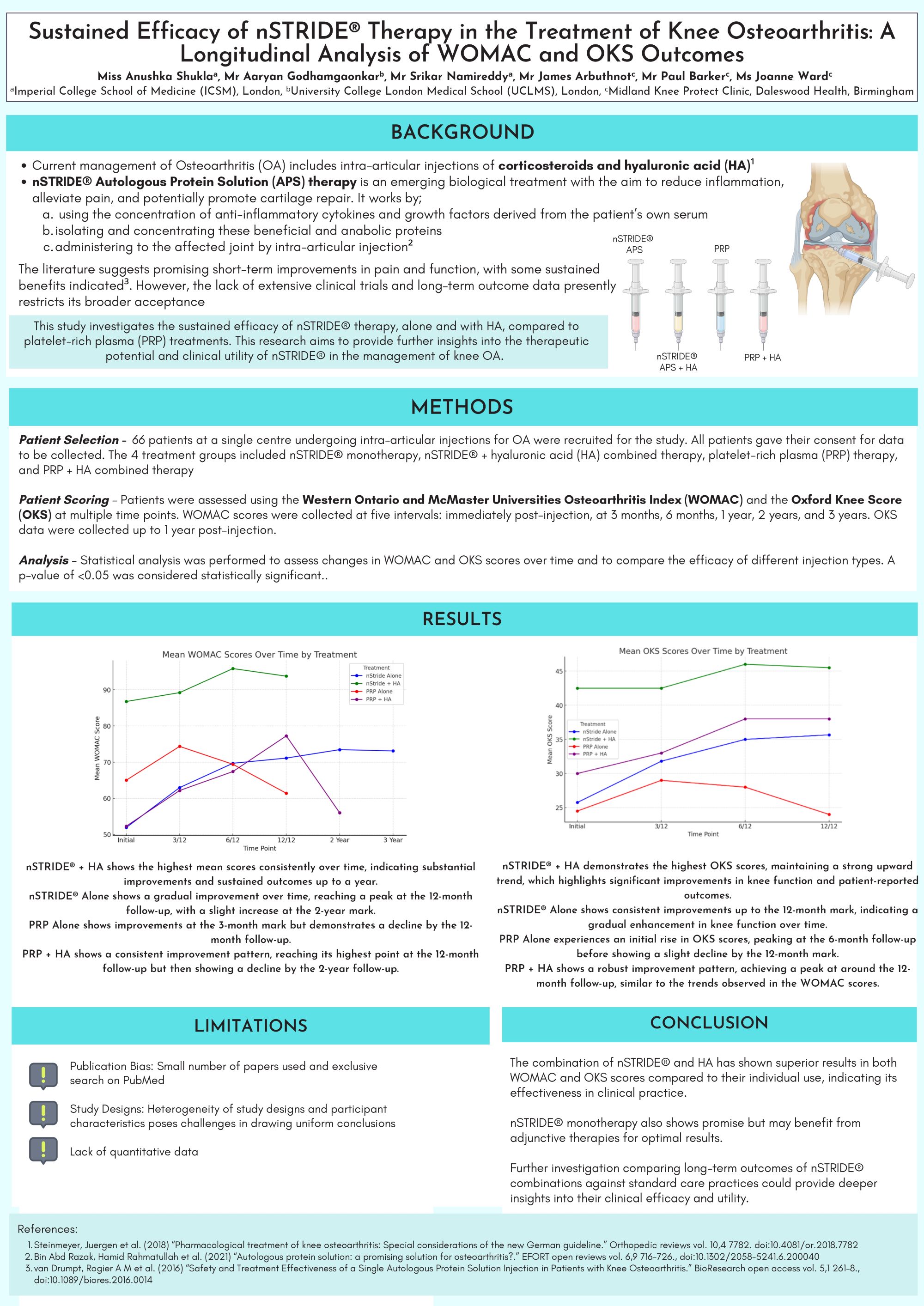
Aaryan Godhamgaonkar1, Anushka Shukla2, Srikar Namireddy2, James Arbuthnot3, Paul Barker3, Joanne Ward4
1University College London Medical School (UCLMS), London, United Kingdom. 2Imperial College School of Medicine (ICSM), London, United Kingdom. 3University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom. 4Daleswood Health Clinic, Solihull, Birmingham, United Kingdom
Abstract
Background: nSTRIDE® therapy, a novel approach for knee osteoarthritis (OA), involves autologous blood processing to concentrate anti-inflammatory cytokines and growth factors. Administered via intra-articular injection, it aims to alleviate pain and promote cartilage repair. Clinically, it serves as both supplementary and standalone therapy, offering promising outcomes in improving pain and function in knee OA patients. This study aims to quantify the efficacy of nSTRIDE® therapy in symptomatic relief of knee OA.
Methods: 66 patients with knee OA underwent various treatments as part of this retrospective cohort study. The 4 treatment groups included nSTRIDE® monotherapy, nSTRIDE® + hyaluronic acid (HA) combined therapy, platelet-rich plasma (PRP) therapy, and PRP + HA combined therapy. Follow-up assessments utilised WOMAC and Oxford Knee Scores (OKS) for up to 3 years post-treatment. Statistical analysis was performed using the 'R' software programme.
Results: In this study, nSTRIDE® + HA treatment demonstrated the most sustained improvement, with mean WOMAC scores rising from 50 to 90 at 12 months and stabilising through 36 months. nSTRIDE® alone showed an increase from 60 to 82 from baseline to 24 months. PRP Alone and PRP + HA both presented declines in WOMAC scores after initial improvements at 3 and 12 months, respectively. Similar trends were observed in OKS scores, with nSTRIDE® + HA showing continuous improvement, while PRP treatments peaked early and then diminished.
Conclusion: The combination of nSTRIDE® and HA has shown superior results in both WOMAC and OKS scores compared to their individual use, indicating its effectiveness in clinical practice. nSTRIDE® monotherapy also shows promise but may benefit from adjunctive therapies for optimal results. Further investigation comparing long-term outcomes of nSTRIDE® combinations against standard care practices could provide deeper insights into their clinical efficacy and utility.
542 - Is return to driving 6 weeks post Total Knee Replacement feasible? A Tertiary Centre experience
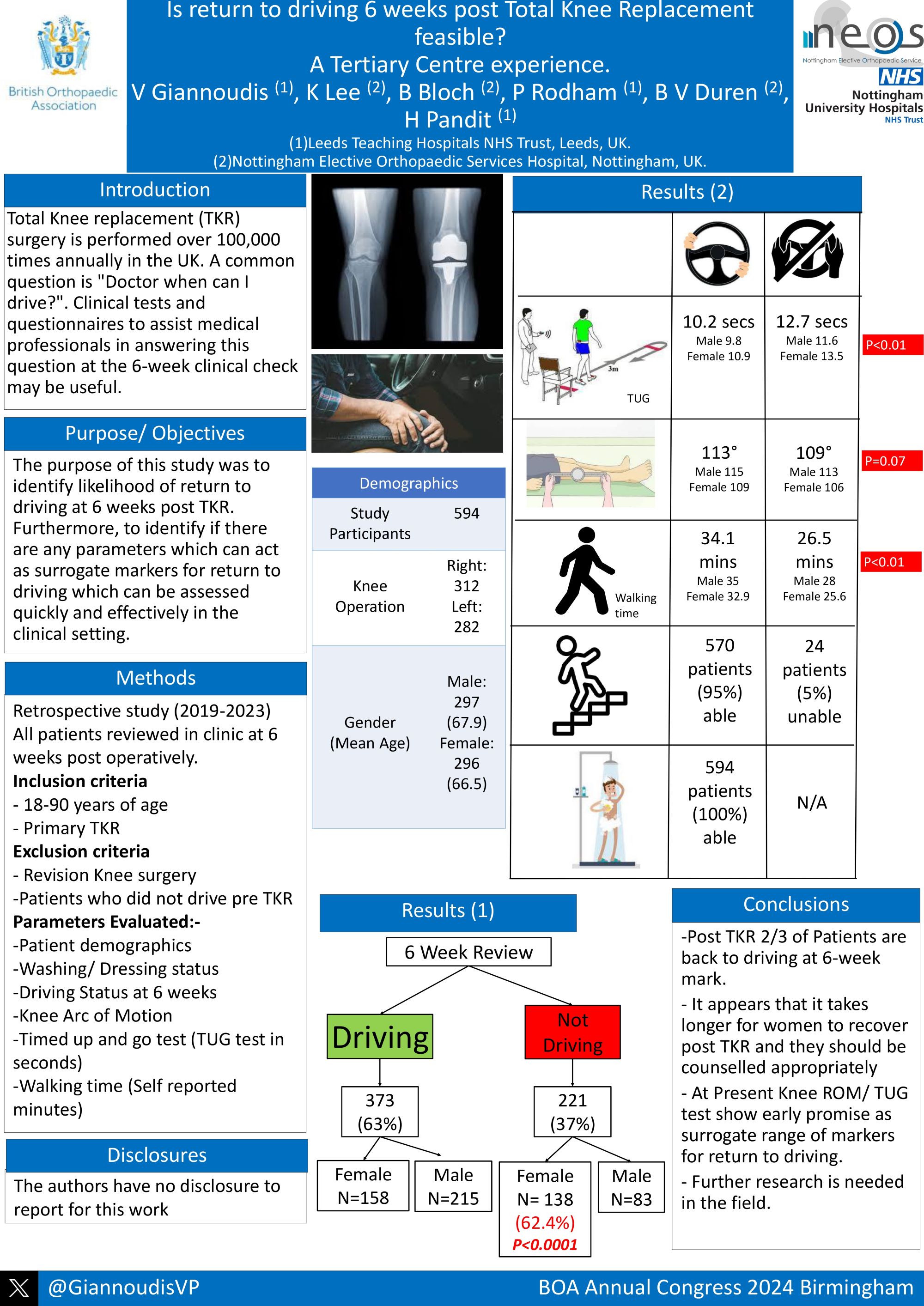
Vasileios Giannoudis1, Katie Lee2, Benjamin Bloch2, Paul Rodham1, Bernard Van Duren2, Hemant Pandit3
1Leeds General Infirmary, Leeds, United Kingdom. 2Nottingham Elective Orthopaedic Services Hospital, Nottingham, United Kingdom. 3Chapel Allerton Hospital, Leeds, United Kingdom
Abstract
Background: Total Knee replacement (TKR) surgery is a commonly undertaken procedure with over 100,000 performed annually in the UK. A common question following TKR is "Doctor when can I drive?". In the UK, the onus is on licence-holder to notify DVLA, however, healthcare professionals are expected to provide advice. Clinical tests to assist medical professionals to give advice to patients at 6-weeks may be useful for decision-making. The purpose of this study was to identify likelihood of driving return at 6 weeks post TKR and to identify clinical markers which could predict safe return to driving.
Methods: This single centre study was conducted between 01/01/2019- 14/07/2023. As part of the post operative TKR protocol, patients were reviewed at 6 weeks. Data collected included: patient demographics; Washing/ Dressing status; driving; Arc of Motion, timed up and go test, and walking time. Descriptive statistics were used alongside t-Tests.
Results: 594 participants were included (312 Right, 282 Left). From these there were 297 males (mean age 67.9) and 296 females (mean age 66.5). At 6-weeks 373 patients (62.8%) were driving, and 221 were not (n=138 female, 62.4%) p<0.00001. Walking time in those driving and not driving (DND) was reviewed with a mean of 34.1 and 26.5 minutes respectively (p=0.000000048). TUG tests were slower in the DND group 12.7 secs vs 10.2 secs, p=0.000000089) these were also seen when comparing males (Drive 9.8 secs vs DND 11.6 secs, p=0.001) and females (Drive 10.9 secs vs DND 13.5 secs, p=0.0005). Knee ROM arc showed small differences between males and females (115 vs 109, p=0.07) and DND (113 vs 106, p=0.23).
Conclusions/ Findings: Following TKR most patients should be driving at 6-weeks, though it may take women longer to return. At present knee ROM and TUG test show promise as surrogate markers for return to driving.
723 - Re-revision total knee arthroplasty – the effect of time from primary to first revision. A study of 4501 patients from the Scottish Arthroplasty Project.
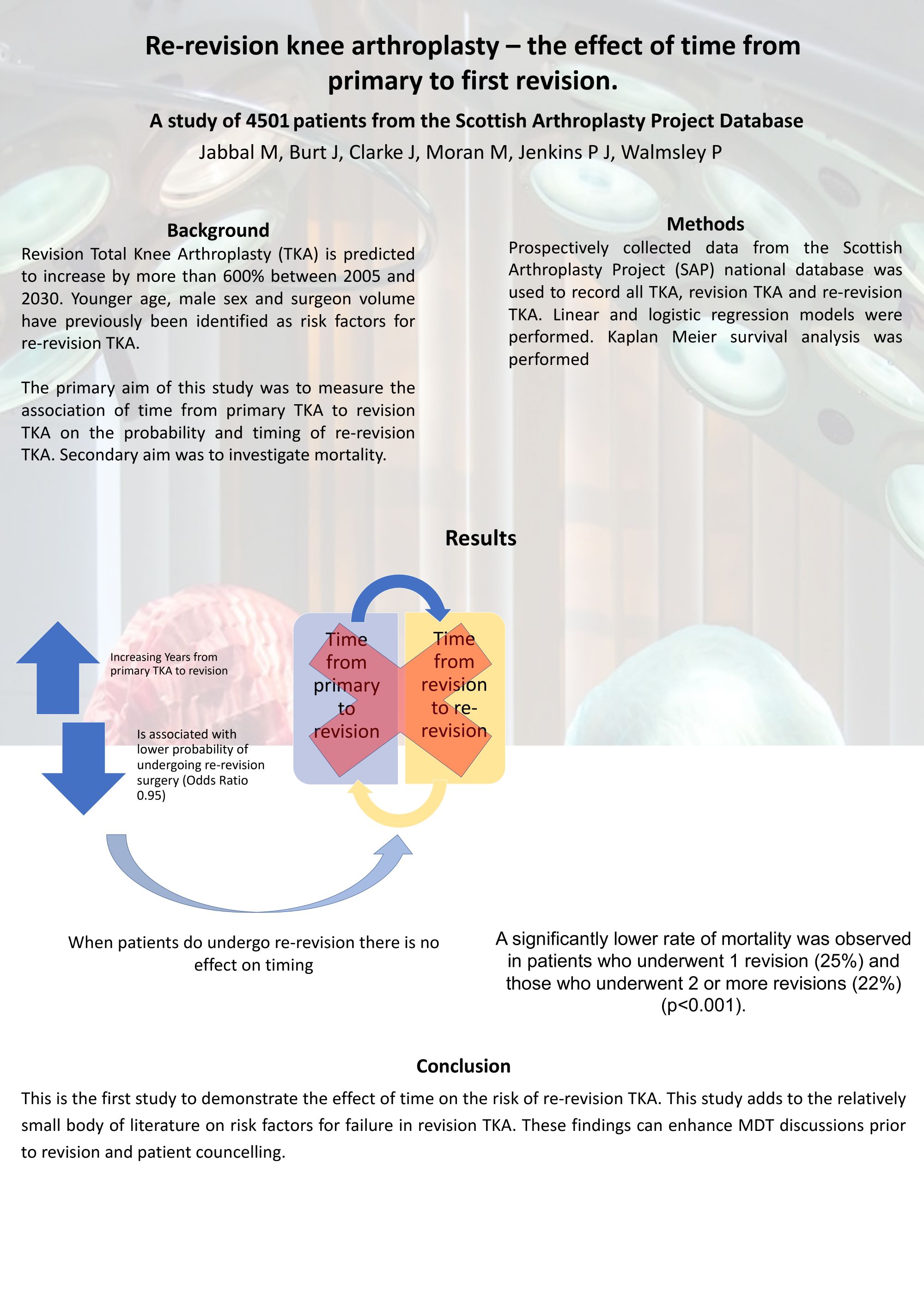
Monu Jabbal1, Justine Burt2, Jon Clarke2, Matthew Moran1, Paul Jenkins3, Phil Walmsley4
1Edinburgh Orthopaedics, Edinburgh, United Kingdom. 2Golden Jubilee National Hospital, Glasgow, United Kingdom. 3Glasgow Royal Infirmary, Glasgow, United Kingdom. 4Fife National Treatment Centre, Kirkcaldy, United Kingdom
Abstract
Background: The primary aim of this study was to measure the effect of time from primary TKA to revision TKA on the risk and timing of re-revision surgery. Secondary aims were to investigate effect of re-revision on mortality and report long term implant survivorship.
Methods: This was an analysis of the Scottish Arthroplasty Project (SAP) data set. 4501 patients from the period 2000 to 2019 were studied. Cox proportional hazard regression was used to estimate relative revision risk over time. Of cases undergoing re-revision, linear regression was used to determine any relationship of time from primary. Kaplan-Meier survival curves were plotted to determine mortality and implant survivorship.
Results: Increasing the time between primary TKA and 1st revision TKA was significantly associated with a reduced risk of subsequent re-revision of (2% per year, p=0.017). Similarly increasing age at primary surgery decreased the subsequent risk (3%/year). Male gender increased risk by 35% (p<0.001). When re-revision did occur, there was no significant association between the time from primary to 1st revision and the time from 1st-revision to re-revision (p>0.05). Patients who had their revision TKA in the period 2010-2019 had a shorter time to re-revision, as did patients with increasing age (p<0.001). A significantly lower rate of mortality was observed in patients who underwent 1 revision (25%) and those who underwent 2 or more revisions (22%) (p<0.001).
Conclusion: This is the first study to demonstrate time from primary TKA to 1st revision TKA having a significant effect on risk of re-revision TKA, but no association with when it occurs. The study describes long term mortality and survivorship from a national dataset and adds to the relatively small body of knowledge on risk factors for failure and long term survivorship of revision TKA.
Hip - Poster Abstracts
814 - Anterior acetabular fracture repair via the Modified Stoppa approach:
Is there a soft tissue safe zone that can be identified intraoperatively to reduce the risk of iatrogenic injury to the obturator neurovascular bundle? (A dissection-based study)
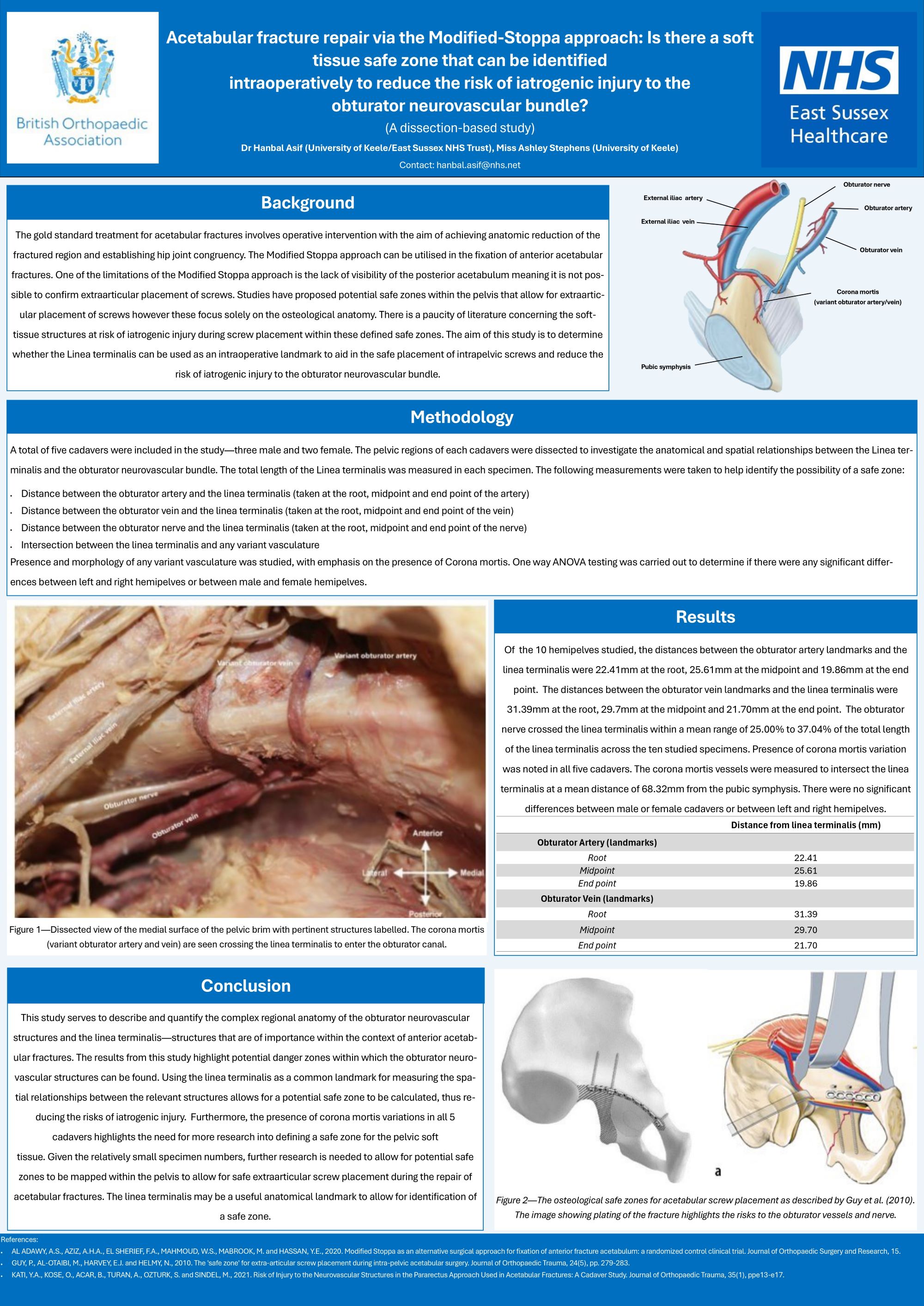
Hanbal Asif
University of Keele, Keele, United Kingdom
Abstract
Background: The Modified Stoppa approach is utilised in fixation of anterior acetabular fractures. Limitations include lack of visibility of the posterior acetabulum making it a challenge to confirm extraarticular placement of screws, thus posing risk of iatrogenic injury to surrounding soft tissue structures. Proposed "safe zones" in the literature focus mainly on osteological anatomy with a paucity of literature relating to soft tissue. This study aimed to determine whether the linea terminalis can be used as an intraoperative landmark to aid in placement of intrapelvic screws and reduce risk of iatrogenic injury to the obturator neurovascular bundle.
Methods: 5 cadavers were dissected to investigate the relationships between the linea terminalis and the obturator neurovascular bundle. A combination of qualitative descriptions and quantitative measurements were carried out to ascertain a "danger zone" for the obturator neurovasculature along the length of the linea terminalis.
Results: The obturator nerve crossed the linea terminalis within a range of 25.00% to 37.04% of the total length of the linea terminalis. The obturator vessels lie within a range of 12.00 mm to 26.00 mm from the linea terminalis at the site of the obturator canal. Presence of corona mortis variation was noted in all cadavers. No significant differences were found between left and right hemipelves or male and female cadavers.
Conclusion: This study highlights a potential "danger zone" within which the obturator nerve may cross the linea terminalis. The obturator vessels lie within the osteological "safe zone" described in the literature and are at risk of iatrogenic injury. The presence of corona mortis variations in all 5 cadavers highlights the need for more research into defining a safe zone for soft tissue.
The linea terminalis may be useful in determining intraoperative safe zones in order to reduce risk of iatrogenic injury to obturator neurovasculature.
882 - What is the Actual Incidence of Infection Control after an Intended Two-Stage Revision Total Hip Arthroplasty For Periprosthetic Joint Infection?
Long-term Results from a Referral Centre on Infection Control After The First Stage Procedure.
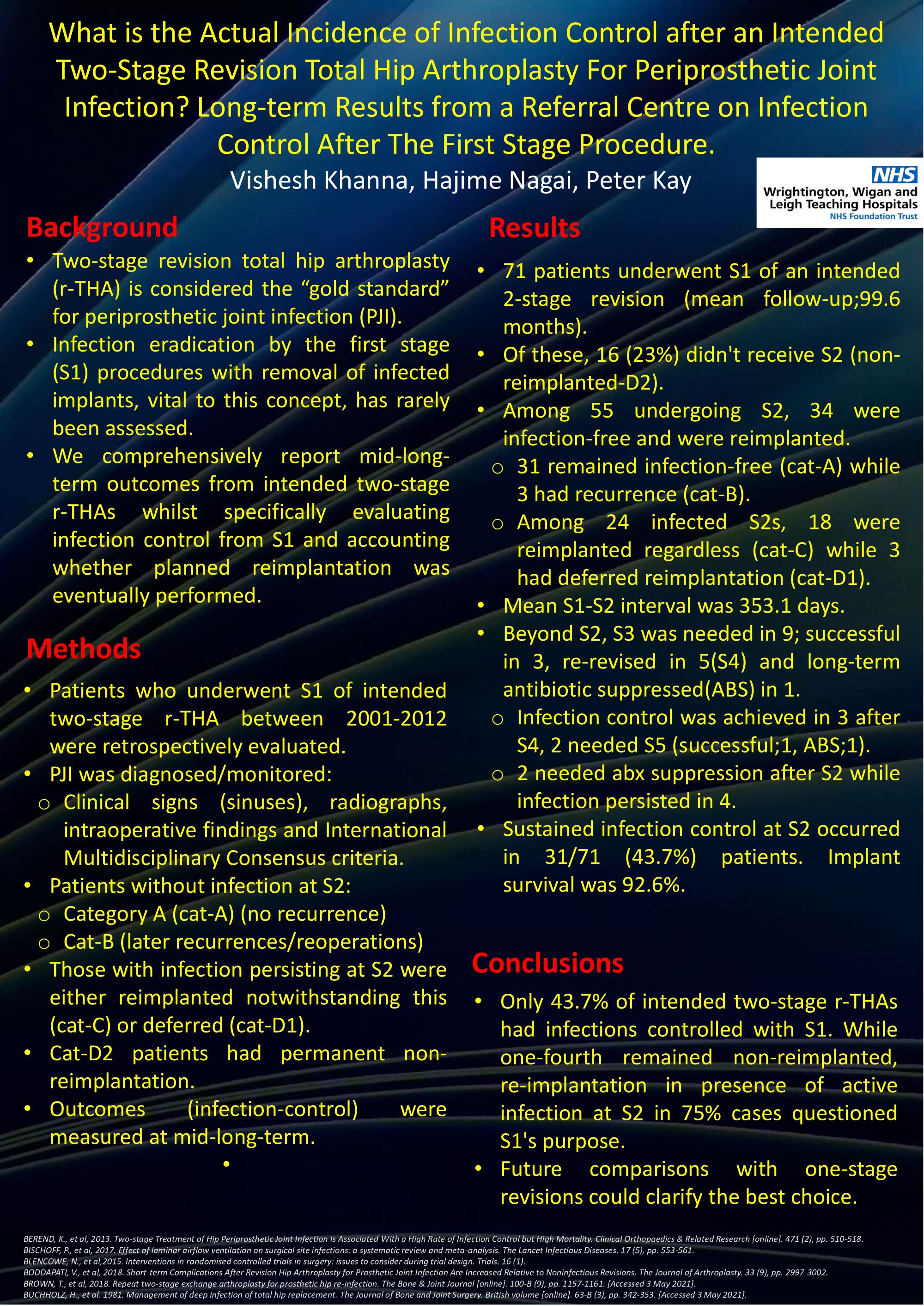
VISHESH KHANNA1, Hajime Nagai2, Peter Kay2
1Wirral University Teaching Hospital, Wirral, United Kingdom. 2Wrightington Hospital, Wigan, United Kingdom
Abstract
Background: Two-stage revision total hip arthroplasty (r-THA) is considered the “gold standard” for periprosthetic joint infection (PJI). Infection eradication by the first stage (S1) procedures with removal of infected implants, vital to this concept, has rarely been assessed. We comprehensively report mid-long-term outcomes from intended two-stage r-THAs whilst specifically evaluating infection control from S1 and accounting whether planned reimplantation was eventually performed.
Methods: Patients who underwent S1 of intended two-stage r-THA between 2001-2012 were retrospectively evaluated. PJI was diagnosed/monitored from clinical signs (sinuses), radiographs, intraoperative findings and International Multidisciplinary Consensus criteria.
Patients without infection at S2 were labelled category A (cat-A) (no recurrence) and cat-B (later recurrences/reoperations). Those with infection persisting at S2 were either reimplanted notwithstanding this (cat-C) or deferred (cat-D1). Cat-D2 patients had permanent non-reimplantation. Outcomes (infection-control) were measured at mid-long-term.
Results: Seventy-one patients underwent S1 of an intended 2-stage revision (mean follow-up;99.6 months). Of these, 16 (23%) didn't receive S2 (non-reimplanted-D2). Among 55 undergoing S2, 34 were infection-free and were reimplanted. Thirty-one remained infection-free (cat-A) while 3 had recurrence (cat-B).
Among 24 infected S2s, 18 were reimplanted regardless (cat-C) while 3 had deferred reimplantation (cat-D1).
Mean S1-S2 interval was 353.1 days. Beyond S2, S3 was needed in 9; successful in 3, re-revised in 5(S4) and long-term antibiotic suppressed(ABS) in 1. Infection control was achieved in 3 after S4, 2 needed S5 (successful;1, ABS;1). Two needed ABS after S2 while infection persisted in 4.
Sustained infection control at S2 occurred in 31/71 (43.7%) patients. Implant survival was 92.6%.
Findings: Only 43.7% of intended two-stage r-THAs had infections controlled with S1. While one-fourth remained non-reimplanted, re-implantation in presence of active infection at S2 in 75% cases questioned S1's purpose. Future matched comparisons with one-stage revisions could clarify the best choice.
Limb Reconstruction - Poster Abstracts
520 - Outcomes of complex tibial plateau fractures (Schatzker V & VI) treated with circular frame:
Retrospective review of 101 cases and tolerances in alignment, articular reduction and tibial/femoral articular width
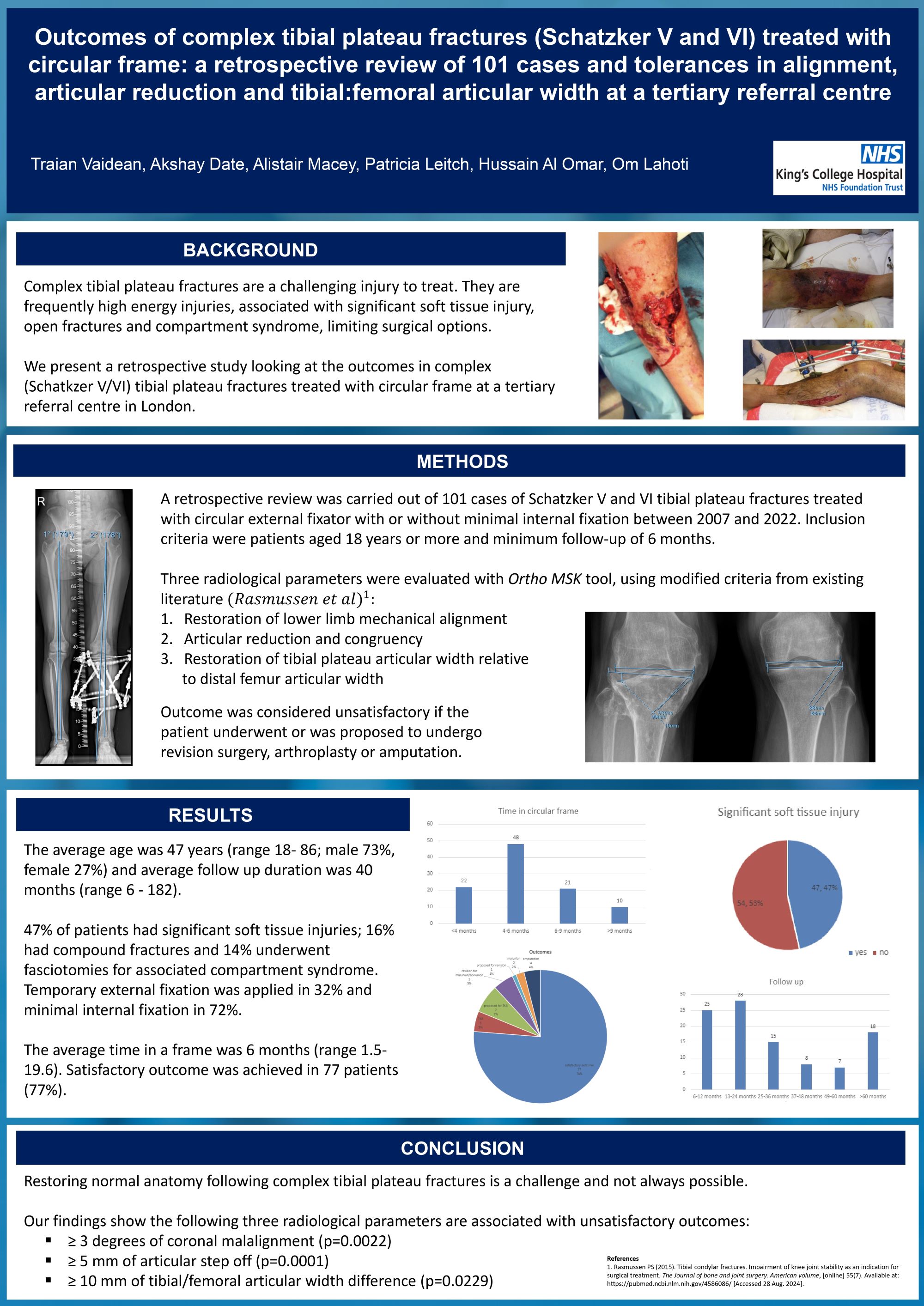
Traian Vaidean1, Akshay Date1, Alistair Macey2, Hussain Khalil Al-Omar3, Patricia Leitch1, Om Lahoty1
1King's College Hospital, London, United Kingdom. 2Queen Elizabeth University Hospital, Glasgow, United Kingdom. 3King Fahad Military Complex, Dhahran, Saudi Arabia
Abstract
Background: Complex tibial plateau fractures remain a challenging injury to treat. They are frequently high energy, associated with significant soft tissue injury, including open fractures and compartment syndrome.
Methods: Retrospective review of electronic records of 101 Schatzker V/VI tibial plateau fractures treated with circular frames+/- minimal internal fixation between 2007-2022 at King’s College Hospital, London. Included were patients aged over 18 years with minimum 6 months follow-up. Three radiological parameters were measured on PACS using Ortho MSK tool: reduction of articular congruency, restoration of lower limb mechanical alignment and restoration of tibial plateau articular width compared to distal femur articular width. Outcome was considered unsatisfactory if the patient underwent or was proposed for revision surgery, arthroplasty or amputation.
Results: Mean age was 47 years (18- 86), 73% were male and mean follow up was 40 months (6-182). 47% had significant soft tissue injuries; 16% had open fractures and 14% underwent fasciotomies for compartment syndrome. Temporary external fixation was applied in 32%, minimal periarticular internal fixation was used in 72% and the average time in a frame was 6 months (1.5-19.6). Satisfactory outcome was found in 77 patients (77%). There was statistically significant association between an unsatisfactory outcome and coronal malalignment of ≥ 3 degrees (P=0.0022), an articular step off ≥ 5mm (P=0.0001) and ≥ 10mm tibial/femoral articular width difference (P=0.0229).
Conclusion/Findings: Restoring normal anatomy following complex tibial plateau fractures is a challenge and not always possible. Our data shows that ≥ 3 degrees of coronal malalignment, ≥ 5 mm of articular step off and ≥ 10 mm of tibial/femoral articular width difference should be avoided as they are risk factors for a poor outcome.
586 - Bigger is not necessarily better – 2-ring circular frames associated with shorter duration of treatment in the management of complex tibial fractures – a retrospective cohort study
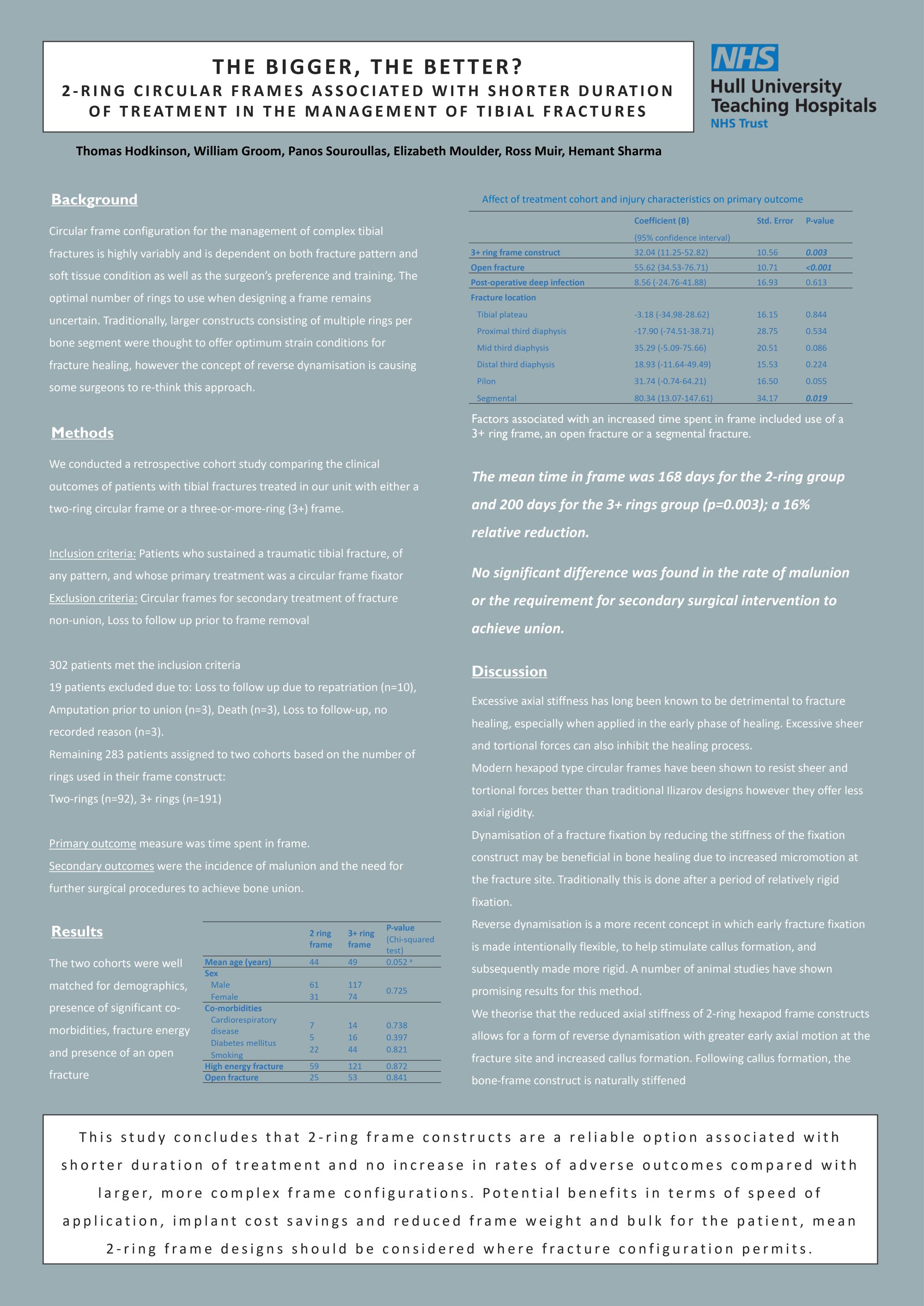
Thomas Hodkinson1, William Groom2, Panos Souroullas3, Elizabeth Moulder2, Ross Muir2, Hemant Sharma2
1Royal Hospital Derby, Derby, United Kingdom. 2Hull Royal Infirmary, Hull, United Kingdom. 3York and Scarborough Teaching Hospitals NHS Trust, York, United Kingdom
Abstract
Frame configuration for the management of complex tibial fractures is highly variably and is dependent upon both fracture pattern and surgeon preference. The optimal number of rings to use when designing a frame remains uncertain. Traditionally larger, multi-ring-per-segment constructs have been assumed to offer optimal stability and therefore favourable conditions for fracture healing but there is little in-vivo evidence for this and the recent concept of reverse dynamisation challenges this approach.
We compared the clinical outcomes in 302 consecutive patients with tibial fractures treated in our unit with either a stable two-ring circular frame or a three-or-more-ring (3+) frame. The primary outcome measure was time spent in frame. Secondary outcomes were the incidence of malunion and the need for further surgical procedures to achieve bone union.
The mean time in frame was 168 days for the 2-ring group and 200 days for the 3+ rings group (p=0.003). No significant differences were found in the rate of malunion or the requirement for secondary surgical intervention to achieve union. The groups were evenly matched for age, co-morbidities, energy of injury mechanism, post-treatment alignment and presence of an open fracture.
This study finds that 2-ring frame constructs are a reliable option associated with shorter duration of treatment and no increase in rates of adverse outcomes compared with larger, more complex frame configurations.
Ultimately, the number of rings used is likely not as significant a factor as span of fixation and overall construct stability, nevertheless, the potential benefits in terms of speed of application, implant cost savings and reduced frame weight and bulk for the patient, mean 2-ring frame designs should be considered where fracture configuration permits.
799 - Periprosthetic fractures of the tibia managed with circular frame
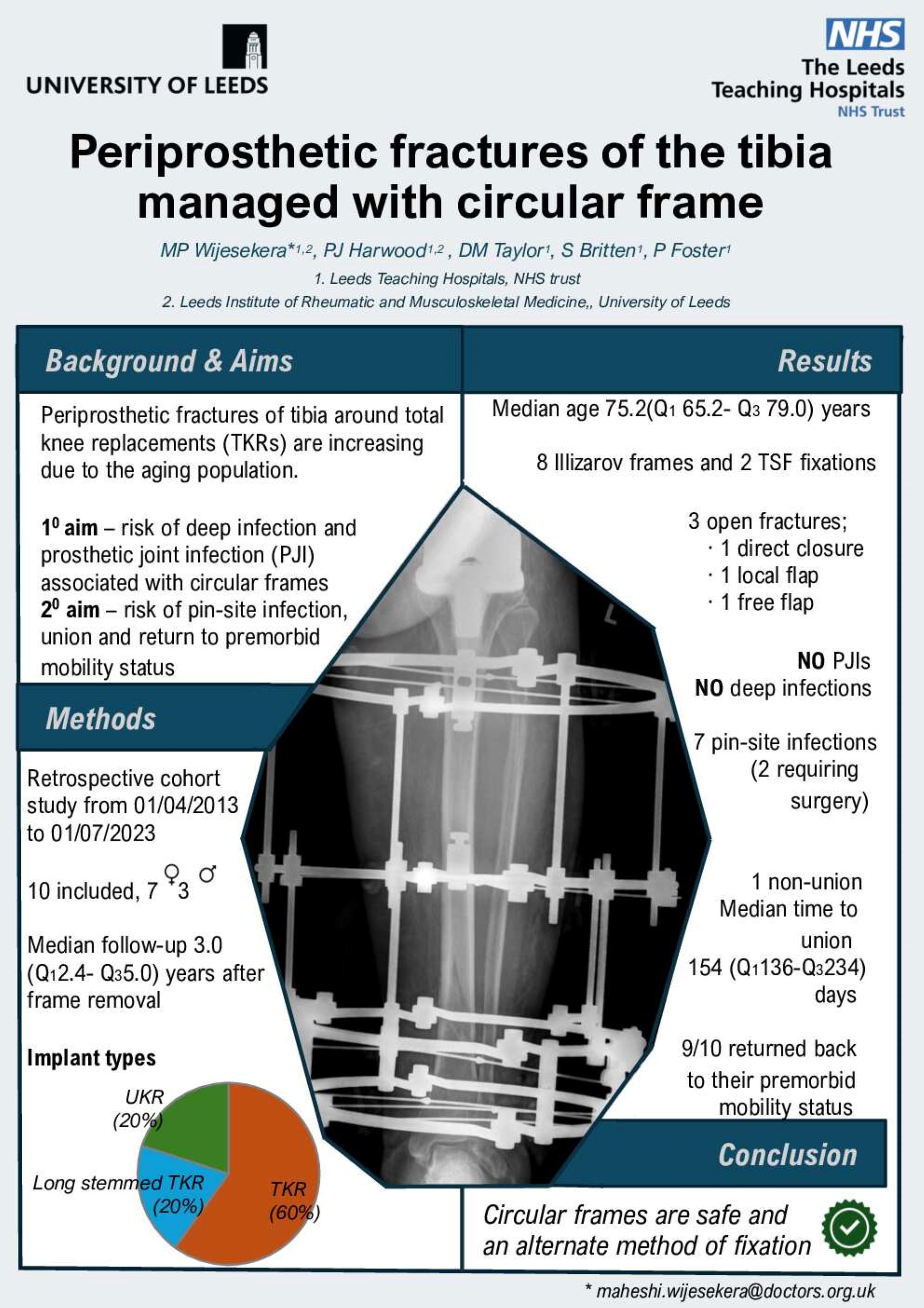
Maheshi Wijesekera, Paul J Harwood, Martin Taylor, Simon Britten, Patrick Foster
Leeds teaching hospitals, Leeds, United Kingdom
Abstract
Background: Periprosthetic fractures of tibia around knee replacements are increasing due to the aging population. The aim of this study was to look at the risk of deep infection and prosthetic joint infection(PJIs) associated with circular frame fixation of tibial fractures. The secondary aim was to look at the risk of pin-site infections, union and return to premorbid mobility status.
Methods: Local institutional approval was obtained. All patients with periprosthetic tibial fractures around a knee replacement were identified between 01/04/2013-01/07/2023 using a prospectively completed limb reconstruction database. Fifteen patients were identified and 5 were excluded as they deceased prior to frame removal. Ten patients were included in this analysis. There were seven females and 3 males. Six patients had total knee replacements (TKRs), two with long stemmed TKRs and two with unicompartmental knee replacements. Patients were followed up for a median 37.9(Q128.2- Q360.5) months from frame removal.
Results: The median age was 75.2(Q1 65.2- Q3 79.0)years.Three patients had open fractures with one undergoing primary closure, one having a local flap and the other patient having a free flap coverage. Mechanism of injuries included, 8 fall from standing height, 1 stress fracture with pre-existing varus deformity and 1 road traffic collision. Eight patients underwent Ilizarov frame application and two TSF fixation all being allowed to weight bear postoperatively. There were no cases of deep infections or PJIs in our series. There were 7 pin-site infections with two requiring surgical debridement. The median time to union was 154(Q1136–Q3 234) days with one case of non-union. Nine patients returned back to their premorbid mobility status.
Conclusions: We present a case series of tibial fractures around knee replacements and conclude that circular frame fixation is a safe and alternate method of fixation, with no risk of deep infection or PJIs.
Medical Student - Poster Abstracts
129 - Anterior Cruciate Ligament Reconstruction: Effect of graft tunnel position on early to mid-term clinical outcomes
Oliver Mann1, Oday Al-Dadah1,2
1South Tyneside District Hospital, South Shields, United Kingdom. 2Newcastle University, Newcastle upon-Tyne, United Kingdom
Abstract
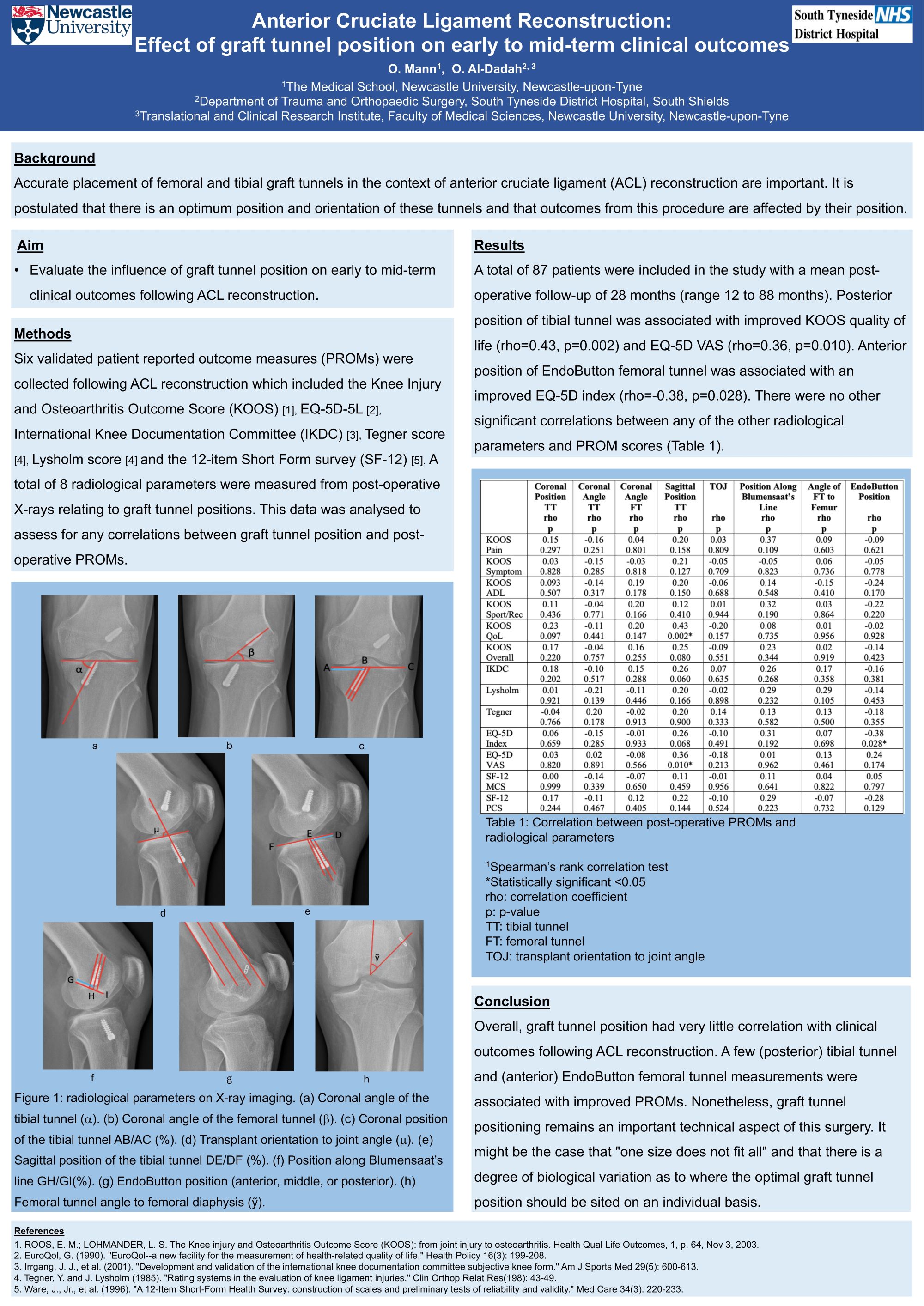
Background: Patient reported outcome measures (PROMs) can be used to assess knee function following anterior cruciate ligament (ACL) reconstruction. Intra-operatively, femoral and tibial tunnels are created to accommodate the new ACL graft. It is postulated that there is an optimum position and orientation of these tunnels and that outcomes from this procedure are affected by their position. The aim of this study was to evaluate the influence of graft tunnel position on early to mid-term clinical outcomes following ACL reconstruction.
Methods: Six PROMs were collected following ACL reconstruction which included the Knee Injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee (IKDC), Lysholm, Tegner, EQ-5D-5L, and Short Form 12-item Health Survey. A total of 8 radiological parameters were measured from post-operative X-rays relating to graft tunnel positions. This data was analysed to assess for any correlations between graft tunnel position and post-operative PROMs.
Results: A total of 87 patients were included in the study with a mean post-operative follow-up of 2.3 years (range 1 to 7 years). Posterior position of tibial tunnel was associated with improved KOOS quality of life (rho=0.43, p=0.002) and EQ-5D VAS (rho=0.36, p=0.010). Anterior position of EndoButton femoral tunnel was associated with an improved EQ-5D index (rho=-0.38, p=0.028). There were no other significant correlations between any of the other radiological parameters and PROM scores.
Conclusion: Overall, graft tunnel position had very little correlation with clinical outcomes following ACL reconstruction. A few (posterior) tibial tunnel and (anterior) EndoButton femoral tunnel measurements were associated with better PROMs.
132 - A Systematic Review of Natural Language Processing Applications in Trauma and Orthopaedics
Luke Farrow1, Arslan Khaliq Raja2, Lesley Anderson1, Mingjun Zhong1
1University of Aberdeen School of Medicine and Dentistry, Aberdeen, United Kingdom. 2University of Edinburgh Medical School, Edinburgh, United Kingdom
Abstract
Background: Prevalence of Artificial Intelligence (AI) algorithms within the Trauma and Orthopaedics (T&O) literature has greatly increased over the last ten years. One increasingly explored aspect of AI is the use of Natural Language Processing (NLP). We set out to review the current evidence for applications of NLP methodology in T&O, including assessment of study design and reporting.
Methods: MEDLINE, AMED, EMBASE, and CENTRAL were screened for studies pertaining to NLP in T&O from database inception to 31/12/23. An additional search of the grey literature was performed using OrthoSearch. The quality of reporting of included NLP were assessed according to the criteria outlined by Farrow et al. 2021 by two independent reviewers and classified as absent, incomplete, or complete. The review protocol was registered on PROSPERO (Registration number CRD42022291714).
Results: 31 articles were included in the final review. The most common subspeciality areas included Trauma, Arthroplasty, and Spine. 13% (4/31) related to online reviews / social media, 42% (13/31) to clinical notes / operation notes, 42% (13/31) to radiology reports and 3% (1/31) to systematic review. According to the reporting criteria 16% (5/31) were considered good quality, 74% (23/31) average quality and 6% (2/31) poor quality. The most commonly absent reporting criteria were evaluation of missing data (26/31), sample size calculation (31/31) and external validation of the study results (29/31 papers). Code and data availability were also poorly documented.
Conclusions: Application of NLP is becoming increasingly common in T&O. The quality of papers published is however mixed, with relatively few considered high quality according to our reporting criteria. We highlight key consistent deficiencies in work relating to NLP that are integral to the widespread application of AI technology in clinical practice. Open science is an important part of research transparency that should be encouraged in NLP applications.
149 - Hemiepiphysiodesis Corrects Lower Extremity Coronal Plane Deformity in Children with Skeletal Dysplasia Irrespective of Ligamentous Instability
Deeptiman James1, Prabjit Ajrawat1, Andrew Howard1,2, Maryse Bouchard1,2
1Division of Orthopaedics, The Hospital for Sick Children, Toronto, Canada. 2Department of Surgery, University of Toronto, Toronto, Canada
Abstract
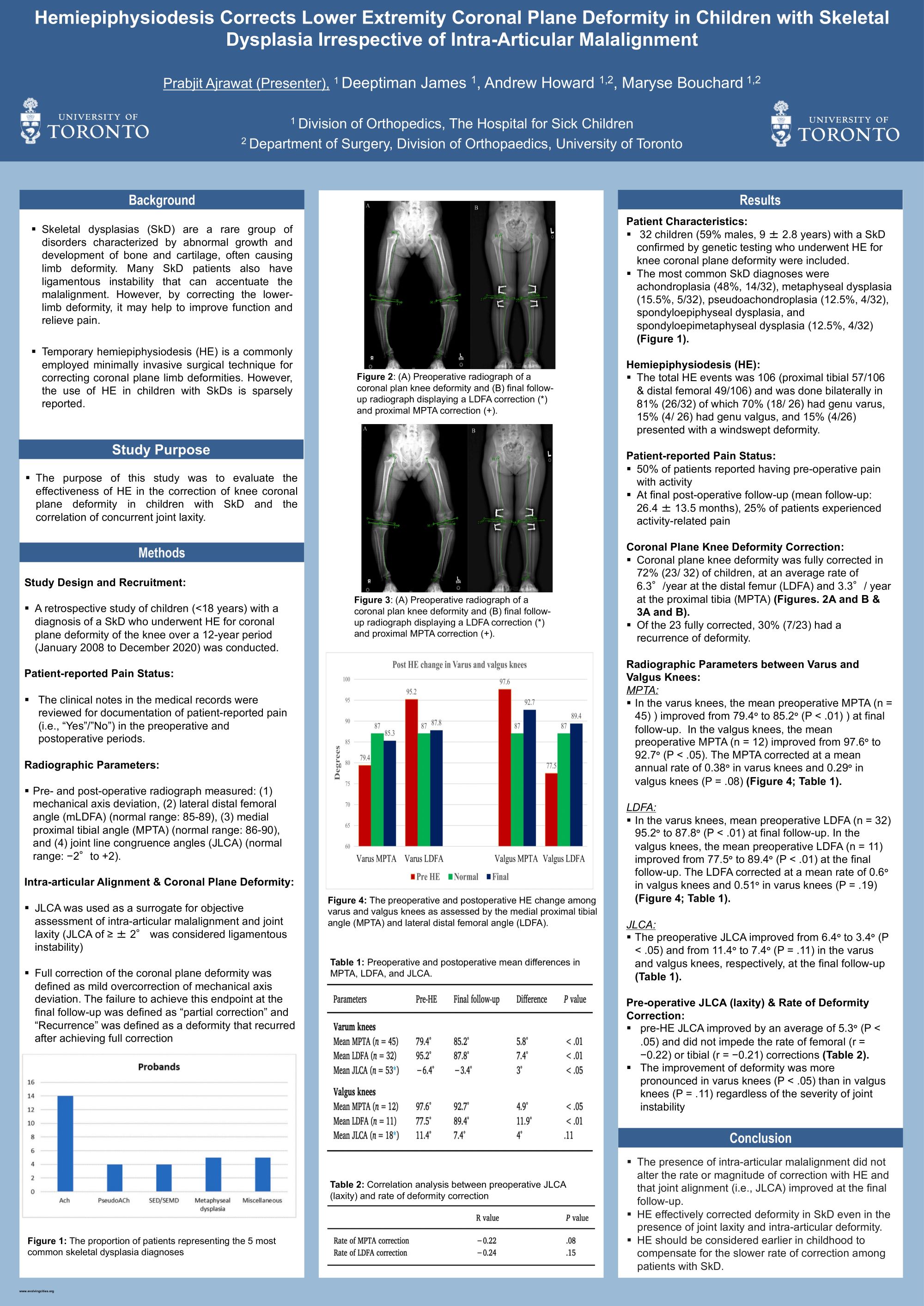
Introduction: Skeletal Dysplasias (SkD) are a rare group of disorders characterized by abnormal bone and cartilage development often causing limb deformity. Many patients also have ligamentous instability that can either present as generalized ligamentous laxity or as focal coronal plane instability, which can accentuate the malalignment. Temporary hemiepiphysiodesis (HE) is a commonly employed minimally invasive surgical technique for correcting coronal plane limb deformities. This study evaluated the effectiveness of HE in correcting knee coronal plane deformity in children with SkD and the correlation of concurrent joint laxity.
Methods: A retrospective cohort study was conducted to evaluate radiological outcomes of HE for coronal plane knee deformities. Changes in distal femoral and proximal tibial mechanical angles and knee joint line congruence angles (JLCA) were analyzed. An increased JLCA of ≥±2° was considered a knee with ligamentous instability. Pre- and post-operative patient-reported pain status was recorded.
Results: Fifty-six tibial and 42 femoral HE procedures in 32 children (mean age: 9.8±2.8 years) were included. The deformity was fully corrected in 23/32 (72 %) children, at an average annual rate of 6.3° at the distal femur and 3.3° at the proximal tibia, over 21.9±12.6 months. The overall pre-HE JLCA improved by an average of 5.3° (p<0.05). The improvement was more pronounced in varus (n=45; p<0.05) than valgus (n= 12; p=0.11) knees but regardless of the severity of joint instability, pre-HE JLCA did not impede the rate of femoral (r = -0.22) or tibial (r = -0.21) corrections. Pre-operative pain was reported by 78% of patients whereas only 25% of patients reported post-operative pain at final follow-up.
Conclusion: The presence of coronal plane instability did not affect the rate and the magnitude of correction with HE in this cohort. Coronal plane deformities and JLCA improve with deformity correction by HE in children with SkD.
156 - Tibial Spine Avulsion Fractures in Paediatric Patients: A Systematic Review and Meta-Analysis of Surgical Management
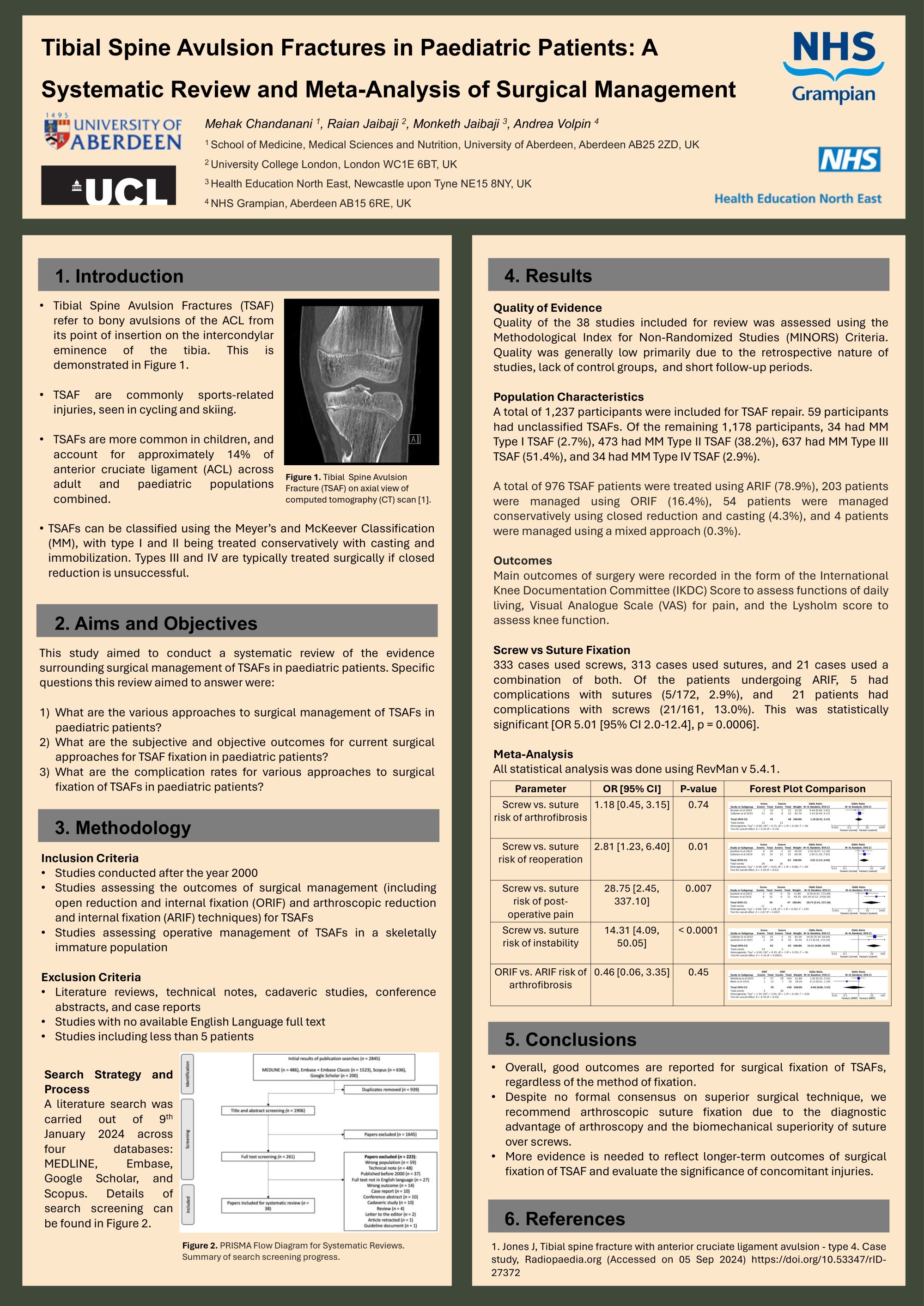
Mehak Chandanani1, Raian Jaibaji2, Monketh Jaibaji3, Andrea Volpin4
1School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, Aberdeen, United Kingdom. 2University College London, London, United Kingdom. 3Health Education North East, Newcastle Upon Tyne, United Kingdom. 4NHS Grampian, Aberdeen, United Kingdom
Abstract
Background: Tibial spine avulsion fractures (TSAFs) are bony avulsions of the anterior cruciate ligament (ACL) from its insertion point on the tibial intercondylar eminence, accounting for approximately 14% of ACL injuries. Due to the frequent occurrence of these injuries in skeletally immature paediatric populations, evaluating treatment approaches for optimal long-term outcomes becomes crucial. This study aims to systematically review the current evidence for the surgical management of paediatric TSAFs.
Methods: A search was carried out across four databases: MEDLINE, Embase, Scopus, and Google Scholar. Studies discussing the outcomes of surgical management of paediatric TSAFs since the year 2000 were included. Studies with similar outcome evaluation were pooled for meta-analysis using a random-effects model to account for unobserved heterogeneity. All statistical analysis was conducted using RevMan v5.4.1 and a p value of < 0.05 was considered statistically significant.
Results: Of 38 studies included for review, 13 studies reported outcomes of TSAF patients undergoing screw fixation only, and 12 studies used suture fixation only. In total, 976 patients underwent arthroscopic reduction and internal fixation (ARIF) and 203 patients underwent open reduction and internal fixation (ORIF). The risk of arthrofibrosis with the use of ARIF (p = 0.45) and screws (p = 0.74) for TSAF repair was not significant. There was a significantly increased risk of knee instability (p < 0.0001), reoperation (p = 0.01), and post-operative pain (p = 0.007) with screw fixation compared to sutures.
Conclusions: While the overall benefits of sutures over screws and ARIF over ORIF are unclear, there is clear preference for ARIF and suture fixation for TSAF repair in practice.
Implications: We recommend large-scale comparative studies to delineate long-term outcomes for various TSAF fixation techniques.
169 - Staphylococcus aureus Bacteraemia in children with Bone and Joint infections: A Quality Improvement Project
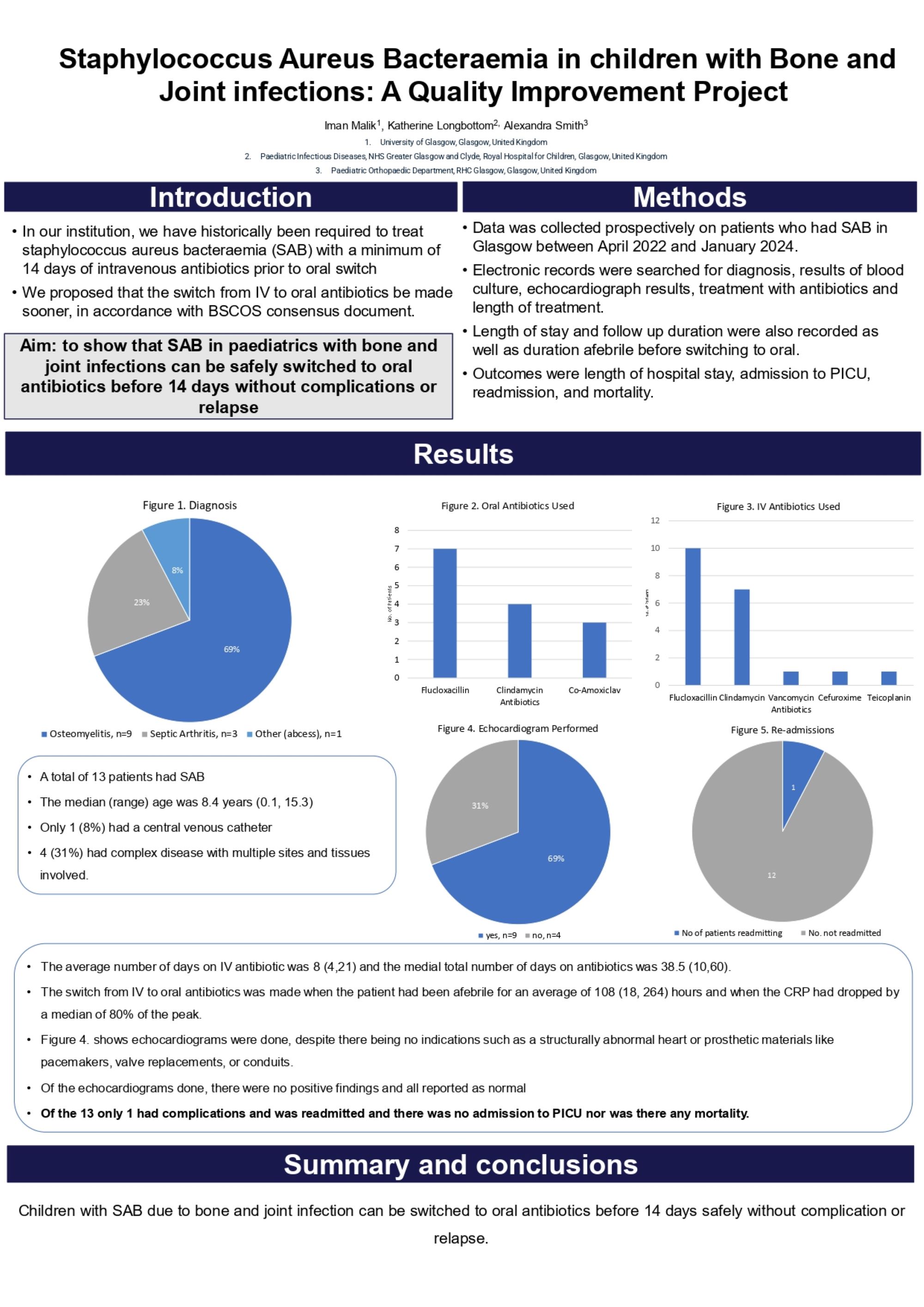
Iman Malik1, Katherine Longbottom2, Alexandra Smith3
1University of Glasgow, Glasgow, United Kingdom. 2Paediatric Infectious Diseases, NHS Greater Glasgow and Clyde, Royal Hospital for Children, Glasgow, United Kingdom. 3Paediatric Orthopaedic Department, RHC Glasgow, Glasgow, United Kingdom
Abstract
Introduction: In our institution, we have historically been required to treat Staphylococcus aureus bacteraemia (SAB) with a minimum of 14 days of intravenous antibiotics prior to oral switch. We proposed that the switch from IV to oral antibiotics be made sooner, in accordance with BSCOS consensus document. The aim of this quality improvement project was to show that SAB in paediatrics with bone and joint infections can be safely switched to oral antibiotics before 14 days without complications or relapse.
Methods: Data was collected prospectively on patients who had SAB in Glasgow between April 2022 and January 2024. Data was collected on diagnosis, results of blood culture, echocardiograph results, treatment with antibiotics and length of treatment. Length of stay and follow up duration were also recorded as well as duration afebrile before switching to oral. Outcomes were measured using length of hospital admission, readmission rate, whether admitted to PICU, and mortality.
Results: A total of 13 patients had SAB during the time period and the median (range) age was 8.4 years (0.1, 15.3). The average number of days on IV antibiotic was 8 (4,21) and the median total number of days on antibiotics was 38.5 (10,60). The switch from IV to oral was made when the patient had been afebrile for an average of 108 (18, 264) hours and when the CRP had dropped by a median of 80% of the peak. Of the 13 only 1 had complications and was readmitted and there was no admission to PICU nor was there any mortality. The average length of stay in hospital was 8 (4,21) days and the average follow up length was 6.5 (1, 18) months.
Conclusions: Children with SAB due to bone and joint infection can be switched to oral antibiotics before 14 days safely without complication or relapse.
173 - When Do Patients Experience Benefit After Reverse Shoulder Arthroplasty for Cuff Tear Arthropathy?
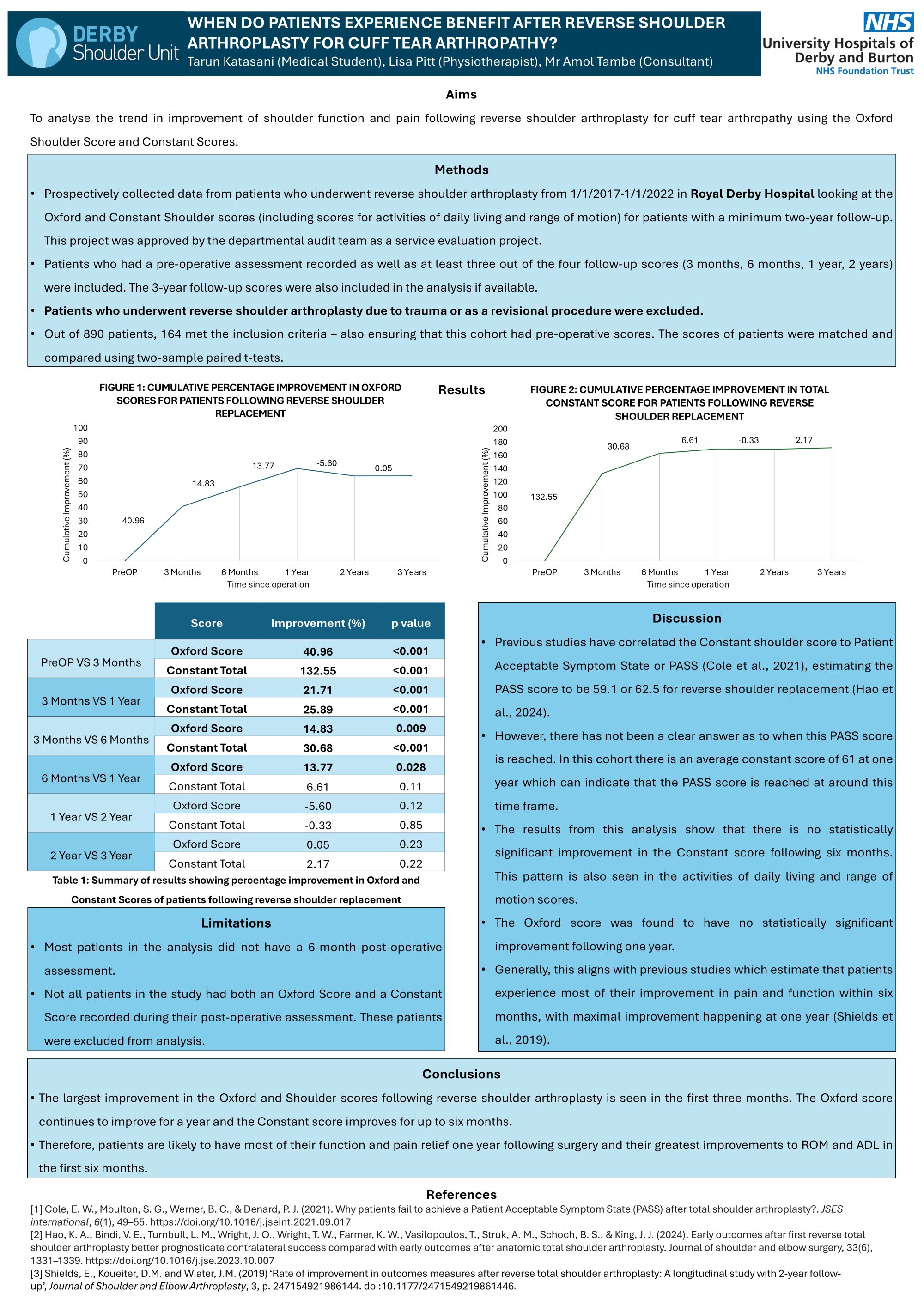
Tarun Katasani1, Amol Tambe2, Lisa Pitt2
1University of Nottingham, Nottingham, United Kingdom. 2Royal Derby Hospital, Derby, United Kingdom
Abstract
Aims: To analyse the improvement in shoulder function and pain following reverse shoulder arthroplasty using the Oxford and Constant Shoulder Scores.
Methods: Prospectively collected data from patients who underwent reverse shoulder arthroplasty from 1/1/2017-1/1/2022 in Royal Derby Hospital was analysed. The Oxford and Constant Shoulder scores (for ROM and ADL) for patients with a two-year follow-up were included in the analysis. Patients who had a pre-operative assessment recorded as well as at least three out of the four follow-up scores (3 months, 6 months, 1 year and 2 years) were included. Data from those who had a 3-year follow-up were also included in the analysis. Patients who underwent reverse shoulder arthroplasty due to trauma or as a revisional procedure were excluded. The scores of patients were then matched and compared using two-sample paired t-tests.
Results: Out of 890 patients,164 met the inclusion criteria – also ensuring that this cohort had pre-operative scores. The Oxford score improved by 40.96% (P<0.001) in the first three months and continued to improve until one year (P<0.001). The Constant score had a 132.55% (P<0.001) improvement in the first three months and continued to improve until six months. There was no statistically significant improvement following the six-month mark at least until the third year of follow-up. Both the ADL and ROM scores improved in this pattern.
Conclusions: Both shoulder scores generally improved following reverse shoulder arthroplasty. The largest improvement was seen in the first three months. The Oxford Score continued to improve for up to a year, but the Constant Score improved up to six months. Therefore, patients are likely to have most of their function and pain relief one year following surgery and their greatest improvements to ROM and ADL in the first six months.
175 - Investigating the impact of COVID-19 Lockdowns on Fragility Fracture Risk in a large observational cohort
Hamzah Amin1, Aqib Khan2, Marwan Bukhari2
1Lancaster University Medical School, Lancaster, United Kingdom. 2University Hospitals of Morecambe Bay NHS Foundation Trust, Lancaster, United Kingdom
Abstract
Background: COVID-19 lockdowns predisposed to sedentary lifestyles, social isolation and compositional changes such as obesity which may have affected fracture risk. However, limited studies describe such an association. We will compare baseline demographics inclding fracture risk factors between the pre- and post-COVID-19 patients and to model the impact of lockdowns on fracture risk.
Methods: Patients were referred to our DEXA scanner from 2004 to 2024. We subsequently categorised them as pre- or post-March 23, 2020 (pre-COVID-19 and post-COVID-19) to allow analysis between the groups. Demographic, BMD, and compositional data were compared between the 2 populations. A Multivariate logistic regression was fit to determine whether post-COVID-19 referrals were more prone to fractures. Subgroup analysis examined fracture risk at 1, 2, and 3 years post-COVID-19. All analyses were adjusted for confounders.
Results: Of 43,799 scanner referrals, 6,564 were post-COVID-19. Post-COVID-19 patients had higher non-hip fracture rates (42.0% vs. 39.8%), were 3 kg heavier, were more likely to be vitamin d deficient and had lower left femur T-scores (T-score -1.2 vs -0.9). Logistic regression revealed increased fracture risk (OR 1.08, 95% CI 1.01,1.14), but lower hip fracture risk (OR 0.82, 95% CI 0.68-0.98). The risk of fracture was elevated for the first two years post lockdown with a subsequent protective effect observed at three years (OR 0.98, 95% CI 0.80, 0.97).
Conclusion: COVID-19 lockdown may have made patients more susceptible to fracture due to reduced BMD, weight gain and Vitamin d deficiency. We recommend a proactive screening approach be adopted by clinicians to identify at risk elderly patients as well as correcting vitamin d deficiency and promoting strength and weight training, which may help to reduce fracture risk. Further research Is needed with prospective cohorts to corroborate this risk.
178 - Glucocorticoid induced adiposity is a Strong Predictor of Fragility Fractures in a Large Cohort: A Cross Sectional Study
Hamzah Amin1, Aqib Khan2, Marwan Bukhari2
1Lancaster University medical school, Lancaster, United Kingdom. 2University hospitals of morecambe bay NHS foundation trust, Lancaster, United Kingdom
Abstract
Background: Glucocorticoids (GC) predispose to fracture through a reduction in BMD, however, GCs also induce adiposity. Emerging evidence is highlighting the deleterious effect of adiposity on bone as well as an increased risk of fracture. Hence the aim of this study is to investigate GC induced adiposity as a predictor of fragility fracture in a large cohort.
Methods: Data was collected from patients referred for a DEXA scan in the northwest of England between 2004-2019. Comparative statistics were performed between the GC and non-GC referred populations, with further analysis of the fractured GC and non-fractured GC subgroups. A multivariate logistic regression was fit to model the fat percentage at the abdomen (FPA), left hip (FPLH) and right hip (FPRH) as predictors of both hip and non-hip fragility fracture. All results were adjusted for possible confounders.
Results: 8,023 GC and 23,523 non-GC patients were referred to our scanner. Mean age of patients on GCs was 67.3 years (SD 28.3) versus non-GC 63.8 years (SD 13.7). Fractured GC patients had higher levels of peripheral fat than non-fractured GC patients. Only the FPLH predicted hip fracture (OR 12 95% CI 1.1,128.1). All anatomical sites of adiposity we analysed predicted non-hip fracture including the FPLH (OR 14.5 95% CI 3.7,15.1), FPRH (OR 6.7 95% CI 3.2,14.0) and FPA (OR 4.5 95% CI 2.6,7.7).
Discussion: GC induced adiposity was a good predictor of non-hip fracture with uncertain results for hip fracture. This indicates the importance of peripheral adiposity as a predictor of both hip and non-hip fragility fracture in patients GCs. While central obesity may precipitate bone loss in these patients through hormonal mechanisms, peripheral adiposity may directly increase fracture risk in patients taking GCs by predisposing to falls due to mechanical instability. Further research is needed to validate our findings using large prospective cohorts.
212 - DXA Scanning in Fragility Fractures - A Tool for Thorough Investigation or Cause of Treatment Delay? A Retrospective Audit with a Fracture Liaison Service in a Dublin Teaching Hospital
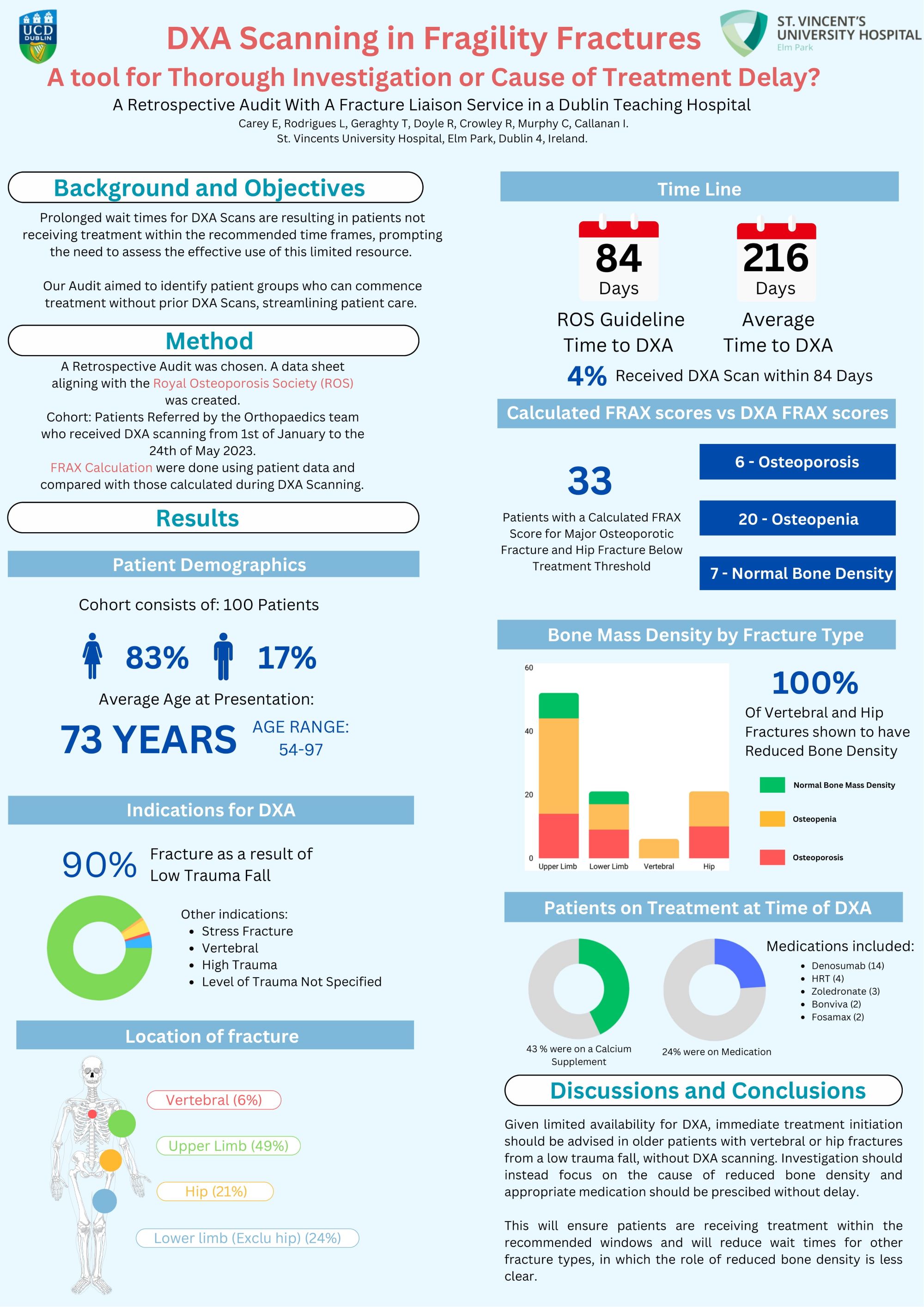
Emily Carey1, Leena Rodrigues2, Tim Geraghty2, Rachael Doyle2
1University College Dublin, Dublin, Ireland. 2St Vincents University Hospital, Dublin, Ireland
Abstract
Background: The aim of this audit was to analyse risk factors (RF) in patients with fragility fractures, to calculate FRAX score based on patient history and compare with DXA results, to compare wait times with recommended guidelines and identify the proportion of patients on treatment at time of DXA.
Methods: 100 patients from January to May were chosen, data was collected including RF, fall history, DXA and FRAX scores.
Results: The cohort was predominantly female (83%), with average age 73. Most common DXA indication was low trauma fall (90%) and fracture types consisted of vertebral (6%), hip (21%), upper limb (49%), and lower limb excluding hip (24%). Average wait time to DXA was 216 days, with only 4% undergoing DXA within 84 days as per guidelines. At time of DXA only 20% were on medical therapy (bisphosphonates, Denosumab). 100% of vertebral and hip fractures were osteopaenic or osteoporotic. 48% and 36% of vertebral and hip fractures respectively were on medical therapy. 29% of osteoporotic hip fractures and 50% of osteoporotic vertebral fractures were not receiving any medical therapy, calcium or vitamin D supplementation or bone protective treatments (eg HRT). 33 patients had patient history based FRAX scores indicating they were below treatment threshold, of these 6 had osteoporosis, 29 had osteopenia and 7 had normal bone mineral density (BMD).
Conclusion: In patients presenting with a fracture as a result of a low trauma fall treatment should not be delayed while waiting for DXA confirmation, particularly in fracture types typical of fragility fractures such as hip and vertebral, 100% of which had reduced BMD. History based FRAX scores are a useful tool but may overestimate patient BMD therefore should not prevent a patient receiving treatment. They can be used in conjunction with patient RF and fall history to aid clinical judgement.
284 - A cadaveric study mapping the cutaneous nerves innervating the posterior hip as targets to optimise analgesia for hip surgery.
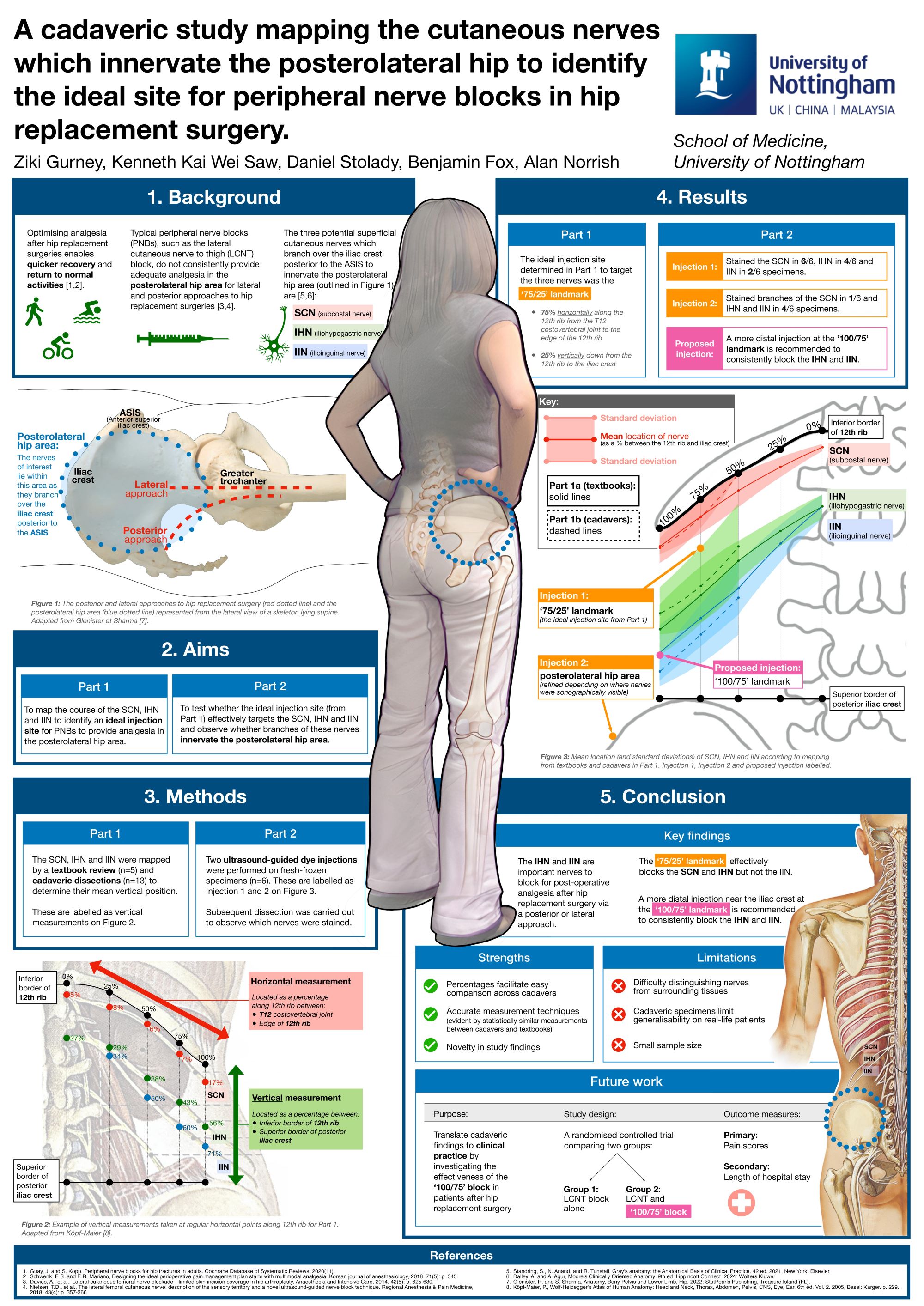
Ziki Gurney1, Kenneth Kai Wei Saw1, Daniel Gareth Stolady2, Benjamin Fox2, Leia Boote1, Alan Norrish1
1University of Nottingham, Nottingham, United Kingdom. 2The Queen Elizabeth Hopsital King's Lynn NHS Foundation Trust, King's Lynn, Norfolk, United Kingdom
Abstract
Background: Achieving day case surgery for hip replacement requires excellent post-operative analgesia. Nerve blocks in hip surgery do not consistently provide good pain relief, particularly for the posterior approach. This study investigates which nerves predominantly innervate this area. The most likely candidates for innervation are the subcostal (SCN), iliohypogastric (IHN) or ilioinguinal (IIN) nerves.
Methods: We mapped the SCN, IHN and IIN by a textbook review (n=5) identifying the mean and standard deviation for the nerve position between the 12th rib and iliac crest. We correlated these results with anatomical dissection in fresh-frozen specimens (n=13). Ultrasound-guided dye injections were carried out on 6 specimens at two sites based on the position of the nerves. Then further dissection of the SCN, IHN and IIN was carried out to see whether the ultrasound-guided dye injections were effective in targeting the nerve branches.
Results: We identified the ideal injection site to target the 3 nerves as a ‘75/25’ landmark: 75% horizontally along the 12th rib from the T12 spinous process to the edge of the 12th rib, and 25% vertically down from the 12th rib to the iliac crest. When injecting dye into the ‘75/25’ landmark, we stained the SCN in 6/6, IHN in 4/6 and IIN in 2/6 cadaveric specimens. When we injected distally at the second site, we stained branches of the SCN in 1/6 and IHN and IIN in 4/6 cadaveric specimens.
Conclusions: Our mapping shows the most important nerve for post-operative analgesia after hip replacement in the posterior aspect of the wound is the IHN and IIN. This study shows that the novel ‘75/25’ landmark is effective in blocking the SCN and IHN but not the IIN. We recommend the more distal injection near the iliac crest, to consistently block the IHN and IIN.
289 - Accelerometer-assisted physical activity outcomes during the first year of recovery after anterior cruciate ligament reconstruction: A prospective cohort pilot study
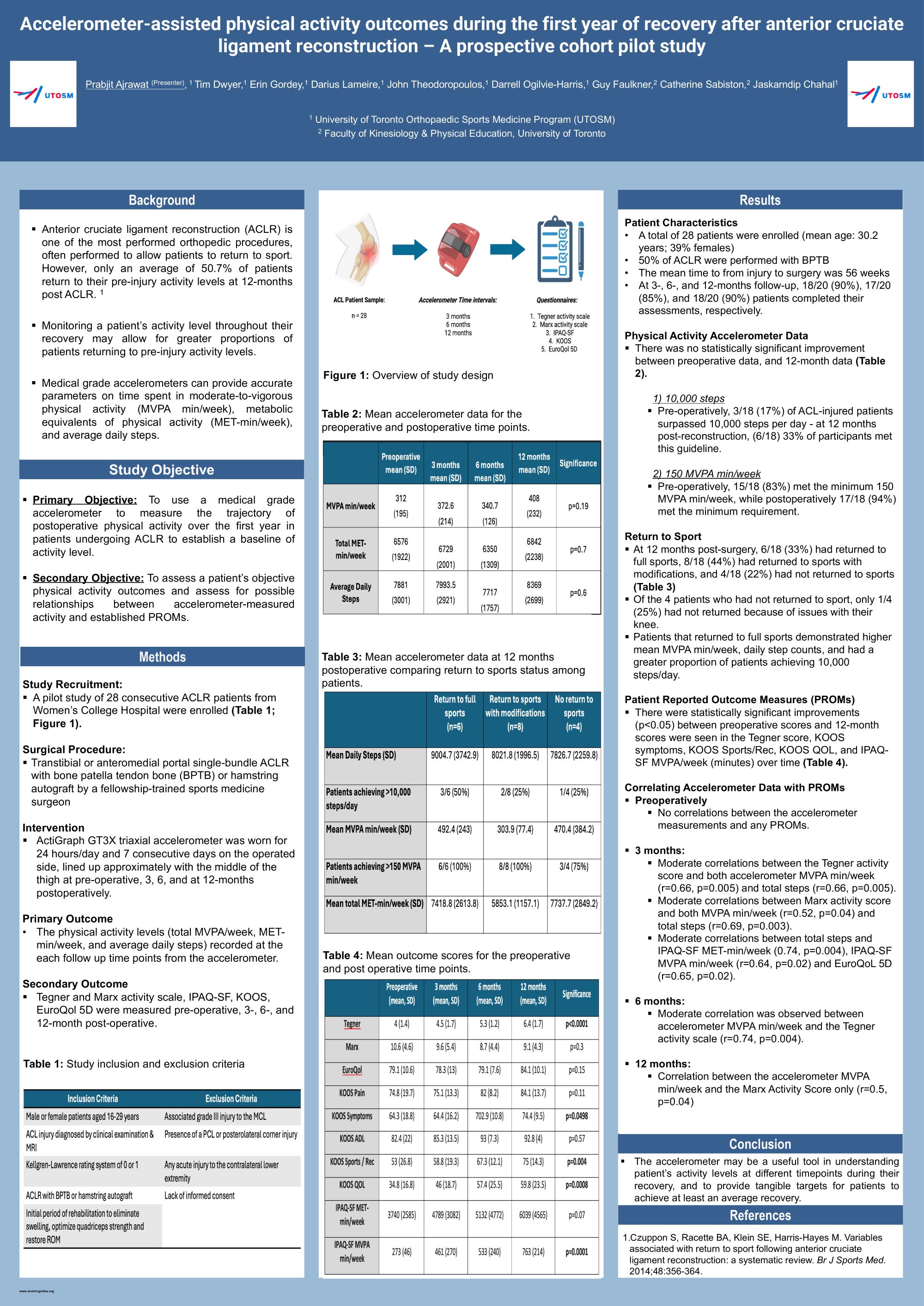
Tim Dwyer1, Erin Gordey1, Prabjit Ajrawat1, Darius Lameire1, John Theodoropoulos1,2, Darrell Ogilvie-Harris1, Guy Faulkner3, Catherine Sabiston3, Jaskarndip Chahal1
1University of Toronto Orthopaedic Sports Medicine Program (UTOSM), Division of Orthopaedic Surgery, Department of Surgery, University of Toronto, toronto, Canada. 2Mount Sinai Hospital, Division of Orthopaedic Surgery, Department of Surgery, University of Toronto, toronto, Canada. 3Faculty of Kinesiology & Physical Education, University of Toronto, toronto, Canada
Abstract
Background: Wearable activity-measurement devices are increasingly popular but there is little information regarding their use in patients undergoing orthopaedic procedures. The purpose of this study was to assess accelerometer-measured data after surgery and to compare these values to patient-reported measures.
Methods: Adult patients undergoing ACL reconstruction were included. The Tegner activity scale, Marx activity scale, IPAQ-SF, KOOS, and EuroQol 5D were administered pre-operatively and at three, six, and 12 months post-operatively. At these intervals, each participant was asked to wear an Actigraph GT3X triaxial accelerometer for seven consecutive days. Time spent in moderate-to-vigorous physical activity (MVPA min/week), metabolic equivalents of physical activity (MET-min/week), and average daily steps were calculated from the accelerometer and correlated with questionnaires.
Results: Eighteen patients (mean age 30 years; 43% female) completed the 12-month assessment. Significant improvements over time were seen in the Tegner scale, KOOS symptoms, KOOS Sports / Rec, KOOS QOL, and IPAQ-SF MVPA/week (minutes). There were also non-statistically significant improvements in all accelerometer measurements at the final follow-up. Preoperatively, 3/18 (17%) of patients met the 10,000 steps/day recommendations and at 12 months postoperatively 6/18 (33)% of patients met this guideline. Preoperatively, 15/18 (83%) met the minimum 150 MVPA min/week recommendations, while postoperatively 17/18 (94%) met the minimum requirement. At six months post-operatively, a moderate correlation was observed between accelerometer MVPA/week and the Tegner activity scale (r=0.74, p=0.004). At 12 months, there was a moderate correlation between the accelerometer MVPA/week and the Marx activity scale (r=0.5, p=0.04).
Conclusion: Accelerometers may be a useful tool in understanding patients’ activity levels at different time points during their recovery, and to provide tangible targets for patients to achieve post-operatively. Larger patient cohorts are required in creating recommendations for activity levels and determining possible correlations with post-operative activity and return to sport.
301 - Evaluation of The Diagnostic Accuracy of Spect/Ct in The Noninfected Painful Total Knee Replacement (Tkr) Through Correlation with Intraoperative Findings
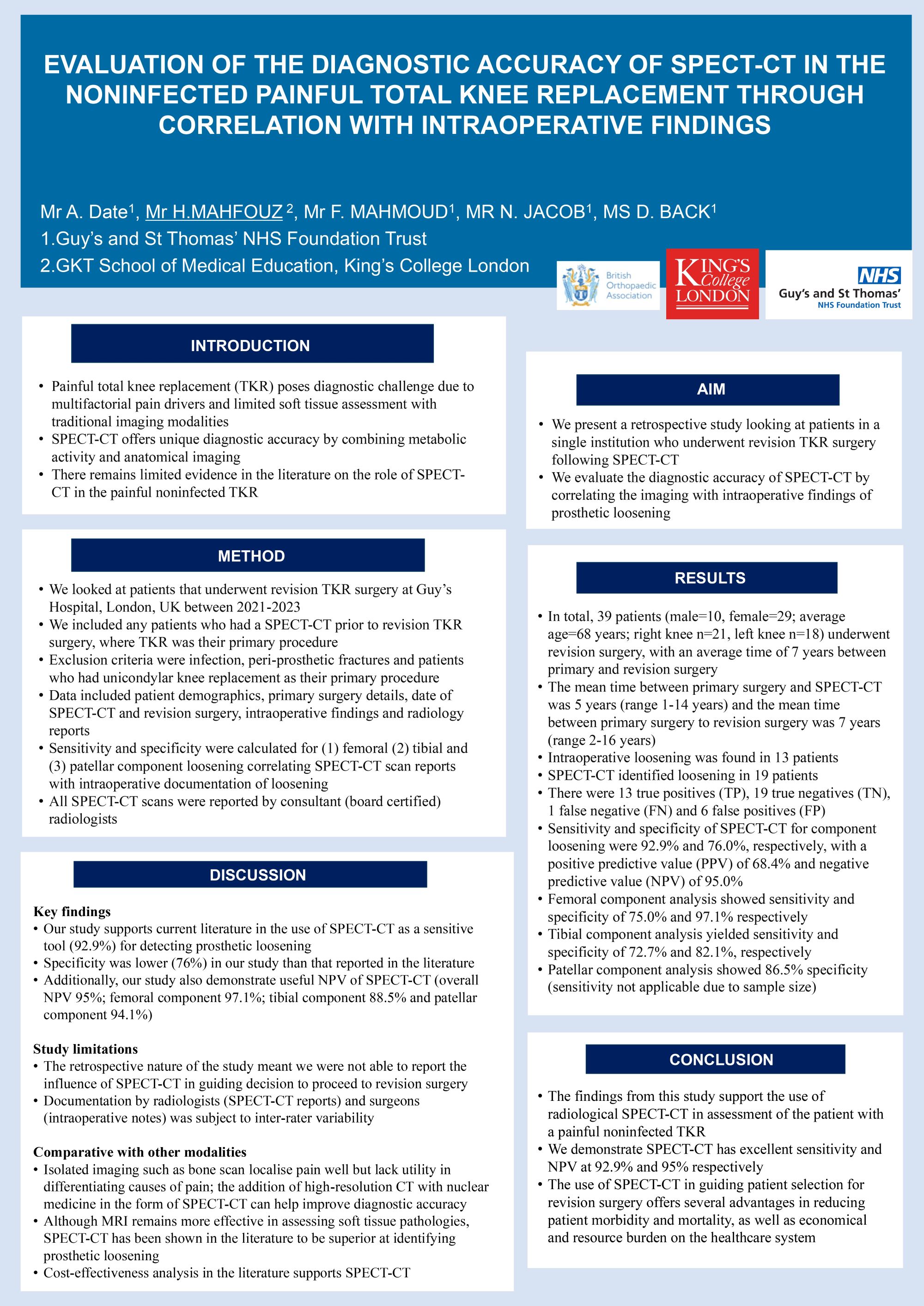
Hassan Mahfouz1, Akshay Date2
1King's College London, London, United Kingdom. 2Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom
Abstract
Background: Painful total knee replacement (TKR) poses diagnostic challenges with traditional imaging modalities. Emerging technologies like SPECT/CT offer superior diagnostic accuracy. While previous studies support its utility, further research is needed to establish its diagnostic accuracy in painful noninfected TKRs.
Methods: Data was analysed from revision total knee replacement (TKR) surgeries at Guys and St Thomas’ Hospital (2021-2023). Data included demographics, primary surgery details, SPECT/CT and revision surgery dates, intraoperative findings, and radiology reports. Sensitivity and specificity were calculated for femoral, tibial, and patellar component loosening using Technetium-99m for SPECT/CT scans. Intraoperative notes were scrutinised, excluding unclear or missing data.
Results: In total, 39 patients (male=10, female=29; average age=68 years) underwent revision surgery, with an average time of 7 years between primary and revision surgeries. Intraoperative loosening was found in 13 patients, while SPECT/CT identified loosening in 19 patients. There were 13 true positives (TP), 19 true negatives (TN), 1 false negative (FN) and 6 false positives (FP). Sensitivity and specificity of SPECT/CT for component loosening were 92.9% and 76.0%, respectively, with a positive predictive value (PPV) of 68.4% and negative predictive value (NPV) of 95.0%. Femoral component analysis showed sensitivity and specificity of 75.0% and 97.1%, respectively, while tibial component analysis yielded sensitivity and specificity of 72.7% and 82.1%, respectively. Patellar component analysis had 0% sensitivity and PPV, with specificity at 86.5% and NPV at 94.1%.
Conclusions: The findings from this study support the use of radiological SPECT/CT in assessment of the patient with a painful noninfected TKR. We showed SPECT/CT has excellent sensitivity and NPV at 92.9% and 95% respectively. The use of SPECT/CT in guiding patient selection for revision surgery offers several advantages in reducing patient morbidity and mortality, as well as economical and resource burden on the healthcare system.
352 - Outcomes in Robotic-Assisted Unicompartmental Knee Arthroplasty – the UK Experience

Amelia Tallents1, Daniel Blyth2, Nick Hancock2
1Southampton University, Southampton, United Kingdom. 2University Hospitals Southampton, Southampton, United Kingdom
Abstract
Background: Robotic unicompartmental knee arthroplasty (UKA) is a joint sparing surgery for the treatment of arthritis. It allows for preservation of the ligaments, aiding recovery following surgery. Prior to surgery, preoperative computer tomography (CT) scans are taken to enable robotic use. The literature highlights the success of robotics; however, a closer look is needed at the implementation of this in the field of knee surgery. This systematic review aims to appraise the most recent literature to assess the outcomes of robotic-assisted UKA compared to conventional techniques. A secondary aim was to focus on the relevance to the UK population.
Methodology: Medline, Embase and CINAHL databases were searched for studies relating to robotic-assisted knee arthroplasty. The search yielded 95 articles, 70 of which underwent title and abstract screening following duplicate removal. Six studies met the inclusion criteria. The data was extracted which included patient demographics, accuracy and functional outcomes.
Results: Ten articles were included in this systematic review, with four obtained through citation searching. One paper identified a learning curve of six cases for operating time and zero cases for precision. Implant alignment with robotic UKA was shown to produce higher precision in five papers. Three papers showed, on average, an additional 11.3% decrease in pain following robotic surgery compared to conventional.
Conclusions: Robotic-assisted UKA has been shown to be superior in all 3 of the anatomical planes; sagittal, coronal and axial alignment. It reduces outliers and is useful in education and training. However, early patient reported outcomes were equivalent to traditional jig-based surgery. Long-term results are more relevant in joint replacement surgery. Therefore, further randomised controlled trials and survivorship data is required. Nevertheless, the early results are no worse than that found with conventional surgery.
361 - Static vs Dynamic Fixation of Intracapsular Hip Fractures: A Comparison of Outcomes in 255 Patients
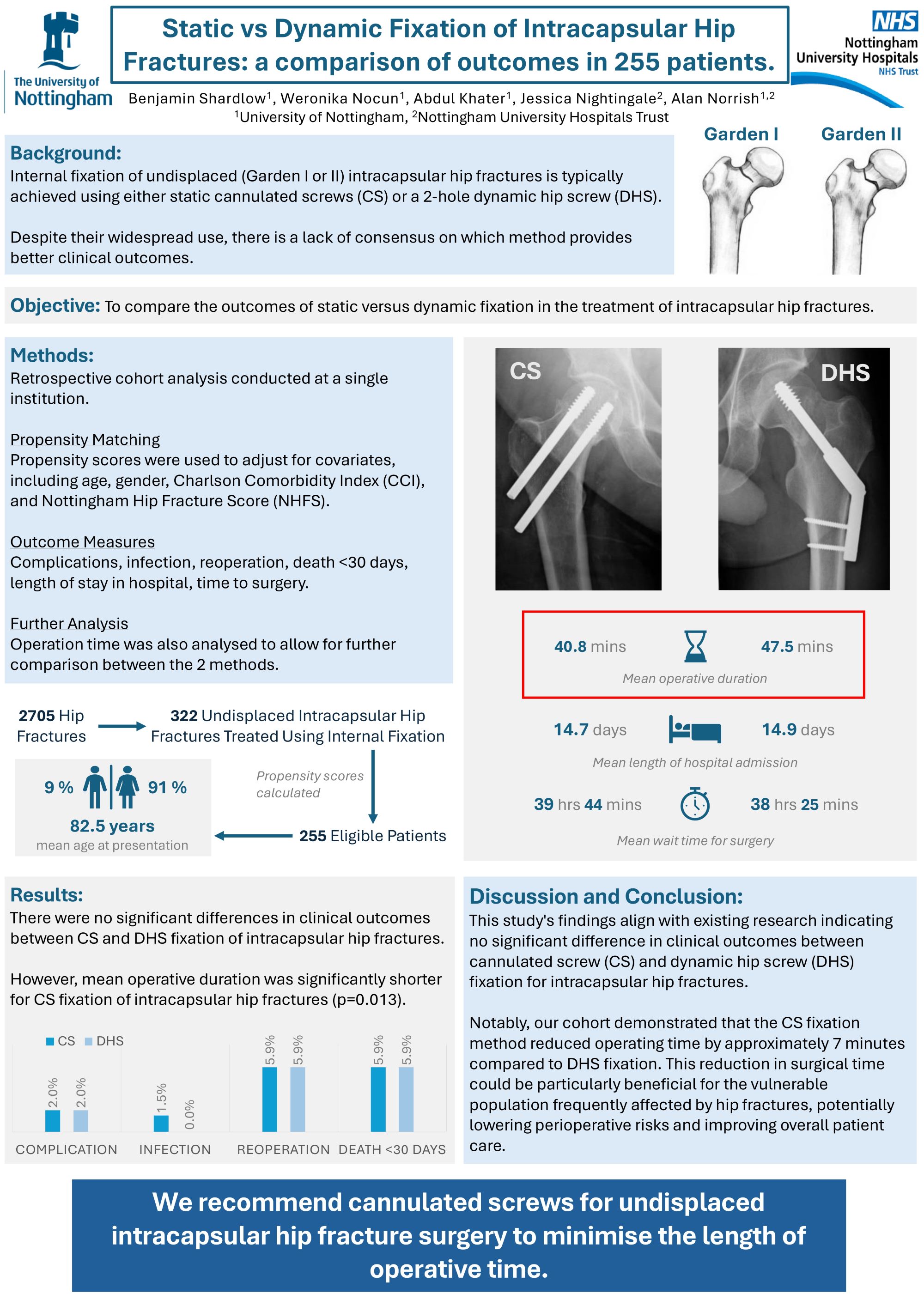
Ben Shardlow1, Weronika Nocun1, Abdhul Khater1, Jessica Nightingale2, Alan Norrish1,3
1University of Nottingham, Nottingham, United Kingdom. 2Nottingham University Hospital, Nottingham, United Kingdom. 3Nottingham University Hospitals, Nottingham, United Kingdom
Abstract
Background: Internal fixation of undisplaced intracapsular hip fractures is typically achieved using either static cannulated screws (CS) or a 2-hole dynamic hip screw (DHS). However, there is a lack of consensus on which of these is more effective clinically. Whilst several biomechanical analyses of cadaveric hips show a higher construct stability of DHS fixation, there is a paucity of large clinical studies investigating patient outcomes. This study aims to investigate clinical outcomes associated with these two approaches.
Methods: Data from 2705 patients at a single institution, including 322 internal fixations, were analysed retrospectively. Propensity scores were calculated to mitigate for the impact of covariates such as age, gender, Charlson Comorbidity Index (CCI) and Nottingham Hip Fracture Score (NHFS), producing an eligible group of 255 patients.
Results: The CS group included 204 patients (mean age 82.5±7.5, 91% female), and the DHS group included 51 patients (mean age 82.4±8.0, 90% female). There were no significant differences in complication rate (CS 2% vs DHS 2%, p=1.000), infection rate (CS 1.5% vs DHS 0%, p=1.000), reoperation rate (CS 5.9% vs DHS 5.9%, p=1.000), length of stay (CS 14.7±11.2 vs DHS 14.9±8.1 days, p=0.294), death <30 days (CS 5.9% vs DHS 5.9%, p=1.000), hours to surgery (CS 39:44±27:42 vs DHS 38:25±24:58 hrs, p=0.618). However, the operation time was significantly shorter for CS (CS 40.8±12.5 vs DHS 47.5±17.1 mins, p=0.013), a 14% reduction.
Conclusion: There is no difference in clinical outcomes between CS and DHS fixation of undisplaced intracapsular hip fractures. However, in this cohort the operating time was approximately 7 minutes shorter in CS fixation, which may represent a clinically important difference in this vulnerable group of patients.
Implications: We recommend CS for undisplaced intracapsular hip fracture surgery to minimise the length of operative time.
390 - Evaluation of Prophylactic Negative Pressure Wound Therapy Versus Standard Surgical Dressings on Wound Outcomes in Posterior Spinal Surgery Patients: A Systematic Review and Meta-Analysis
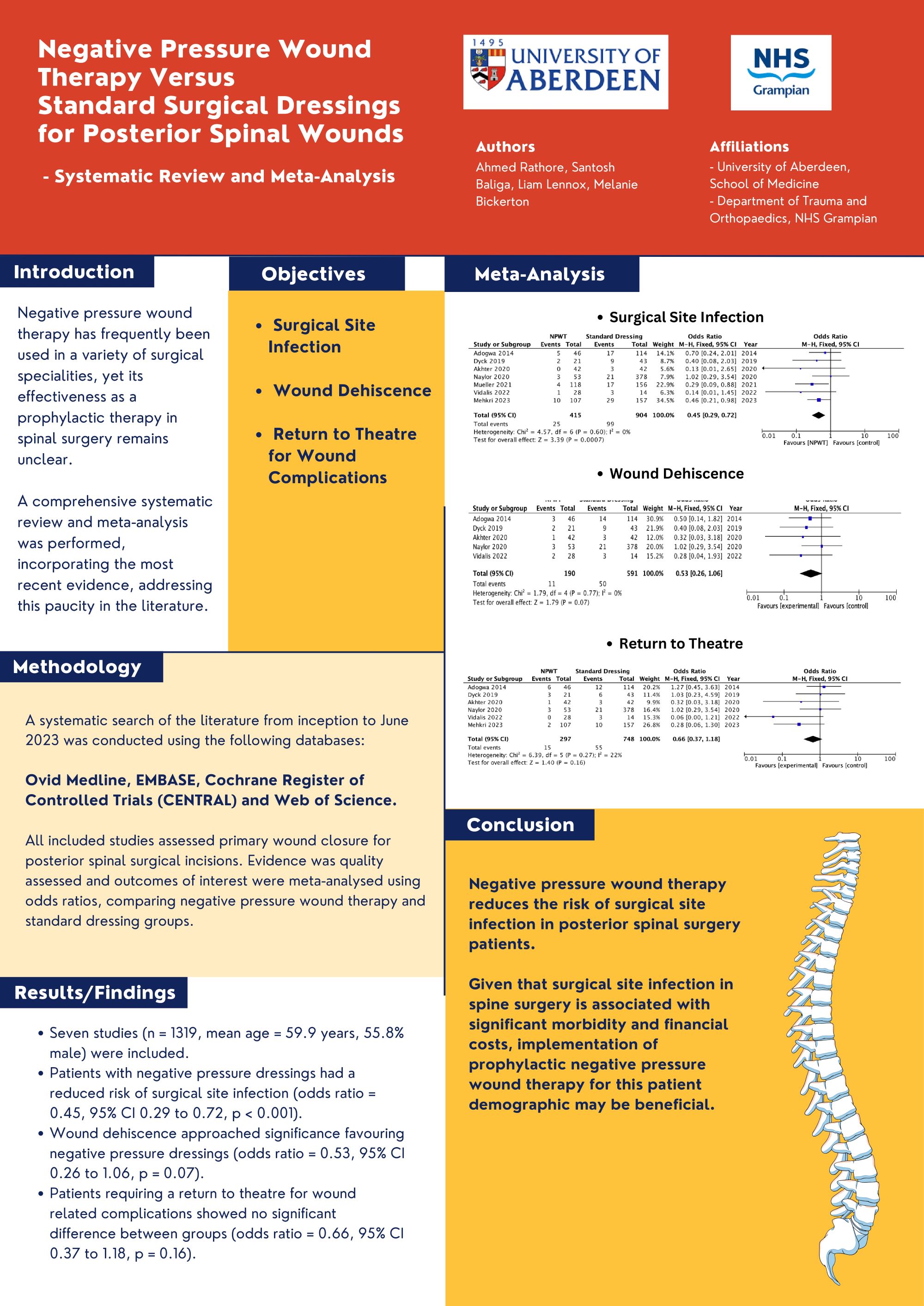
Ahmed Rathore1, Santosh Baliga2, Liam Lennox1, Melanie Bickerton1
1University of Aberdeen, Aberdeen, United Kingdom. 2NHS Grampian, Aberdeen, United Kingdom
Abstract
Background: Negative pressure wound therapy has frequently been used in a variety of surgical specialities, yet its effectiveness as a prophylactic therapy in spinal surgery remains unclear. A comprehensive systematic review and meta-analysis was performed, incorporating the most recent evidence, addressing this paucity in the literature.
Methods: A systematic search of the literature from inception to June 2023 was conducted using the following databases: Ovid Medline, EMBASE, Cochrane Register of Controlled Trials (CENTRAL) and Web of Science. All included studies assessed primary wound closure for posterior spinal surgical incisions. Evidence was quality assessed and outcomes of interest were meta-analysed using odds ratios, comparing negative pressure wound therapy and standard dressing groups.
Results: Seven studies (n = 1319, mean age = 59.9 years, 55.8% male) were included. Patients with negative pressure dressings had a reduced risk of surgical site infection (odds ratio = 0.45, 95% CI 0.29 to 0.72, p < 0.001). Wound dehiscence approached significance favouring negative pressure dressings (odds ratio = 0.53, 95% CI 0.26 to 1.06, p = 0.07). Patients requiring a return to theatre for wound related complications showed no significant difference between groups (odds ratio = 0.66, 95% CI 0.37 to 1.18, p = 0.16).
Conclusion: Negative pressure wound therapy reduces the risk of surgical site infection in posterior spinal surgery patients. Given that surgical site infection in spine surgery is associated with significant morbidity and financial costs, implementation of prophylactic negative pressure wound therapy for this patient demographic may be beneficial.
406 - Hemiarthroplasty Versus Total Hip Arthroplasty for Hip Fracture Patients That Meet the NICE Guidelines for Total Hip Replacement: A Comparison of Clinical Outcomes in 234 Patients
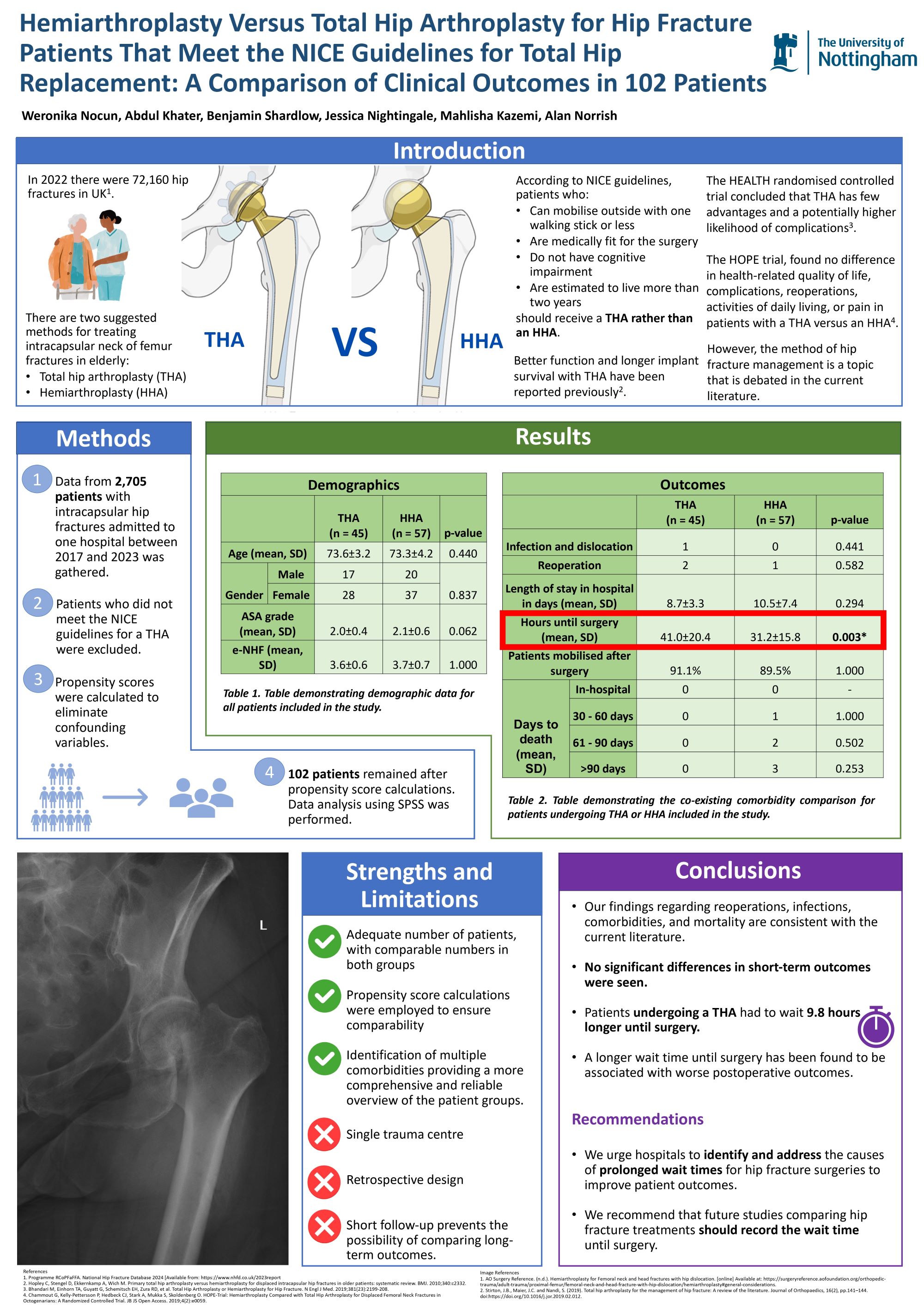
Weronika Nocun1, Adbul Khater1, Benjamin Shardlow1, Jessica Nightingale2, Alan Norrish1,2
1University of Nottingham, Nottingham, United Kingdom. 2Nottingham University Hospitals, Nottingham, United Kingdom
Abstract
Background: The treatment of displaced intracapsular hip fractures in mobile elderly patients without cognitive impairment is debated, with options including hip hemiarthroplasty (HHA) and total hip arthroplasty (THA). NICE guidelines suggest that THA is appropriate for many of these patients. However, sometimes logistical considerations make access to THA challenging. This study compares outcomes for a propensity-scored population who underwent HHA or THA.
Methods: Data from 2,705 patients with intracapsular hip fractures admitted to one institution between 2017-2023 was gathered and retrospectively analysed. Patients who had cognitive impairment or could not walk outdoors with no more than one walking aid were excluded. Propensity scores were calculated to eliminate confounding variables such as age, gender, ASA grade, and the Nottingham Hip Fracture Score. 234 patients remained after propensity score calculations.
Results: There were 141 patients in the THA group (mean age 72.8±4.3, 67% female) and 93 patients in the HHA group (mean age 73.9±4.2, 67% female). The infection and dislocation rate in the THA group was 1.4% versus 0% for the HHA, p=1.000. 3.5% of patients in the THA group had revision surgery versus 2.1% in the HHA group, p=0.706. The mean length of stay for patients in the THA group was 10.6±6.4 days versus 11.2±7.4 days for the HHA group, p=0.321. There was a significantly longer wait time for a THA (46.3±47.2 hours) versus HHA (30.4±15 hours), p<0.001. The mortality rate 90 days post-operation was 1.41% in the THA group compared to 3.2% in the HHA group, p=0.119.
Conclusion: All patients in this study had NICE-directed indications for a THA, and no significant differences in short-term outcomes were seen. However, patients undergoing THA had a significantly longer wait until surgery, which is a clinically important difference in the context of a painful hip.
437 - Enhancing Career Interest and Competency in Orthopaedics: The Impact of an Interactive Surgery Skills Day for Medical Students
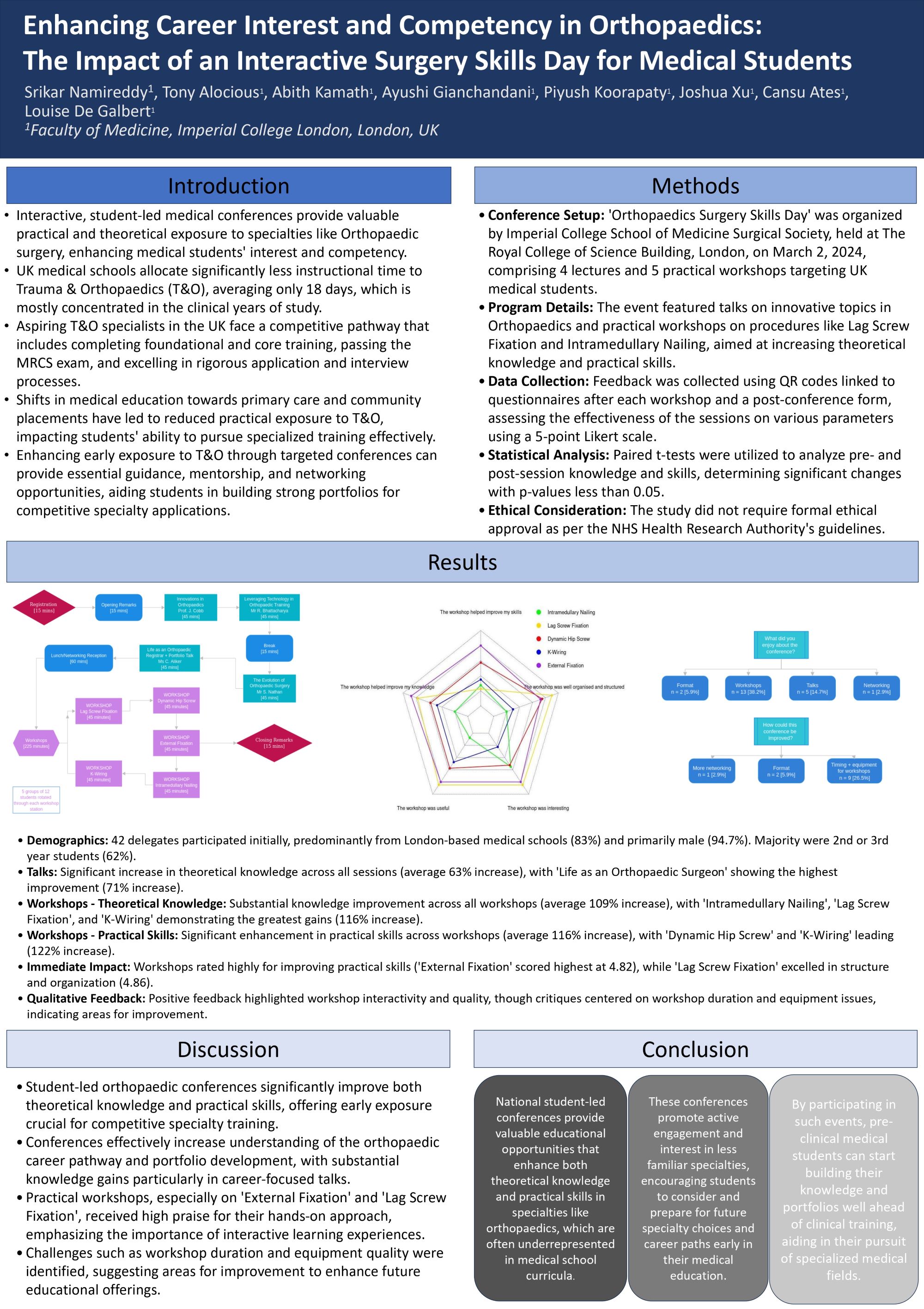
Srikar Namireddy, Piyush Koorapaty, Ayushi Gianchandani, Abith Kamath, Tony Alocious, Joshua Xu, Amelia Wild, Cansu Ates, Louise De Galbert
Imperial College School of Medicine, London, United Kingdom
Abstract
Background: The choice of specialty is a significant decision for medical students, influenced by various experiences throughout their education. Orthopaedic surgery, being highly technical, often benefits from practical exposure to attract potential specialists. This study evaluates the impact of a targeted Orthopaedic Surgery Skills Day, organized by the ICSM Surgical Society, on medical students' interest in the specialty as well as their theoretical knowledge and clinical competency.
Methods: The effectiveness of the conference was assessed through a post-conference questionnaire filled in by attendees, comprising 25 questions on their knowledge and skills. Additional data was collected using QR codes at each of the five workshops (k-wiring, ex-fix, DHS, lag screw, IM nailing). Data analysis was performed using SPSS and Excel to compare pre- and post-event competency levels, with statistical significance tested using u-tests.
Results: The event led to significant improvements in students' theoretical knowledge (average increase of 150%, p<0.001) and practical skills (average increase of 120%, p<0.001). Specifically, knowledge of 'Innovation in Orthopaedics' and 'Leveraging Technology in Orthopaedic Training' saw substantial gains, with increases averaging 4.7 points on a 10-point scale. IM Nailing and K-Wiring were the most successful workshops, seeing ~2-point average improvements on a 5-point scale. Furthermore, post-event, over 90% of attendees expressed a heightened interest in pursuing orthopaedics as a career.
Conclusion: The conference significantly improved medical students' theoretical knowledge and practical skills, affirming the value of hands-on, interactive learning environments. The marked improvements in knowledge and skills, validated by statistically significant results, highlight the effectiveness of such events in fostering medical specialization. This study supports the broader integration of practical and interactive educational approaches in medical training to guide and enhance student specialty choices.
484 - A Retrospective Study of Degenerative Cervical Myelopathy and the Surgical Management Within Northern Ireland.
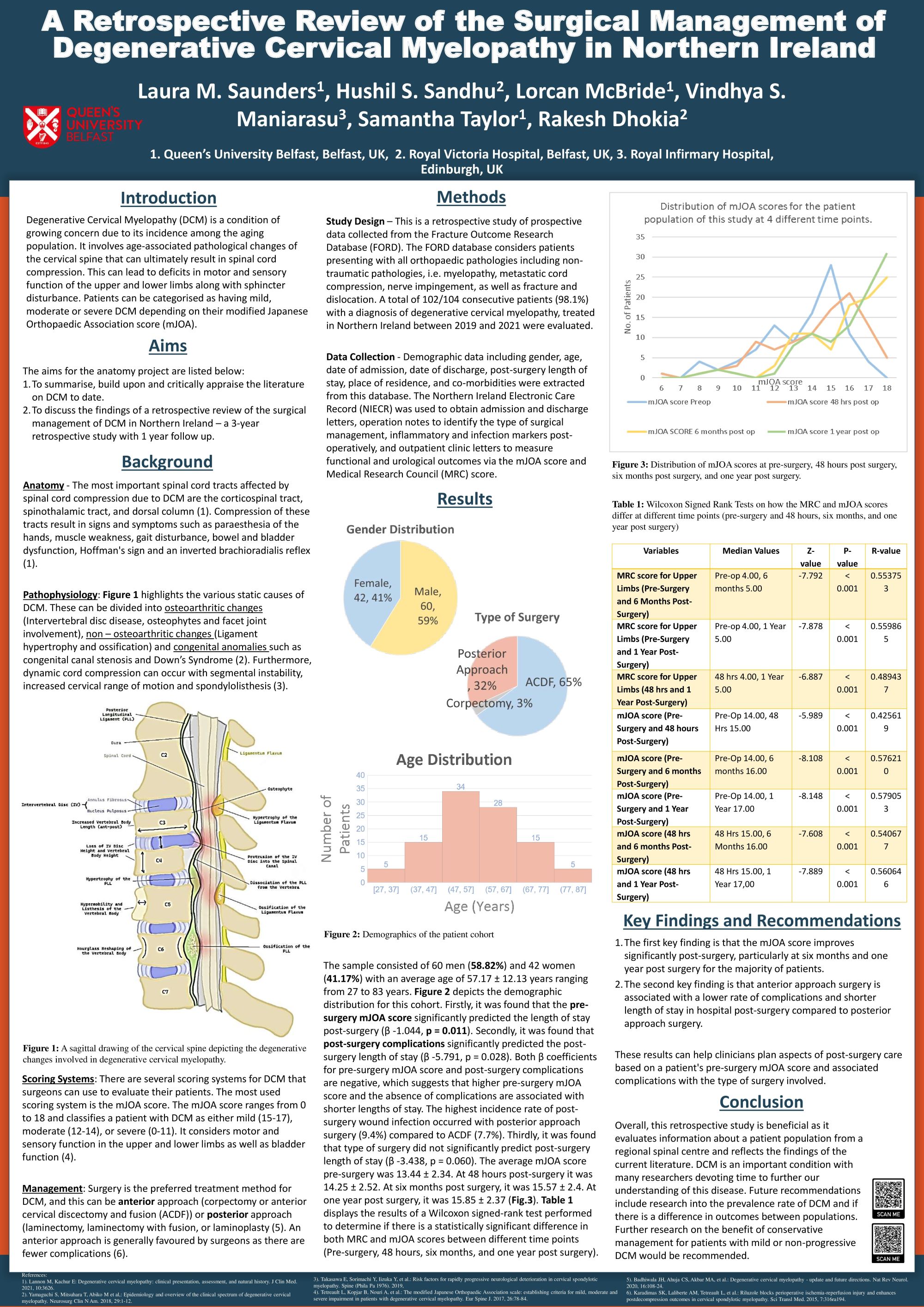
Laura Saunders1, Hushil Sandhu2, Lorcan McBride1, Vindhya Maniarasu3, Samantha Taylor1, Rakesh Dhokia2
1Queen's University Belfast, Belfast, United Kingdom. 2Royal Victoria Hospital, Belfast, United Kingdom. 3Royal Infirmary Hospital, Endiburgh, United Kingdom
Abstract
Introduction: Degenerative cervical myelopathy (DCM) is a condition of growing concern due to increasing incidence among the ageing population. It involves age-associated pathological changes of the cervical spine resulting in spinal cord compression. This can lead to deficits in motor and sensory function of the upper and lower limbs, issues with balance and dexterity, as well as bladder and bowel disturbance. Patients can be categorised as having mild, moderate, or severe DCM depending on their modified Japanese Orthopaedic Association (mJOA) score.
Methods: This is a retrospective study of the surgical management of DCM within the Regional Spinal Orthopaedic Unit in Northern Ireland over three years with one-year follow-up. 102 patients (10:7, male: female) with DCM were retrospectively evaluated. Exclusion criteria included patients diagnosed with spinal tumour, fracture, central cord syndrome, and dislocation. Key variables assessed were gender, age, symptoms, type of surgery, complications, MRC score, and mJOA score pre-surgery, 48 hours, six months, and one-year post-surgery.
Results: The sample consisted of 60 men (58.82%) and 42 women (41.17%) with an average age of 57.17 ± 12.13 years (27 to 83 years old). The statistical analysis explored the effect of time before and after surgery up to one year on the mJOA score. There was a significant difference in mJOA score pre-surgery and at six months and one-year post-surgery (R = 0.579053, p <0.001). Of the patients, 61.8% with a length of stay greater than three days and 71.4% of patients with a length of stay greater than seven days had a posterior approach surgery.
Conclusion: The first key finding is that the mJOA score generally improves after surgery, particularly at six months. The second key finding is that anterior approach surgery is associated with a lower rate of complications and shorter length of stay in hospital compared to posterior approach surgery.
495 - The mid-term clinical and radiological outcomes of stemless total shoulder replacement
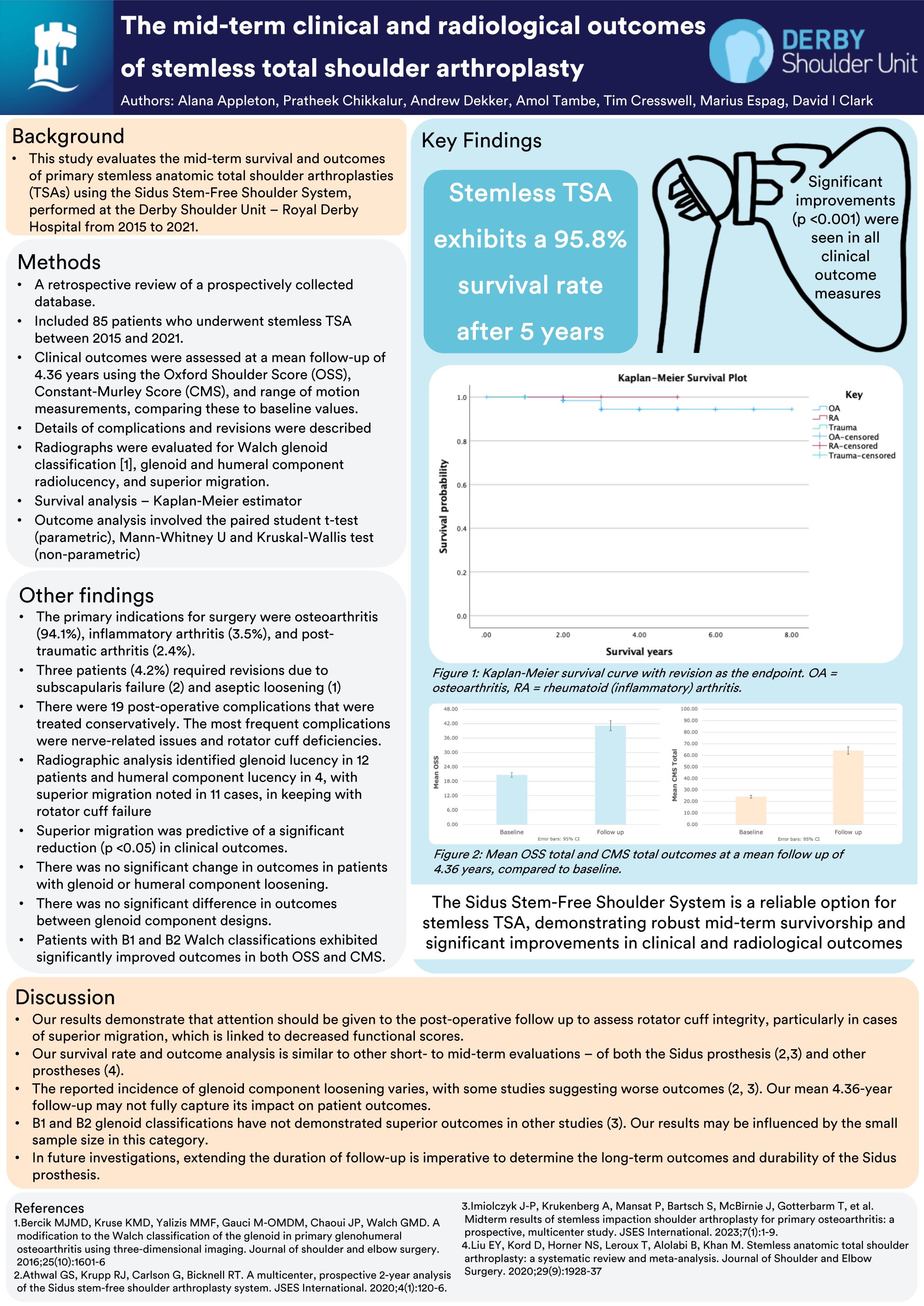
Alana Appleton1, David Clark2,1, Pratheek Chikkalur2, Andrew Dekker2, Amol Tambe2, Marius Espag2
1University of Nottingham, Nottingham, United Kingdom. 2UNIVERSITY HOSPITALS OF DERBY AND BURTON NHS FOUNDATION TRUST, Derby, United Kingdom
Abstract
Background: This study evaluates the mid-term survival and outcomes of primary stemless anatomic total shoulder arthroplasties (TSAs) using the Zimmer Biomet Sidus Stem-Free Shoulder System, performed at a single centre from 2015 to 2021.
Methods: We conducted a retrospective analysis of a prospectively collected database including 85 patients. Survival analysis was performed using the Kaplan-Meier method. Clinical outcomes were assessed at a mean follow-up of 4.36 years using the Oxford Shoulder Score (OSS), Constant-Murley Score (CMS), and range of motion measurements, comparing these to baseline values. Complications and revisions were recorded, and radiographs were evaluated for Walch glenoid classification, component radiolucency, and superior migration. Statistical analyses included the paired Student's t-test, Mann-Whitney U test, and Kruskal-Wallis test.
Results: The primary indications for surgery were osteoarthritis (94.1%), inflammatory arthritis (3.5%), and post-traumatic arthritis (2.4%). The Sidus prosthesis demonstrated a 95.8% survival rate at five years with revision surgery as the endpoint. Three patients (4.2%) required revisions due to subscapularis failure (2) and aseptic loosening (1). Clinical outcomes significantly improved (p < 0.001) from baseline to follow-up, with OSS increasing from 20.68 to 41.20, and CMS from 24.16 to 64.09. Radiographic analysis identified glenoid lucency in 12 patients and humeral component lucency in four, with superior migration noted in 11 cases. Superior migration was significantly associated with poorer outcomes (p < 0.05), although no correlation was found between component lucency and clinical outcomes.
Conclusions: The Sidus Stem-Free Shoulder System is a reliable option for stemless TSA, demonstrating robust mid-term survivorship and significant improvements in clinical and radiological outcomes. Attention should be given to the management of rotator cuff integrity, particularly in cases of superior migration, which is linked to decreased functional scores.
Disclosure: Educational contact with Zimmer Biomet is acknowledged for Mr. David Clark and Mr. Amol Tambe.
524 - Early to Medium Outcomes of Early Onset Scoliosis
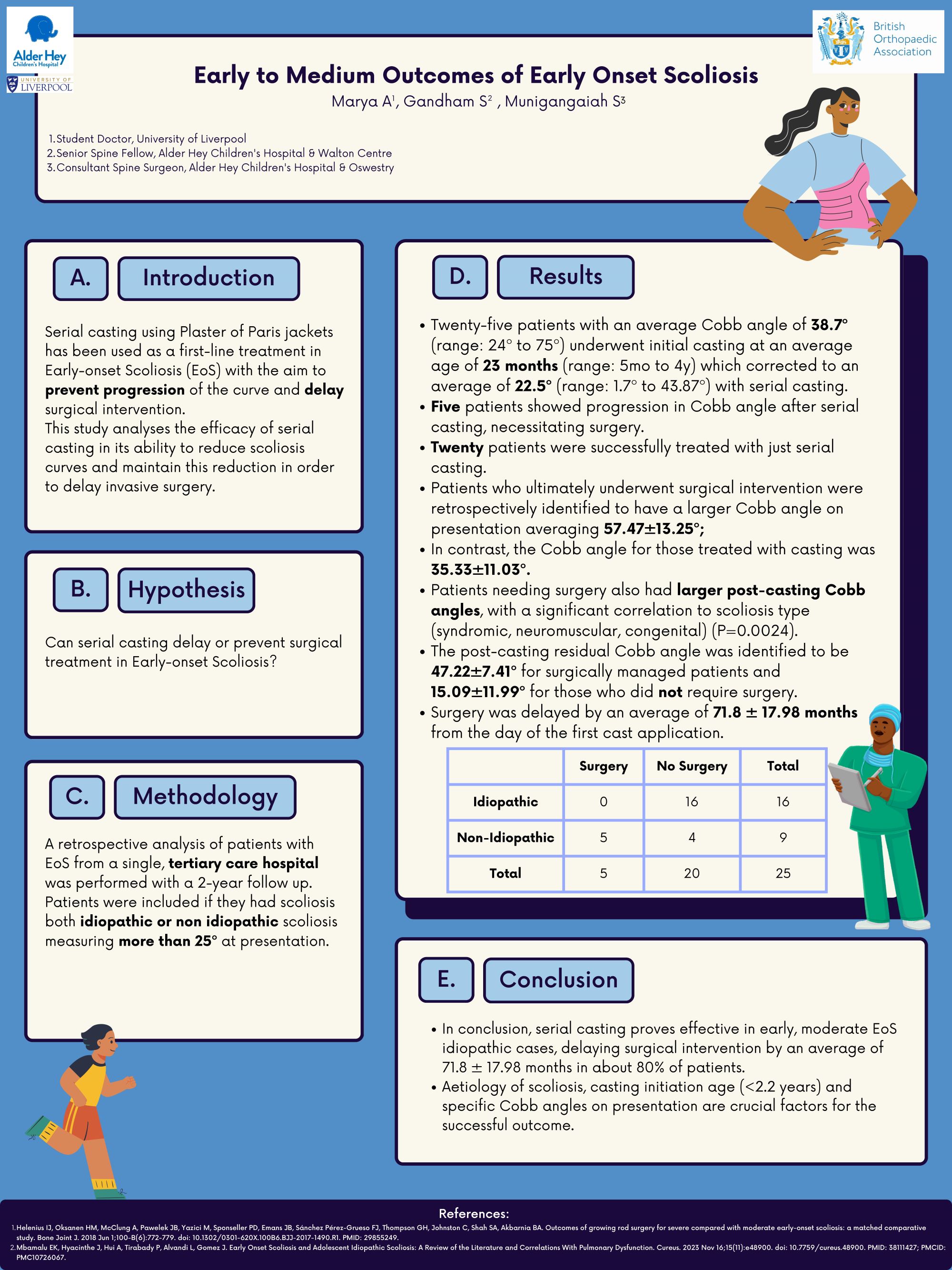
Archisha Marya1, Surya Gandham2, Sudarshan Munigangaiah2
1University of Liverpool, Liverpool, United Kingdom. 2Alder Hey Children's Hospital, Liverpool, United Kingdom
Abstract
Introduction: Serial casting using Plaster of Paris jackets has been used as a first-line treatment in Early-onset Scoliosis (EoS) with the aim to prevent progression of the curve and delay surgical intervention. This study analyses the efficacy of serial casting in its ability to reduce scoliosis curves and maintain this reduction in order to delay invasive surgery.
Methodology: A retrospective analysis of patients with EoS from a single, tertiary care hospital was performed with a 2-year follow up. Patients were included if they had scoliosis both idiopathic or non idiopathic scoliosis measuring more than 25º at presentation.
Results: Twenty-five patients with an average Cobb angle of 38.7º (range: 24º to 75º) underwent initial casting at an average age of 23 months (range: 5mo to 4y) which corrected to an average of 22.5º (range: 1.7º to 43.87º) with serial casting. Five patients showed progression in Cobb angle after serial casting, necessitating surgery. Twenty patients were successfully treated with just serial casting. Patients who ultimately underwent surgical intervention were retrospectively identified to have a larger Cobb angle on presentation averaging 57.47±13.25º; In contrast, the Cobb angle for those treated with casting was 35.33±11.03º. Patients needing surgery also had larger post-casting Cobb angles, with a significant correlation to scoliosis type (syndromic, neuromuscular, congenital) (P=0.0024). The post-casting residual Cobb angle was identified to be 47.22±7.41º for surgically managed patients and 15.09±11.99º for those who did not require surgery. Surgery was delayed by an average of 71.8 ± 17.98 months from the day of the first cast application.
Conclusions: In conclusion, serial casting proves effective in early, moderate EoS idiopathic cases, delaying surgical intervention by an average of 71.8 ± 17.98 months in about 80% of patients. Aetiology of scoliosis, casting initiation age (<2.2 years) and specific Cobb angles on presentation are crucial factors for the successful outcome.
539 - Circular frame in patients with in-situ arthroplasty - Is there an unacceptable risk of infection?
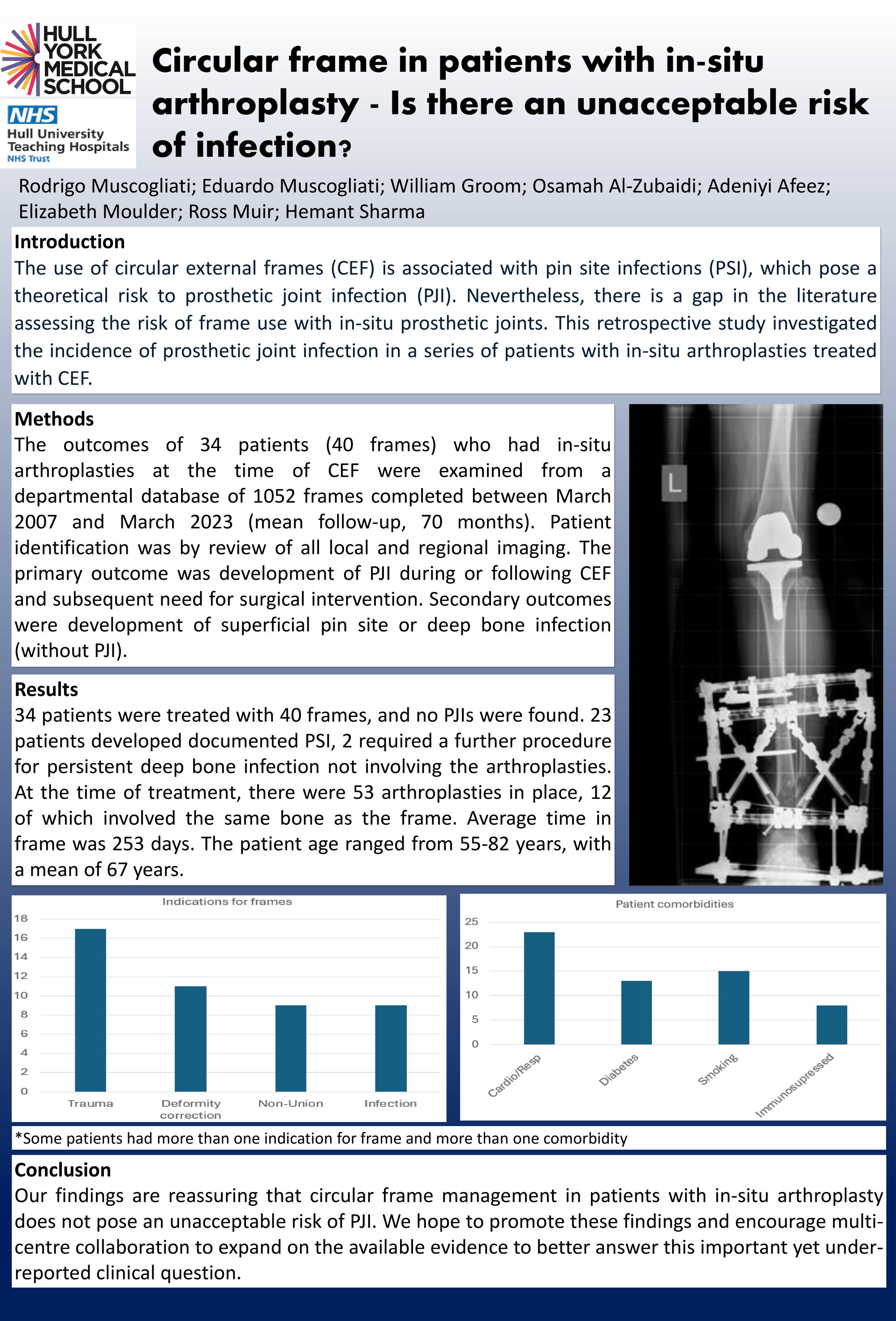
Eduardo Muscogliati1, Rodrigo Muscogliati1, William Groom2, Osamah Al-Zubaidi2, Adeniyi Afeez2, Elizabeth Moulder2, Ross Muir2, Hemant Sharma2
1Hull-York Medical School, Hull, United Kingdom. 2Hull University teaching hospitals, Hull, United Kingdom
Abstract
Background: The use of circular external frames (CEF) is associated with pin site infections (PSI), which pose a theoretical risk to prosthetic joint infection (PJI). Nevertheless, there is a gap in the literature assessing the risk of frame use with in-situ prosthetic joints. This retrospective study investigated the incidence of prosthetic joint infection (PJI) in a series of patients with in-situ arthroplasties treated with CEF.
Materials & Methods: The results of 34 patients (40 frames) who had in-situ arthroplasties at the time of CEF were examined from a departmental database of 1052 frames completed between March 2007 and March 2023 (mean follow-up, 70 months). Patient identification was by review of all local and regional imaging. The primary outcome was development of PJI during or following CEF and subsequent need for surgical intervention. Secondary outcomes were development of superficial pin site or deep bone infection (without PJI).
Results: 34 patients were treated with 40 frames, and no PJIs were found. 23 patients developed PSI, 2 required a further procedure for persistent deep bone infection not involving the arthroplasties. At the time of treatment, there were 53 arthroplasties in place, 12 of which involved the same bone as the frame. Average time in frame was 253 days. The patient age ranged from 55-82, with an average of 67. Of them, 8 were immunosuppressed, 15 smoked, 11 had diabetes, and 22 had cardio-respiratory illness.
Conclusion: Despite the small sample size, our findings are reassuring that circular frame management in patients with in-situ arthroplasty does not pose an unacceptable risk of PJI. We hope to promote these findings and encourage multi-centre collaboration to expand on the available evidence to better answer this important yet under-reported clinical question.
563 - Can the use of a novel alignment device significantly reduce radiation exposure in long bone fracture fixation using intramedullary nails?
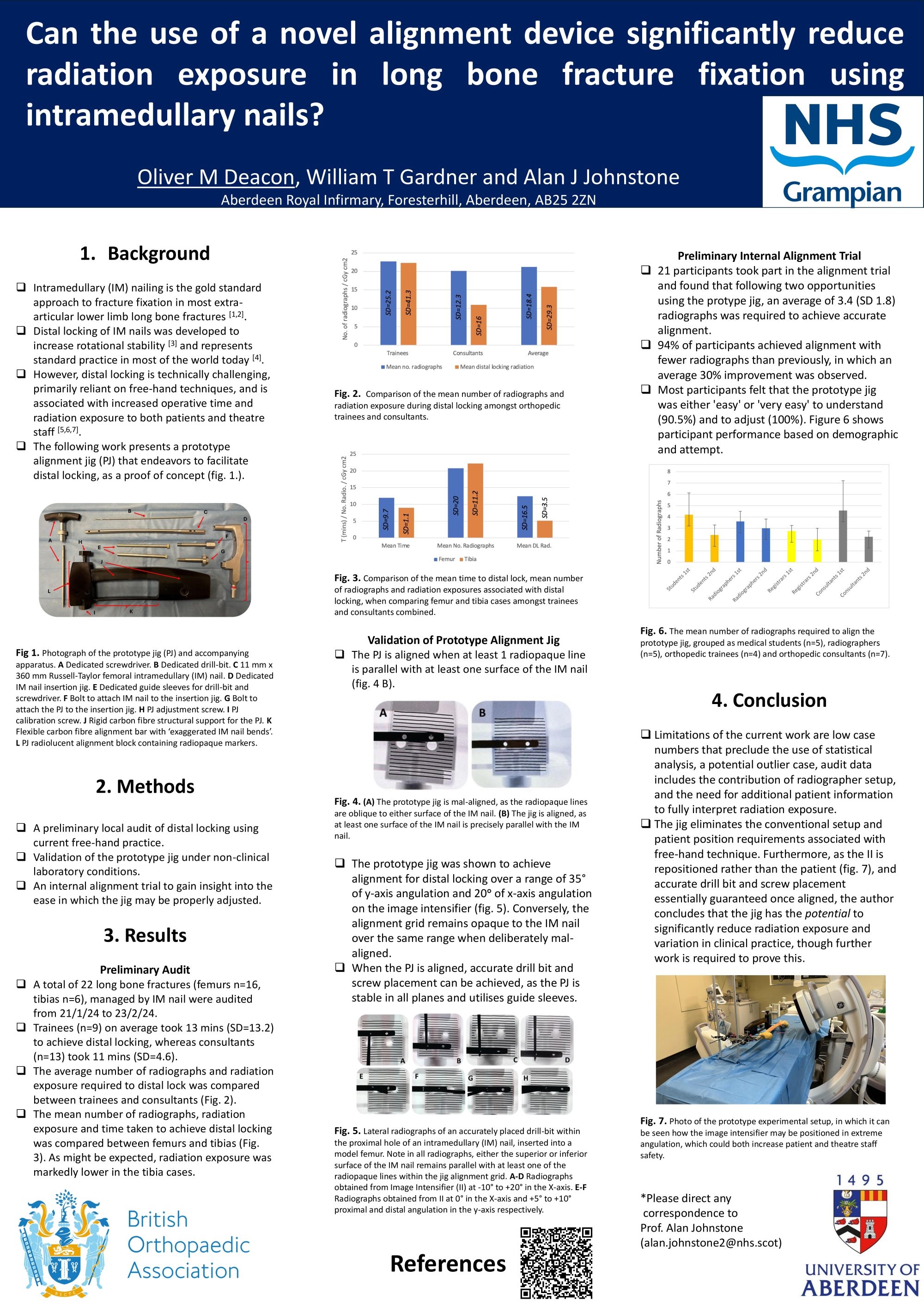
Oliver Deacon1,2, Tim Gardner2, Alan Johnstone2
1University of Aberdeen, Aberdeen, United Kingdom. 2Aberdeen Royal Infirmary, Aberdeen, United Kingdom
Abstract
Background: Intramedullary (IM) nailing is the gold standard approach to fracture fixation, in most extra-articular lower limb long bone fractures. Distal locking of IM nails was developed to increase rotational stability and represents standard practice in most of the world today. However, distal locking is technically challenging, primarily reliant on free-hand techniques, and is associated with increased operative time and radiation exposure to both patients and theatre staff. The following work presents a prototype alignment jig that endeavours to facilitate distal locking, as a proof of concept.
Methods: A preliminary local audit of distal locking using current free-hand practice. Validation of a protype alignment jig under non-clinical laboratory conditions, and an internal alignment trial to gain insight into the ease in which the jig may be properly adjusted.
Results: The average number of radiographs to distal lock using free-hand technique was 21.2 (SD 18.4), including radiographer setup and final confirmation of screw placement. The prototype jig was shown to achieve alignment for distal locking over a range of 35° of y-axis angulation and 20° of x-axis angulation on the image intensifier. 21 participants took part in the alignment trial and found that following two opportunities using the prototype jig, an average of 3.4 (SD 1.8) radiographs was required to achieve accurate alignment. Most participants felt that the prototype jig was either ‘easy’ or ‘very easy’ to understand (90.5%) and to adjust (100%).
Conclusion: As the jig eliminates the conventional setup and patient position requirements associated with the free-hand technique, and essentially guarantees accurate drill bit and screw placement once aligned, the author concludes that the jig has the potential to significantly reduce radiation exposure and variation in clinical practice. Thus, the jig has the potential to benefit patients and staff, whilst also improving theatre productivity through improved operative efficiency.
601 - Internal fixation vs hemiarthroplasty for intracapsular hip fractures in the elderly: a comparison of outcomes for 1018 matched patients
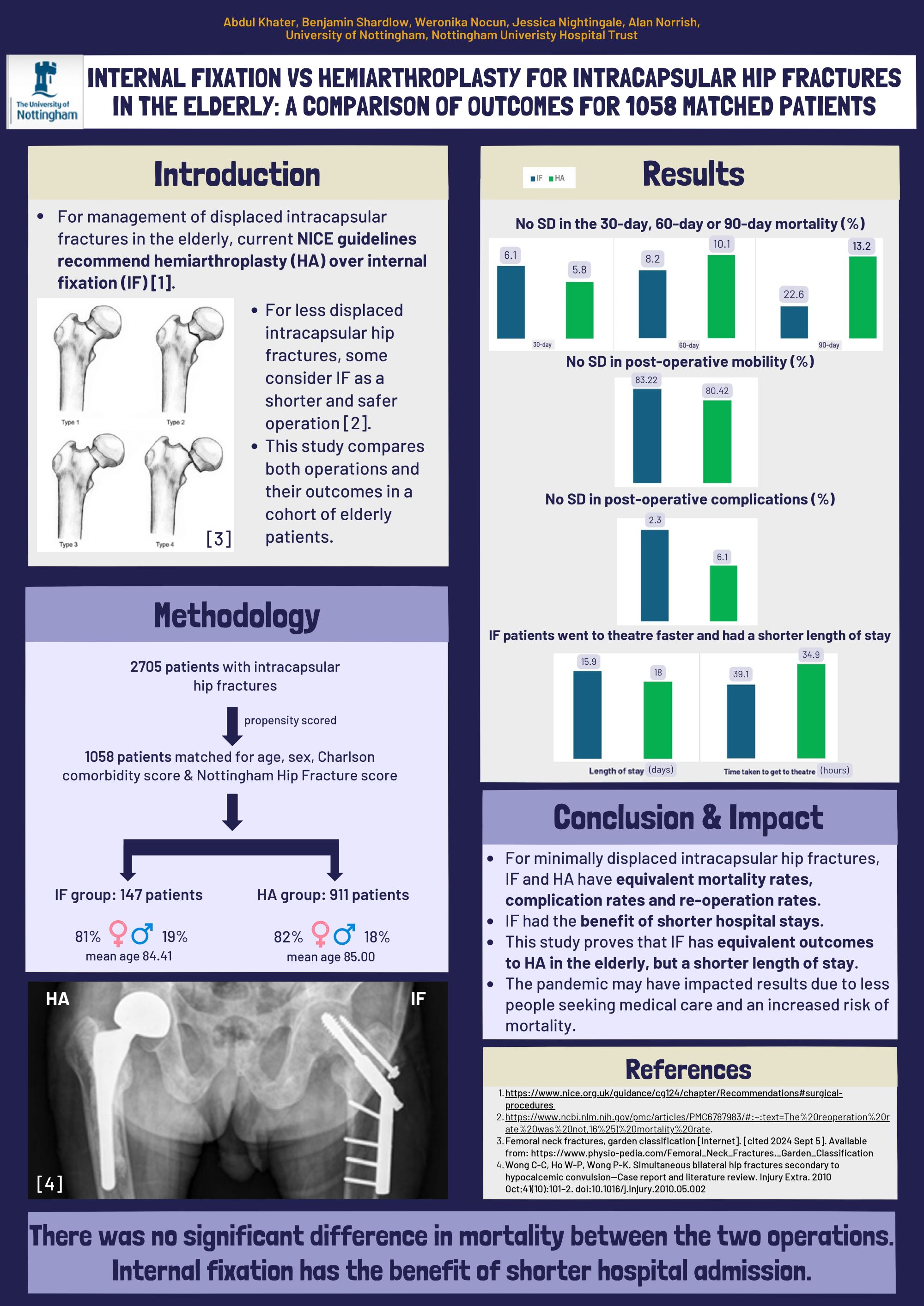
Abdul Khater1, Benjamin Shardlow1, Weronika Nocun1, Jessica Nightingale2, Alan Norrish2
1University of Nottingham, Nottingham, United Kingdom. 2Nottingham University Hospitals, Nottingham, United Kingdom
Abstract
Background: Current NICE guidelines recommend hemiarthroplasty (HA) over internal fixation (IF) for the management of intracapsular fractures in the elderly. Some consider IF as a shorter and safer operation for less displaced intracapsular hip fractures. This study aims to compare the treatment outcomes of both operations in a matched cohort of elderly patients.
Methods: Data from 2705 patients with intracapsular hip fractures were propensity scored to select a subset of 1018 patients to account for for age, sex, Charleson Comorbidity score and the Nottingham Hip Fracture score leaving 155 patients in the IF group (mean age 82.43 +/- 5.33 SD, 80.0% female) and 863 patients in the HA group (mean age 83.17 +/- 5.32 SD, 84.9% female).
Results: There was no significant difference in the 30-day (IF = 5.80%, HA = 4.52%, p=0.486), 60-day (IF = 7.74%, HA = 9.50%, p=0.802) or 90-day (IF = 10.32%, HA = 10.66%, p=0.900) mortality between HA and IF groups. There was also no significant difference in post-operative mobility (IF = 83.22% mobilised, HA = 80.42% mobilised, p=0.413). There was no significant difference in post-operative complications (IF = 3.23%, HA = 1.97%, p=0.194). On average, IF patients had a significantly shorter length of stay (IF = 14.67 days +/- 8.72 SD, HA = 17.10 +/- 12.45 SD, p=0.015).
Conclusion: Internal fixation for minimally displaced intracapsular hip fractures has equivalent mortality rates, complication rates and reoperation rates to a cohort of matched patients undergoing hip hemiarthroplasty. Internal fixation may have the advantage of allowing patients a shorter length of stay in hospital.
Impact: This study shows that internal fixation for minimally displaced fractures has equivalent outcome to hip hemiarthroplasty for minimally displaced hip fractures in the elderly, but a shorter length of stay.
615 - Adjuvant local antibiotic prophylaxis in GA IIIb open fractures: Follow-up of outcomes over the last decade
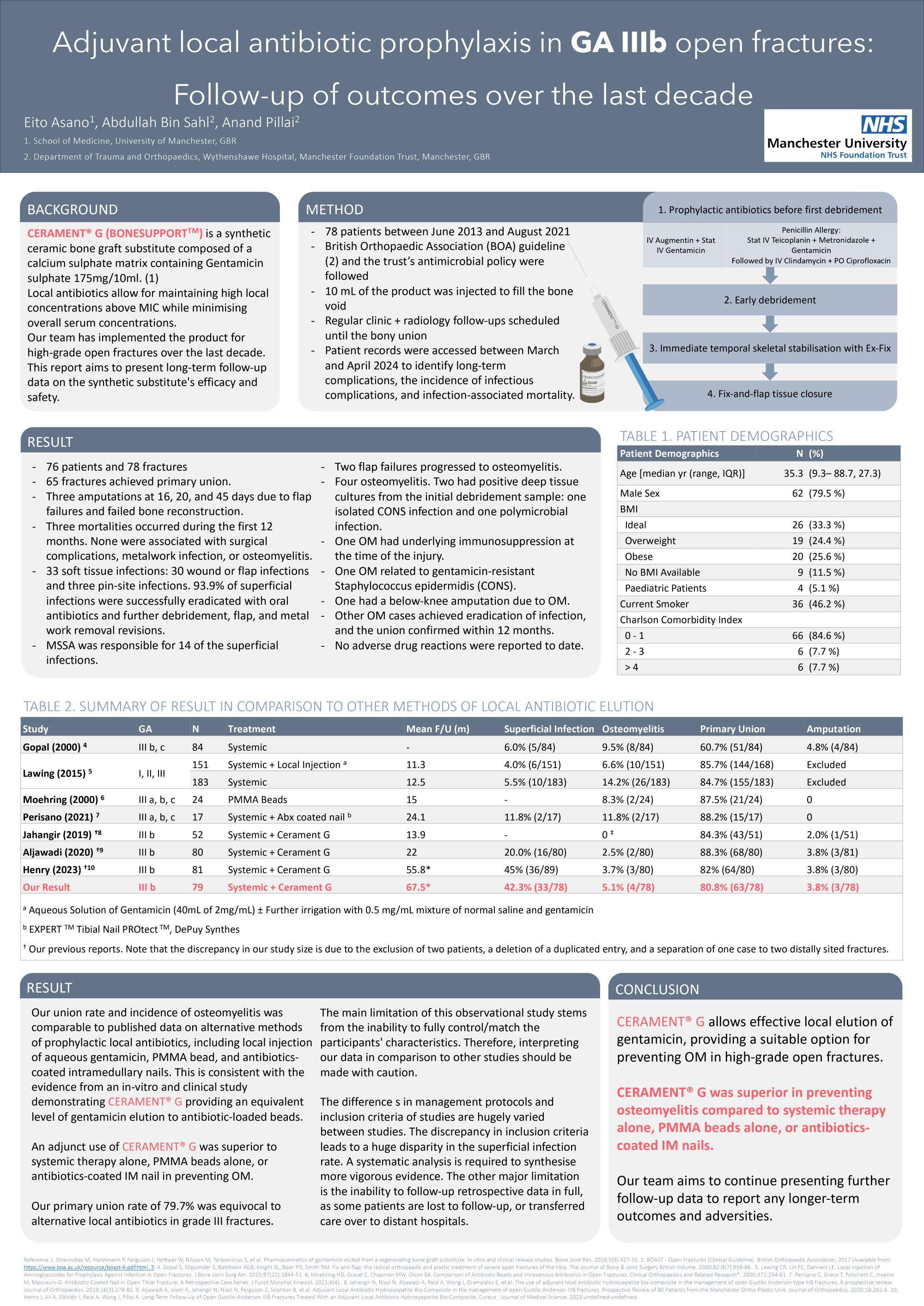
Eito Asano1, Abdullah Bin Sahl2, Pillai Anand2
1University of Manchester, Manchester, United Kingdom. 2Manchser Universtiy NHS Foundation Trust, Manchester, United Kingdom
Abstract
Background: High-grade open fractures carry a devastating risk of osteomyelitis despite advancements in techniques and treatment protocols. The use of prophylactic, adjuvant local antibiotics is controversially discussed in the literature. CERAMENT® G (BONESUPPORT TM) is a novel synthetic bone substitute that provides an effective elution of gentamicin. The aim of this report is to present the latest follow-up data collected over the last decade and compare them against our previous findings and existing literature.
Methods: A retrospective, descriptive analysis of all patients sustaining GA IIIb fracture who received CERAMENT® G in addition to the conventional fix and flap approach between June 2013 to August 2021. Patient demographics, orthoplastic interventions, microbiology reports, and latest outcome data including union, infection, mortality, and amputation were extracted from electronic records to April 2024.
Results: A total of 76 patients with 79 fractures were included with a mean follow-up period of 67.5 months since the operation and the review period. The primary union was achieved in 63 fractures (79.7%). The secondary union was achieved following bone graft in 5 out of 15 non-union cases. Three fractures were associated with mortality. Four fractures required amputation. Indications included osteomyelitis, flap failure leading to soft tissue infection, failure in bone reconstruction, and chronic pain. Superficial infections occurred in 34 fractures (43.0%). Osteomyelitis occurred 4 fractures (5.1%) at a mean of 270.8 days. There were no reported local or systemic adverse reactions to the product to date.
Conclusion: In adjunct to systemic antibiotic prophylaxis, CERAMENT ® G provides a safe option for local antibiotics in high-grade open fractures. This is an interim result. Figures may vary in the final report.
641 - Coronal Plane Alignment of the Knee (CPAK) Distribution in a Diverse Asian Population: Influence of Ethnicity, Sex, and Bilaterality
Azmi Rahman1, Lenice Tan2, Sabine Wong2, Merrill Lee3, Seng Jin Yeo3
1University of Oxford, Oxford, United Kingdom. 2National University of Singapore, Singapore, Singapore. 3Singapore General Hospital, Singapore, Singapore
Abstract
Background: In total knee arthroplasty (TKAs), it remains unclear which patients benefit from correction vs restoration of native knee alignment. The Coronal Plane Alignment Knee (CPAK) classification system was introduced in 2021 to describe native knee alignment, to improve characterisation of the effect of different TKA alignment techniques. This study aims to describe CPAK in an ethnically diverse population, and characterise the relationship between CPAK and ethnicity, bilaterality of OA, and other patient factors.
Methods: 503 primary TKAs were performed in a large tertiary institution in Singapore from 2014-2021. Pre-operative anteroposterior knee radiographs were collected for 441 procedures - all had ethnicity, age, sex, and BMI data. The medial proximal tibial angle (MPTA) and lateral distal femoral angle (LDFA) were measured with excellent inter-observer correlation. Knees were then classified into 9 CPAK categories based on arithmetic hip-knee-ankle (aHKA) angle and joint-line obliquity (JLO).
Results: 77% of cohort were apex-distal (CPAK-1,2,3) and 59% were varus (CPAK-1,4,7); 44% were CPAK-1 (varus + apex-distal). Distributions did not vary between sexes or across BMI (p=0.156, p=0.355). Chinese and Indian knees followed near identical patterns: CPAK-1(46%) > CPAK-2(20%) > CPAK-4(15%). Malay knees had significantly fewer CPAK-1 (p=0.0183), with CPAK-1(29%) ≈ CPAK-2(29%) ≈ CPAK-4(21%). 38 patients had bilateral TKA. Identical categories were recorded bilaterally in 45% for CPAK, 67% for JLO, and 70% for aHKA. Bilateral TKA were more likely when knees were in valgus alignment, than unilateral TKA (p=0.00457).
Conclusion/Implications: Ethnicity is a factor influencing CPAK, and Malay knees are less likely to be CPAK-1; this is a novel finding and may explain ethnic differences in TKA outcomes described in literature. Bilateral TKA was more likely to be performed in valgus knees, but only 45% had the same CPAK category bilaterally. The implications of this bilateral CPAK congruence is unclear and requires further study.
750 - Improving undergraduate medical students' confidence in interpreting multimodal orthopaedic and whole-body cross-sectional imaging by teaching normal radiological anatomy
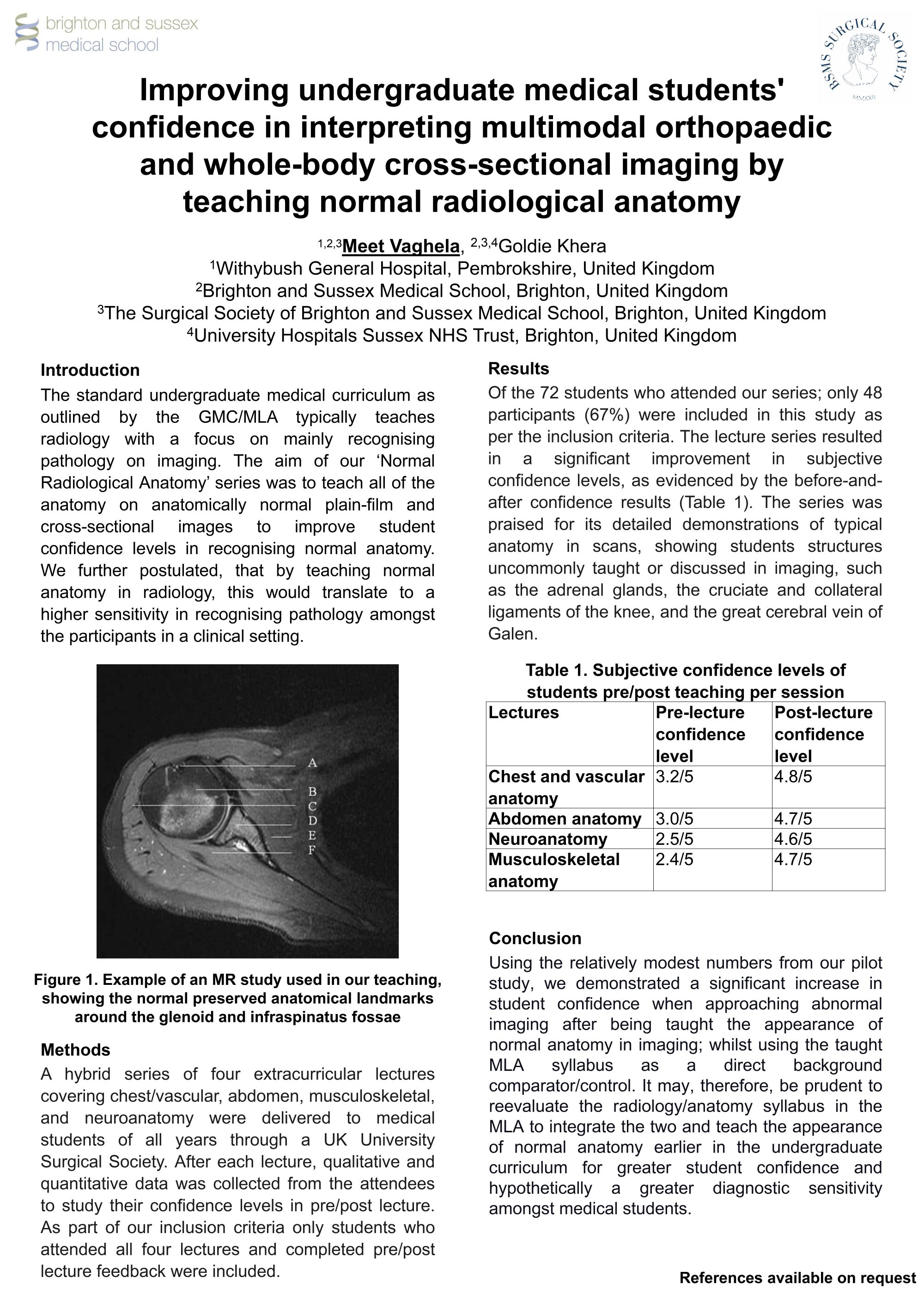
Meet Vaghela1,2,3, Goldie Khera4,2,3
1Withybush General Hospital, Pembrokshire, United Kingdom. 2Brighton and Sussex Medical School, Brighton, United Kingdom. 3The Surgical Society of Brighton and Sussex Medical School, Brighton, United Kingdom. 4University Hospitals Sussex NHS Trust, Brighton, United Kingdom
Abstract
Background: Our educational series teaching normal radiological anatomy was designed to offer a more comprehensive understanding of scans. Our approach involved identifying and teaching all anatomical structures visible in common plain-film and cross-sectional imaging, similar to illustrated anatomy textbooks. This differs from the typical radiology curriculum offered as part of the GMC/MLA program, where mostly pathology and relevant landmarks are discussed.
Methods: Delivered through a UK University Surgical Society, a series of four voluntary, extracurricular lectures covering orthopaedic, chest/vascular, abdomen, and neuroanatomy, were delivered in a hybrid in-person/virtual format for medical students. Following the lectures, a survey consisting of seven questions was distributed to the students.
Results: In total, 72 students participated in at least one lecture. However, we only considered feedback forms from individuals who attended all four lectures and provided feedback on each. With this inclusion criteria, we were able to include 48 individuals, representing 67% of all attendees. Prior to attending the lecture series, the average subjective confidence level in interpreting scans was 2.6/5. According to the feedback received after attending the series, the overall subjective confidence increased to 4.8/5. The series was praised for its detailed demonstration of normal anatomy in scans; showing students rarely taught/discussed structures in imaging at the undergraduate level such as the cruciate ligaments of the knee and the tendons of the rotator cuff on MRI.
Conclusions: Rather than following the traditional approach of teaching students to identify pathology in imaging, our series suggests that it may be more effective to train students in recognising normal anatomy on scans. This approach not only bolstered student confidence when working with pathological imaging, but we hypothesise it also potentially enhances their ability to identify pathology on scans by making them more familiar with the appearance of normal anatomy.
754 - The Impact of COVID-19 on Presentation to Urgent Care Services in Those Awaiting Elective Orthopaedic Surgery: An Interrupted Time Series Analysis
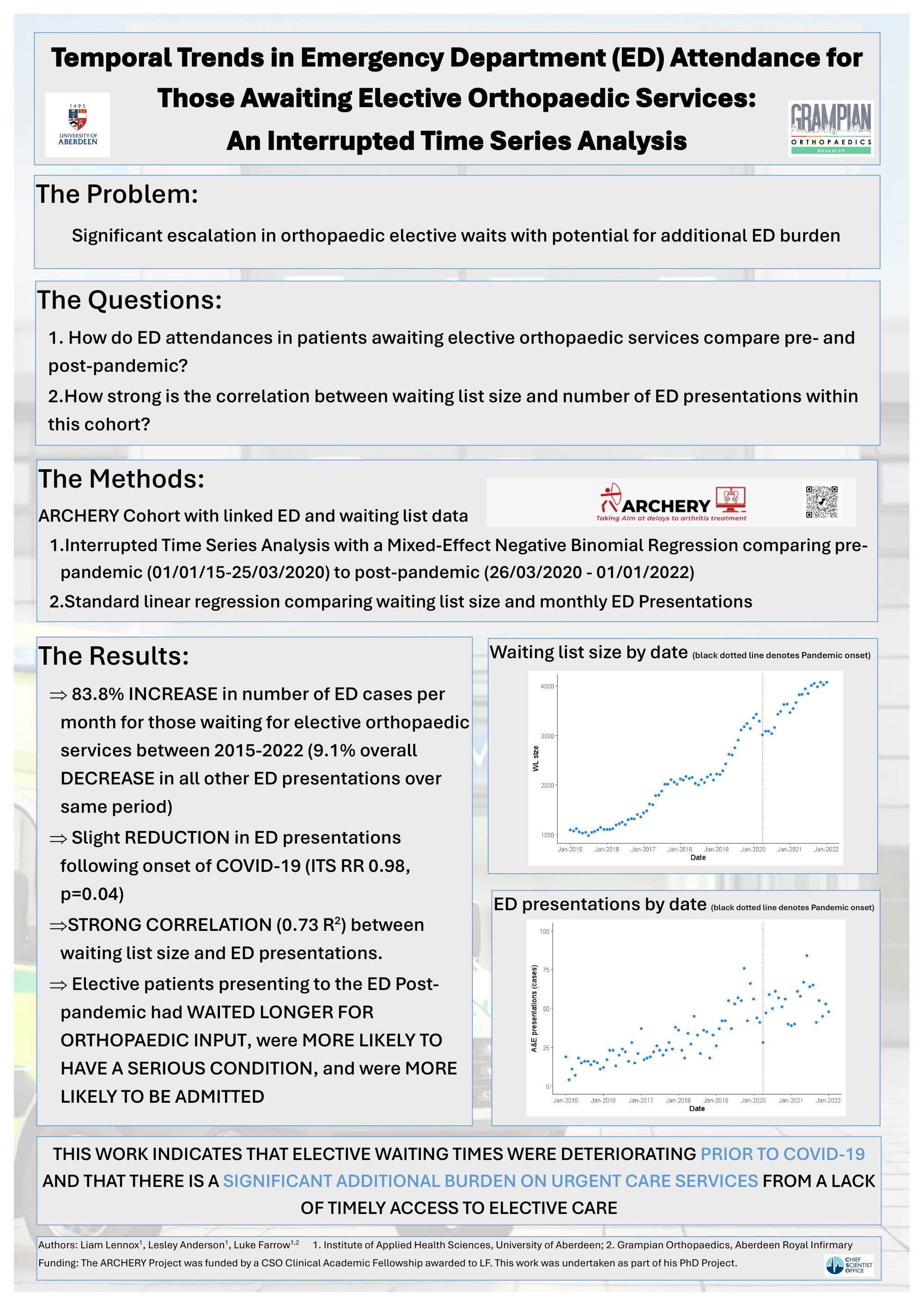
Liam Lennox1, Lesley Anderson1, Luke Farrow1,2
1University of Aberdeen, Aberdeen, United Kingdom. 2Grampian Orthopaedics, Aberdeen, United Kingdom
Abstract
Introduction: Waiting times have appeared to significantly escalate coronavirus-19 (COVID-19) pandemic, with an associated detrimental impact on health and wellbeing. One potential unforeseen consequence of this is additional emergency care burden whilst waiting for surgery. We therefore set out to determine if there was any direct link between COVID-19 and subsequent presentation of patients waiting for elective orthopaedic surgery to urgent care services.
Methods: An interrupted time series analysis was conducted using linked routinely collected data from a single region in Scotland. Only patients on the in-patient elective orthopaedic waiting list between January 2015 and January 2022 were included. Initiation of the COVID-19 pandemic was determined to be the 26th of March (when Scotland entered its first national lockdown). Mixed-effect negative binomial regression (interrupted time series analysis [ITS]) was undertaken to determine if COVID-19 was associated with changes to the number and rate of presentations to ED services.
Results: 8155 patients were identified as waiting for orthopaedic surgery at some point during the data collection period, of which 2031 recorded a presentation to the ED (25%). Patients who presented to the ED post-COVID-19 spent longer in the ED, were triaged as more serious conditions and more likely to be admitted. Post-COVID-19 twice as many presentations to A&E occurred (RR (95% CI) 2.02 (1.89 to 2.15); p < 0.001), this was not however significantly associated with the onset of the pandemic according to the ITS (Relative Risk 0.96, Standard Error 0.60, p=0.11).
Conclusions: The number of patients waiting for surgery and associated presentations to urgent care services have risen massively since the COVID-19 pandemic. However, both of these factors were already deteriorating before the pandemic began, and therefore current pressures appear to be the result of long-term inadequacies in funding and service provision rather than the isolated impact of COVID-19.
787 - Length of Stay Following Total Hip Arthroplasty. A Comparative Audit of Patients Under 55 Years Versus Over 55 Years with ASA Grades 1 & 2; Factors Most Influencing Length of Stay

Benjamin Hee1, Max Mulligan1, Sabri Bleibleh2, Gayle Kwidini2
1University of Birmingham Medical School, BIRMINGHAM, United Kingdom. 2Royal Orthopaedic Hospital Birmingham, Birmingham, United Kingdom
Abstract
Background: Total hip arthroplasty (THA) is a common surgical procedure, but factors affecting post-operative length of stay (LOS) remain unclear, particularly in patients under 55 years of age versus those over 55. Furthermore, recognising that current care pathways are largely based on the needs of the older patient, the authors wanted to explore whether specific needs of the younger patient were also met.
Methods: A retrospective cohort analysis of 50 patients who undertook an elective THA at the Royal Orthopaedic Hospital from 2021 to 2023 was conducted. All patients were ASA grade 1 or 2. Baseline characteristics and audit criteria information were collected and analyzed via statistical analysis.
Results: There was no significant difference in LOS between age groups, average LOS in over 55s were found to be at 2.68 days while under 55s were at 2.56. In patients over 55, BMI, pain scores, and oral opioid administration correlated positively with LOS. Conversely, no variables significantly correlated with LOS in patients under 55. Notably, the under 55 cohort had more documented problems mobilising than the over 55 cohort, with 91% of them being syncope/hypotension in the under 55 group.
Conclusion: Effective pain management and BMI control may reduce LOS in THA patients over 55 with ASA grades 1 & 2. Optimizing pain control strategies and encouraging healthy BMI could expedite recovery, suggesting the need for personalized care approaches in this population. Further research into adverse effects experienced by the younger age group, particularly regarding problems mobilizing, could help optimize rehabilitation pathways for this demographic due to their more homogenous distribution of issues. Further research with larger cohorts is warranted to validate these findings and explore additional determinants of post-THA recovery.
Paediatrics - Poster Abstracts
653 - Improving sustainability in paediatric orthopaedic day case surgery: A pilot study
Gemma Green, Anthony Yiu, Matthew Baker, Chun Tang, Jo Dartnell, Marcos Katchburian, Gregory Firth
Maidstone and Tunbridge Wells NHS Trust, Tunbridge Wells, United Kingdom
Abstract
Background: In the NHS 156,000 tonnes of clinical waste are incinerated each year, producing 4% of England’s overall carbon emissions and 40% of public sector emissions. Streamlining and reducing clinical waste is key both environmentally and financially for NHS trusts. Volume of waste generated in paediatric orthopaedic day case theatres is unacceptable. We aim to reduce economic and environmental costs by using streamlined sets and drapes.
Methods: Paediatric orthopaedic day cases in one centre were identified between 1 April 2023 and 31 March 2024. Environmental costs of cleaning the standard minor orthopaedic tray as well as incinerating clinical waste generated per case was calculated using weight and published UK emissions data.Sets were scrutinised, and surplus instruments removed. Reduced draping was identified with the trust sustainability team. The cost of sterilisation was calculated using data from IHSS and NHS published costs.
Results: 94 eligible procedures were included. Sterilisation costs for the current sets were £40 compared to £25 for streamlined sets. Financial saving £1410. Total incineration costs of current drapes (1717g) were £81 compared to £2 for reduced drapes (44g). Financial saving £1489. Environmentally, the cost of incinerating current drapes was 173.34kgCO2e /year, compared to 4.4kgCO2e/year for reduced drapes. Combining this with the emissions produced in cleaning sets (254.34 kg/ year current, 106kg/ year streamlined), the carbon emissions saved by streamlining was 317.28kgCO2e/year .
Conclusion/Findings: Current practice in paediatric day case surgery is generating excess waste, with both financial and environmental implications. Streamlining trays, and reducing drapes can save £1500 per year, and more than halve carbon emissions produced. Extrapolating to other areas of orthopaedics, would further enhance this saving.
Implications: Small changes in practice can collectively make a substantial difference to our environment.
Quality Improvement - Poster Abstracts
49 - A Novel, Cost-effective and Easily Reproducible Simulation Method for Teaching Fascia Iliaca Blocks Significantly Improves Peri-operative Administration Rates in NOF Fracture Patients
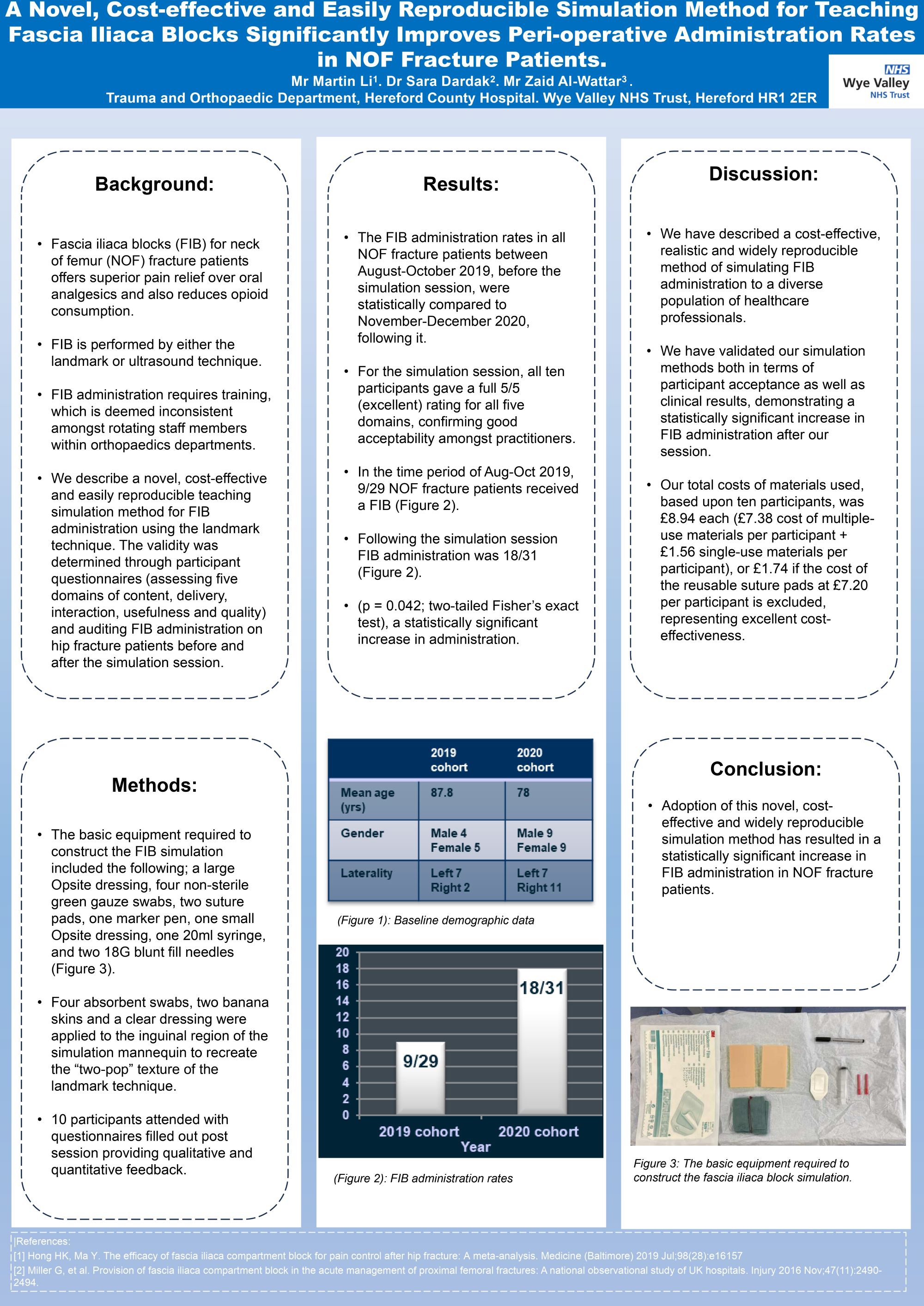
Martin Li1,2, Sara Dardak3,2, Zaid Al-Wattar2
1Birmingham Women's and Children's NHS Foundation Trust, Birmingham, United Kingdom. 2Hereford County Hospital, Hereford, United Kingdom. 3William Harvey Hospital, Ashford, United Kingdom
Abstract
Background: Fascia iliaca blocks (FIB) for neck of femur (NOF) fracture patients offers superior pain relief over oral analgesics and also reduces opioid consumption. FIB is performed by either the landmark or ultrasound technique. FIB administration requires training, which is deemed inconsistent amongst rotating staff members within orthopaedics departments. We describe a novel, cost-effective and easily reproducible teaching simulation method for FIB administration using the landmark technique. The validity was determined through participant questionnaires (assessing five domains of content, delivery, interaction, usefulness and quality) and auditing FIB administration on hip fracture patients before and after the simulation session.
Methods: Four absorbent swabs, two banana skins and a clear dressing were applied to the inguinal region of the simulation mannequin to recreate the “two-pop” texture of the landmark technique. 10 participants attended limited by social distancing due to Covid-19 with questionnaires filled out post session providing qualitative and quantitative feedback. The FIB administration rates in all NOF fracture patients between August-October 2019, before the simulation session, were statistically compared to November-December 2020, following it.
Results: For the simulation session, all ten participants gave a full 5/5 (excellent) rating for all five domains, confirming good acceptability amongst practitioners. In the time period before the session, 9/29 neck of femur fracture patients received a FIB, improving to 18/31 patients following it (p = 0.042; two-tailed Fisher’s exact test), a statistically significant increase in administration. The average cost per participant for the single-use materials in the session was £1.56, whereas the multiple-use items costed £7.88 per participant.
Conclusion: Adoption of this novel, cost-effective and widely reproducible simulation method has resulted in a statistically significant increase in FIB administration in NOF fracture patients.
86 - Assessing the Rate of Bone Protection with IV Zoledronic Acid for Frail Patients Admitted with Neck of Femur Fractures
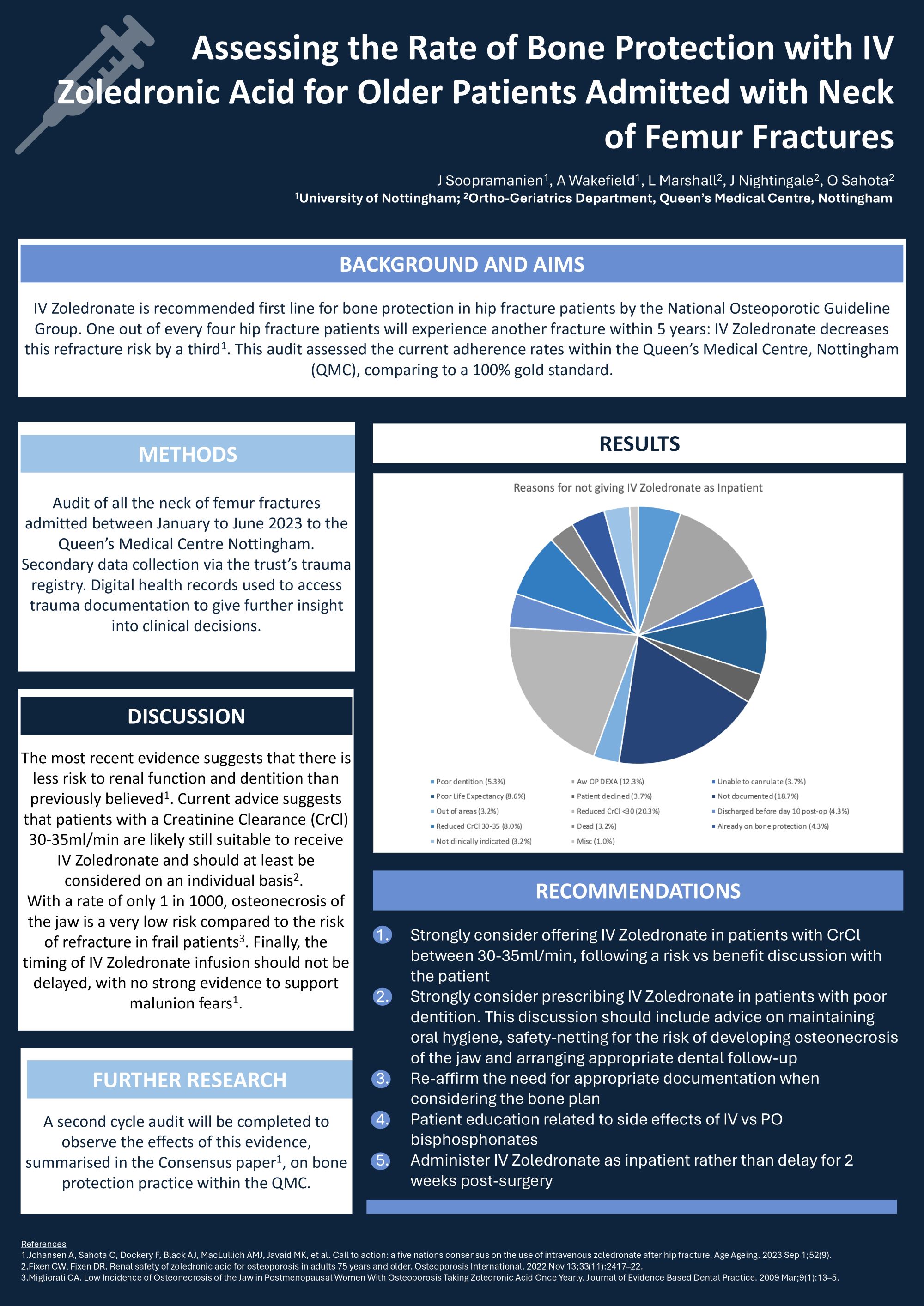
Jasen Soopramanien1, Anisha Wakefield1, Opinder Sahota2, Lindsey Marshall2, Jessica Nightingale2
1University of Nottingham, Nottingham, United Kingdom. 2Queens Medical Centre, Nottingham, United Kingdom
Abstract
Introduction: IV Zoledronate is recommended first line for bone protection in neck of femur fracture (NOF) patients by the National Osteoporotic Guideline Group. One in four NOF patients will experience re-fracture within 5 years: IV Zoledronate decreases this risk by a third. This audit assessed the current adherence rates within the Queen’s Medical Centre, Nottingham (QMC), comparing to a 100% gold standard.
Methods: A retrospective audit of secondary data was conducted, analysing all NOFs admitted to the QMC between January - June 2023. Data was collected via the Trust’s trauma registry. Information about clinical decisions was ascertained via digital health records to view the clinical documentation.
Results: An adherence rate of 50.1% was found from the total of 307 patients included – far below the gold standard, although the QMC has notably been well above national averages for such rates. The main reasons for eligible patients not receiving IV Zoledronate includes: Borderline Creatinine Clearance (CrCl) 30-35ml/min (8%), Patient discharged before day 10 of inpatient stay (4.3%), Poor dentition (5.3%), No documentation about clinical decision-making (18.7%)
Discussion/Implications: The most recent evidence suggests that there is less risk to renal function and dentition than previously believed. Current advice suggests that patients with a CrCl 30-35ml/min are likely still suitable to receive IV Zoledronate and should at least be considered on an individual basis. With a rate of only 1 in 1000, osteonecrosis of the jaw is a very low risk compared to the risk of refracture in frail patients. Finally, the timing of IV Zoledronate infusion should not be delayed, with no strong evidence to support malunion fears. A 2nd cycle audit will be completed to observe the effects of this evidence, summarised by Johansen et all in their Consensus paper, on bone protection practice within the QMC.
261 - Validation of British Hip Society Guidelines for Prioritisation in Hip surgery
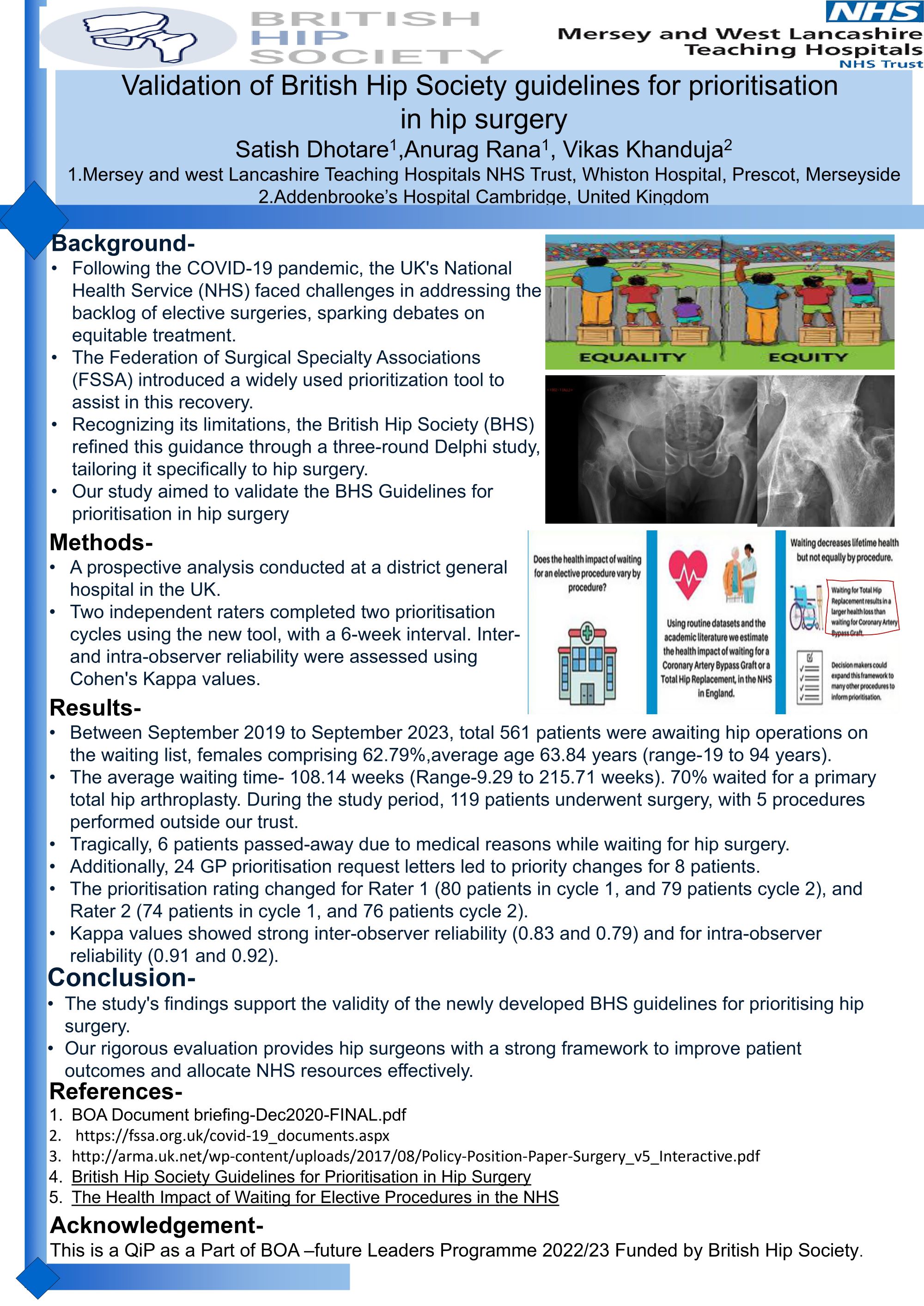
Satish Dhotare1, Anurag Rana1, Vikas Khanduja2
1Merseyside and West Lancashire Teaching Hospitals NHS Trust, Whiston Hospital, Prescot, Merseyside, Prescot, Merseyside, United Kingdom. 2Addenbrooke's Hospital, Cambridge, United Kingdom
Abstract
Background: Following the COVID-19 pandemic, the UK's National Health Service (NHS) faced challenges in addressing the backlog of elective surgeries, sparking debates on equitable treatment. The Federation of Surgical Specialty Associations (FSSA) introduced a widely used prioritization tool to assist in this recovery. Recognizing its limitations, the British Hip Society (BHS) refined this guidance through a three-round Delphi study, tailoring it specifically to hip surgery. Our study aimed to validate the BHS Guidelines for prioritisation in hip surgery.
Methods: A prospective analysis conducted at a district general hospital in the UK. Two independent raters completed two prioritisation cycles using the new tool, with a 6-week interval. Inter- and intra-observer reliability were assessed using Cohen's Kappa values.
Results: Between September 2019 to September 2023, total 561 patients were awaiting hip operations on the waiting list, females comprising 62.79%. The average age was 63.84 years (range-19 to 94 years). The average waiting time was 108.14 weeks (Minimum-9.29 to 215.71 weeks). Of these patients, 70% waited for a primary total hip arthroplasty. During the study period, 119 patients underwent surgery, with 5 procedures performed outside our trust. Tragically, 6 patients passed-away due to medical reasons while waiting for hip surgery. Additionally, 24 GP prioritisation request letters led to priority changes for 8 patients. The prioritisation rating changed for Rater 1 (80 patients in cycle 1, and 79 patients cycle 2), and Rater 2 (74 patients in cycle 1, and 76 patients cycle 2). Kappa values showed strong inter-observer reliability (0.83 and 0.79) and for intra-observer reliability (0.91 and 0.92).
Conclusion: The study's findings support the validity of the newly developed BHS guidelines for prioritising hip surgery. Our rigorous evaluation provides hip surgeons with a strong framework to improve patient outcomes and allocate NHS resources effectively.
321 - Surgical Site Infections: Are we getting better?

Daniel Lewandowski1, Claire Joyner1, Francesca Solari1, Aso Mohammed2
1Morriston Hospital, Swansea, United Kingdom. 2Morriston Hospitsal, Swansea, United Kingdom
Abstract
A surgical site infection (SSI) occurs when micro-organisms get into the part of the body that has been operated on and multiply in the tissues. The incidence of SSIs in neck of femur procedures is roughly 1% in England. Surgical site infections can lead to significant morbidity and mortality and can be divided to superficial and deep, where deep infections carry a 4.5-fold increase in mortality in hip fracture patients .
A prospective analysis of SSI rates in fracture neck of femur patients was recorded at Morriston Hospital from 1/3/2023 to 28/08/2023 and compared to previous year studies. Data analysis included gender, age, ASA, time to theatre, grade of surgeon, COVID status, and material for closure (monocryl vs clips).
Results were compared to previous years 2019-2022 (monocryl vs clips). SSIs in 2019 showed a rate of 6.9%, with monocryl compliance of 52%. 2023 demonstrated a SSI rate of 3.95% with 98.4% monocryl compliance. Skin preparation with alcoholic betadine and 2% chlorhexidine gluconate (CHG) was compared. There was a higher SSI rate in alcoholic betadine use (12% vs 3.4%). Patients deemed to have deep infections (1.6%) returned to theatre vs superficial infections (2.3%) treated with antibiotics. There was no difference in surgeon grade between trainees and consultants for SSI rates. Infections were found to be higher in total hip hemiarthroplasties, compared to other operations.
Analysing the data over the years, evidence shows that using monocryl vs clips has improved SSI rates in neck of femur fracture patients, as well as 2% CHG skin prep use.
508 - Surgical Tray Leaning: Carbon, efficiency and cost-savings in MAKO Robotic-assisted Total Knee Arthroplasty
Ghaith Al-Abbasi, Caitlin Brennan, Nick Ohly, Christopher Gee
Golden Jubilee University National Hospital, Clydebank, United Kingdom
Abstract
Background: Robotic-assisted total knee arthroplasty (RA-TKA) is associated with a higher carbon footprint compared to manual total knee arthroplasty. This quality improvement project sought to reduce the carbon and financial costs associated with MAKO RA-TKA by ‘leaning’ surgical trays.
Methods: The contents of each tray in use were collated. Surgeons routinely performing MAKO RA-TKA were consulted and reached a consensus on instruments that were either essential or could be removed and provided as an individually packaged supplemental. Three new ‘lean trays’ were introduced for the primary MAKO RA-TKA. Carbon and financial savings were calculated, recording the reduction in the number of trays requiring decontamination, sterilisation, and repackaging.
Results: Leaning has reduced tray count from five to four, removing 36 instruments per case. In 5 months, the use of ‘lean trays’ avoided 115 unnecessary trays being reprocessed and sterilised. There has been a total carbon saving of 220.85 kgCO2e due to avoided sterilisation processes (176 kgCO2e) and use of tray wraps (44.85 kgCO2). Staff satisfaction has been high citing the ability to count instruments more quickly, increased space in the theatre, and reduced learning curve for unfamiliar staff. Additionally, an approximate financial saving of £5,750 was made due to the reduced burden on sterilisation services.
Conclusions: Innovative technologies must be implemented with sustainability in mind. The implementation of 'lean trays' for orthopaedic and other surgical procedures should be considered by all departments to minimise the impact of surgical practice on the environment while also improving efficiency and lowering costs.
653 - Improving sustainability in paediatric orthopaedic day case surgery: A pilot study.
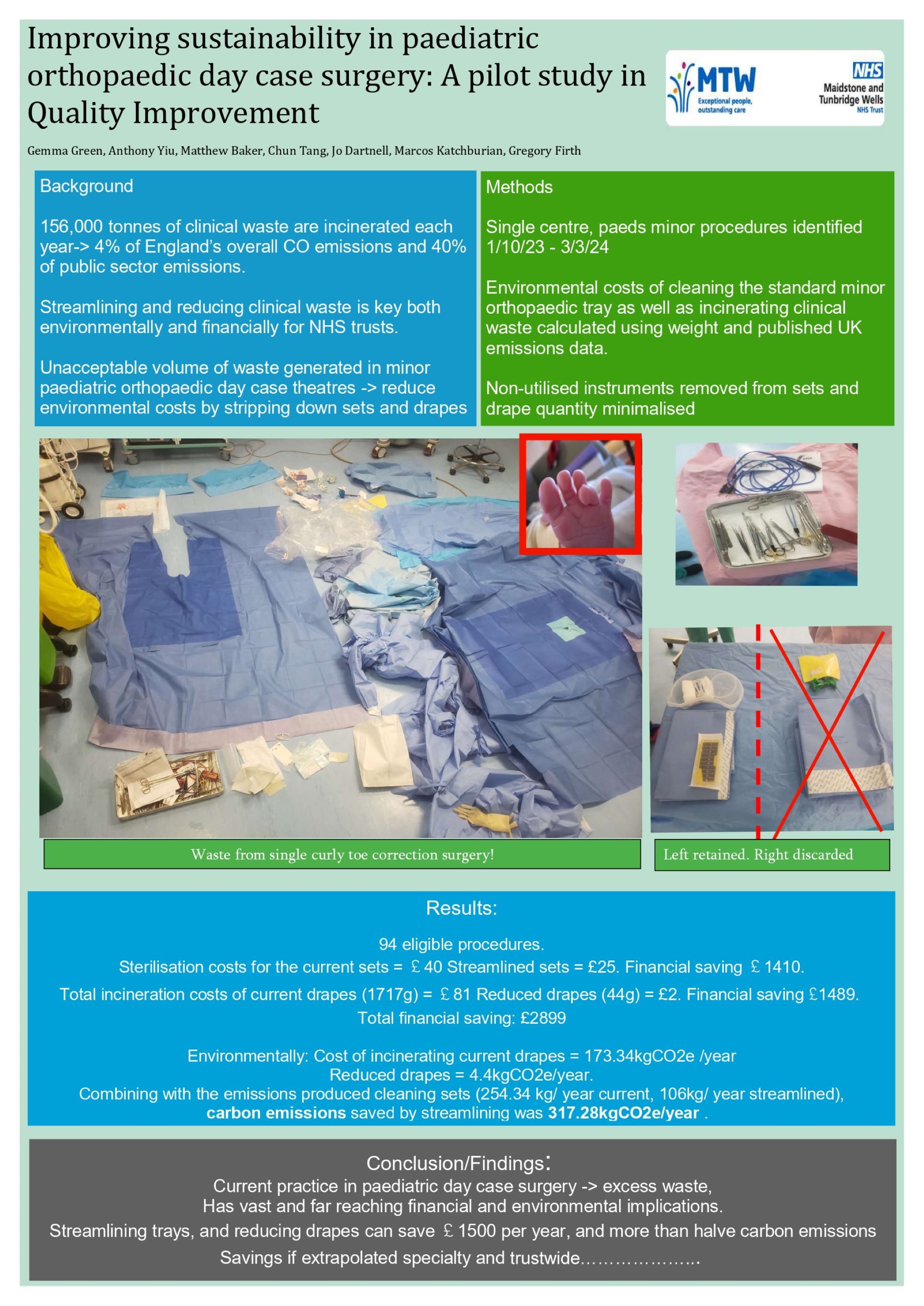
Gemma Green, Anthony Yiu, Matthew Baker, Chun Tang, Jo Dartnell, Marcos Katchburian, Gregory FirthMaidstone and Tunbridge Wells NHS Trust, Tunbridge Wells, United Kingdom
Abstract
Background: In the NHS 156,000 tonnes of clinical waste are incinerated each year, producing 4% of England’s overall carbon emissions and 40% of public sector emissions. Streamlining and reducing clinical waste is key both environmentally and financially for NHS trusts. Volume of waste generated in paediatric orthopaedic day case theatres is unacceptable. We aim to reduce economic and environmental costs by using streamlined sets and drapes.
Methods: Paediatric orthopaedic day cases in one centre were identified between 1 April 2023 and 31 March 2024. Environmental costs of cleaning the standard minor orthopaedic tray as well as incinerating clinical waste generated per case was calculated using weight and published UK emissions data. Sets were scrutinised, and surplus instruments removed. Reduced draping was identified with the trust sustainability team. The cost of sterilisation was calculated using data from IHSS and NHS published costs.
Results: 94 eligible procedures were included. Sterilisation costs for the current sets were £40 compared to £25 for streamlined sets. Financial saving £1410. Total incineration costs of current drapes (1717g) were £81 compared to £2 for reduced drapes (44g). Financial saving £1489. Environmentally, the cost of incinerating current drapes was 173.34kgCO2e /year, compared to 4.4kgCO2e/year for reduced drapes. Combining this with the emissions produced in cleaning sets (254.34 kg/ year current, 106kg/ year streamlined), the carbon emissions saved by streamlining was 317.28kgCO2e/year .
Conclusion/Findings: Current practice in paediatric day case surgery is generating excess waste, with both financial and environmental implications. Streamlining trays, and reducing drapes can save £1500 per year, and more than halve carbon emissions produced. Extrapolating to other areas of orthopaedics, would further enhance this saving.
Implications: Small changes in practice can collectively make a substantial difference to our environment.
687 - “Putting The Patient Front And Centre”: Rebuilding the Orthopaedic PROMS Service In Arthroplasty – A Quality Improvement Project
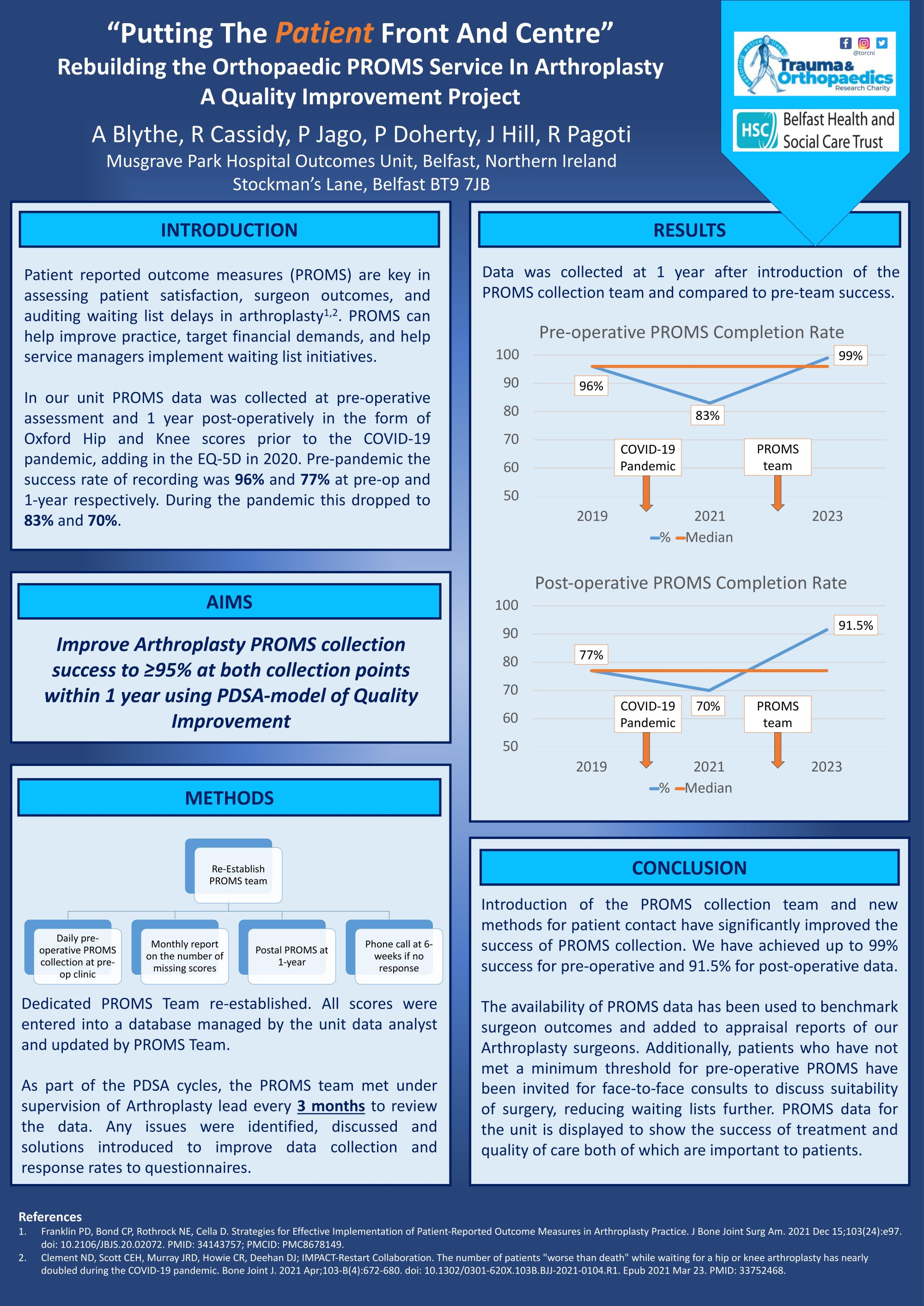
Andrew Blythe1, Roslyn Cassidy2, Paul Jago1, Patricia Doherty2, Janet Hill2, Ravikanth Pagoti1
1Belfast Health and Social Care Trust, Belfast, United Kingdom. 2Trauma and Orthopaedic Research Charity, Belfast, United Kingdom
Abstract
Background: Patient-reported outcome measure scores (PROMS) are key in determining outcomes after hip and knee arthroplasty and can assist evaluating arthroplasty surgeons and units. In our unit, pre-operative and 1-year PROMS are collected using the Oxford Hip and Knee score and the EuroQOL 5 dimension (EQ-5D) score. With the advent of the pandemic, this practice faltered considerably; at recommencement of elective work in 2022, the number of missing pre-operative PROMS had increased to 17%, and 1-year PROMS to 30%. Our aim was to reduce this to <5% in both categories.
Methods: Using the Plan-Do-Study-Act model, the following changes were made to improve PROMS recording: A dedicated PROMS collation team, Daily pre-operative PROMS collection using clinic lists to cross-reference missing data, A monthly report on the number of missing scores, Postal PROMS questionnaires at 1-year along with a cover letter and addressed envelope, Missing scores at 6-weeks followed up with a phone call. The PROMS team met every three months to review data. Any issues were identified, discussed and solutions introduced.
Results: One year on from establishing the PROMS team and database, the rate of missing pre-operative scores reduced to 1%, with missing 1-year scores reduced to 8.5%. PROMS data has been included as part of the 2023 appraisal reports for all arthroplasty surgeons. Individual surgeon and unit health gains were reported along with NHS England health gains. This has allowed surgeons to compare their outcomes to those of their peers as well as NHS England.
Conclusion: Improvement to PROMS collection methods and assembly of a dedicated PROMS team has greatly improved accuracy of PROMS recording in our unit. This has aided in disseminating accurate outcomes, benchmarking individual surgeon outcomes, superior data for audit and research and delivering patient-focused best-practice changes for hip and knee arthroplasty.
704 - Pausing before you implant- A NICE idea.
Nikhil Ravindranath Gangane, Benjamin Kapur
Glan Clwyd Hospital, Betsi Cadwaladr University Health board, Rhyl, United Kingdom
Abstract
Background: The selection of a wrong implant in a primary elective joint replacement is rare. This refers to an event where the prosthesis used for the patient by the surgeon is the incorrect size, is put on the wrong side or if the parts of the implants used are incompatible with each other. This is also termed as a ‘never event’ and occurred at our health care system 2 years ago where a 32mm head was implanted with a 36 liner. This was caught by the National Joint Registry (NJR) which lead to the implementation of NICE guidelines NG157. This includes a prosthesis check-list when the boxes are opened and the same boxes checked prior to closure to prevent this never event from occurring again. This form is signed by the surgeon, circulator and scrub nurse and kept in the patient’s notes.
Aim: To identify the accuracy of the prosthesis pause check-list in preventing a never event.
Methods: A prospective study of 50 patients undergoing primary hip and knee arthroplasty by a single surgeon where each patient had a prosthetic pause check-list.
Results: Despite the prosthesis pause check-list by NICE guidelines for all arthroplasty patients, the circulatory nurse produced an out-of-date/expired head in a case of a primary hip arthroplasty. The wrong implant was identified and discarded.
Conclusions/ Findings: This ‘never event’ would have been missed if not for the NICE guidelines, which clearly state that all the components should be checked by the surgeon and the scrub team at the time they are opened and implanted and a final review and check for the compatibility should be made prior to closure.
Shoulder and Elbow - Poster Abstracts
147 - Custom 3D Printed Glenoid Guides Allow for Precise Guidewire Placement in Deformed Glenoid Faces: A Cadaveric Study
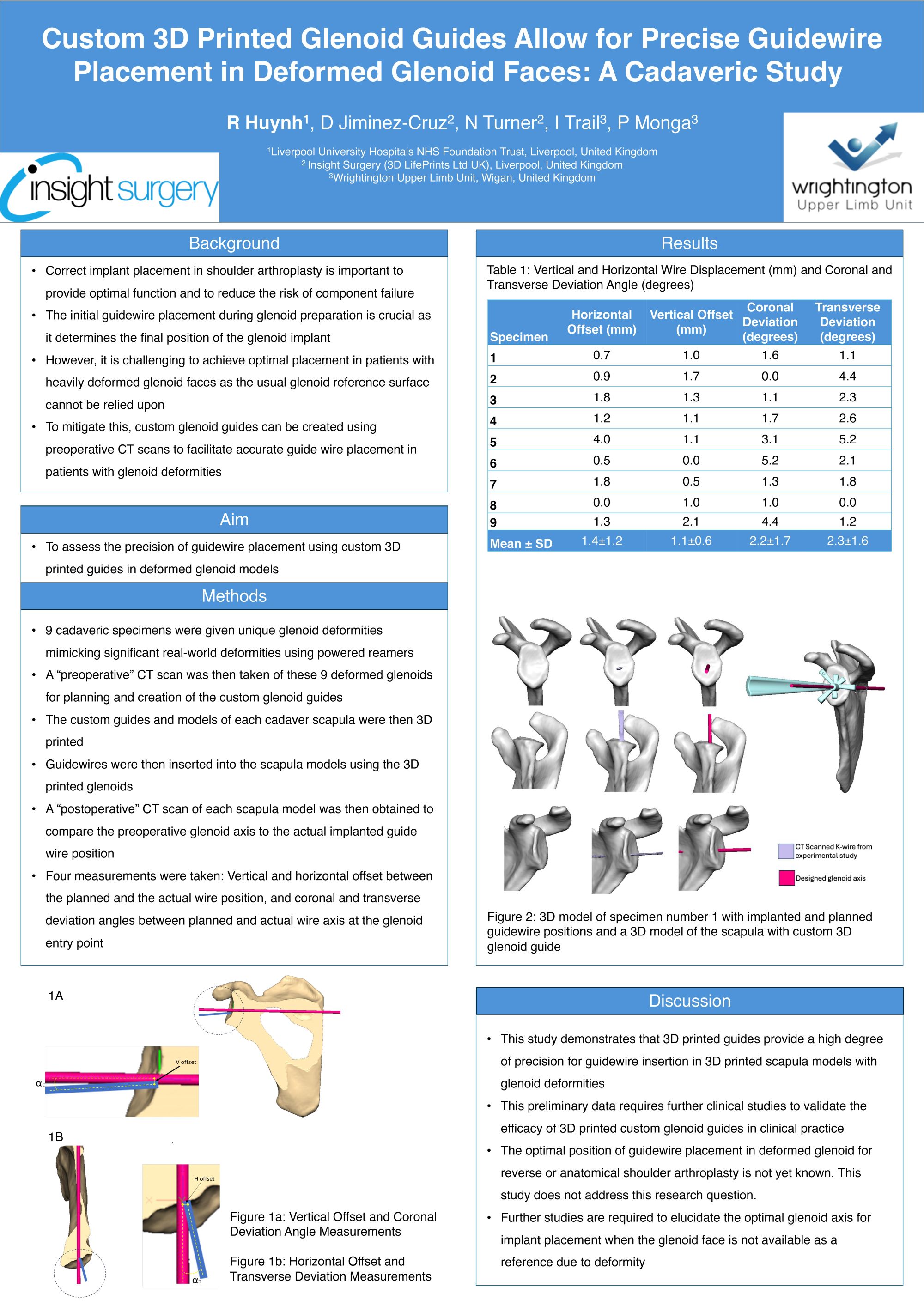
Richard Huynh1,2, David Jiminez-Cruz3, Henry Pinchbeck3, Ian Trail4, Puneet Monga4
1Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom. 2University of Liverpool, Liverpool, United Kingdom. 33D LifePrints Ltd UK, Liverpool, United Kingdom. 4Wrightington, Wigan, and Leigh NHS Foundation Trust, Wigan, United Kingdom
Abstract
Introduction: Correct implant placement in shoulder arthroplasty is important to provide optimal function and to reduce the risk of component failure. The initial guidewire placement during glenoid preparation is crucial as it determines the final position of the glenoid implant. However, it is challenging to achieve optimal placement in patients with heavily deformed glenoid faces as the usual glenoid reference surface cannot be relied upon. To circumvent this, 3D printed custom guides can be utilised to allow for wire placement as per preoperative planning on CT scans. However, this technology relies on a normal glenoid face to determine the optimal glenoid axis and currently no method exists for defining this in deformed glenoid faces. Additionally, the current guides may not have enough stability during usage due to their design and thus affect the precision of wire placement.
Aim: To assess the precision of guidewire placement using custom 3D printed glenoid guides in deformed cadaveric glenoid specimens.
Methods: 9 cadaveric specimens were prepared with unique glenoid face deformities. Custom 3D glenoid guides were then created based on “preoperative” CT scans. The specimens then underwent guidewire insertion using the guides. “Postoperative” CT scans were obtained from which four measurements were taken. The measurements were deviation angle between optimal and wire axes in the coronal and transverse planes and horizontal and vertical deviation from the optimal axis in millimetres.
Results: Deviation angles in the transverse and coronal planes were 2.3±1.6° and 2.2±1.7° respectively. Horizontal deviation was 1.4±1.2mm. Vertical deviation was 1.1±0.6mm.
Conclusion: Our cadaveric data demonstrates high precision in these custom 3D printed glenoid guides for initial guidewire placement. Clinical studies are required to determine the efficacy of this type of guide in shoulder arthroplasty. Further studies are also required to define the optimal glenoid axis in deformed glenoid faces.
162 - A prospective cross-sectional survey comparing management of proximal humerus fractures across a multi-national upper limb specialist panel
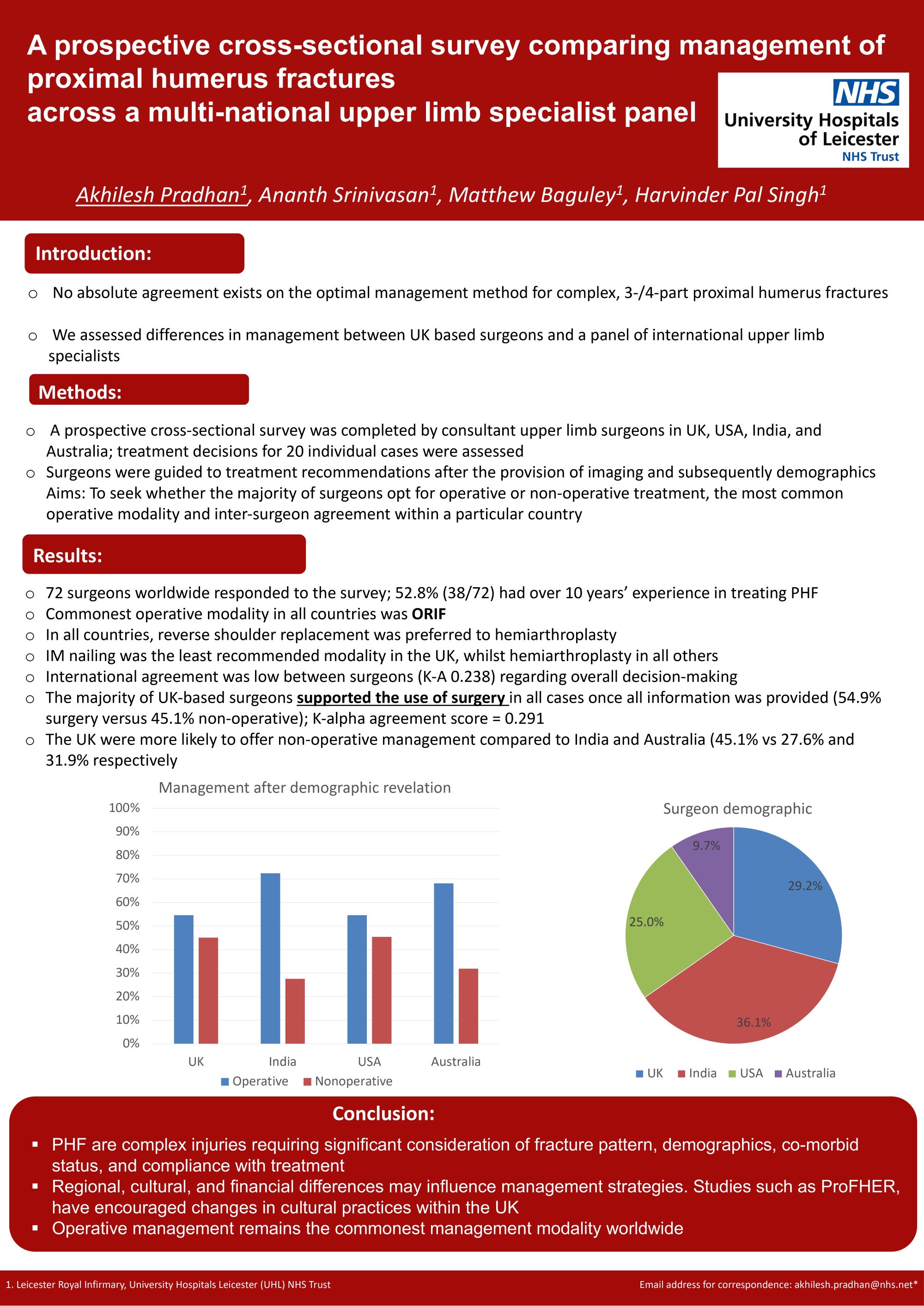
Akhilesh Pradhan, Ananth Srinivasan, Matthew Baguley, Harvinder Singh
University Hospitals Leicester NHS Trust, Leicester, United Kingdom
Abstract
Background: Proximal humerus fractures are the most common traumatic bony injury to the shoulder. No absolute agreement exists on the optimal method of management for various morphologies/fracture patterns. Our study assesses differences in management of these fractures between UK and international upper limb specialists.
Methods: A prospective cross-sectional survey was completed by shoulder surgeons in UK, USA, India, and Australia. Treatment decisions for 20 individual cases were assessed with standardisation of clinical data and imaging. Inclusion criteria included patients 20-80 years, 3/4-part Neer proximal humerus fractures, fracture-dislocations. Statistical analysis was performed using Krippendorff’s alpha.
Results: 72 surgeons worldwide responded to the study. 29.2% (21/72) were UK-based and 36.1% (26/72) were Indian. 95.2% (20/21) of UK surgeons were NHS-based whilst 84.6%, 100% and 71.4% of Indian, US and Australian surgeons worked in the private sector. After discussion of demographics and imaging, 54.9% of UK-based surgeons opted for operative management, whilst 72.4% of Indian, 54.6% of American and 68.1% of Australian surgeons opted for operative management. Commonest operative modality in all countries was ORIF. In all countries, reverse shoulder replacement was preferred to hemiarthroplasty. IM nailing was the least recommended modality in the UK, whilst hemiarthroplasty was the least recommended in all others. Agreement between surgeons was highest in the UK (K-alpha 0.291) whilst India had the lowest surgeon agreement (K-alpha 0.235). Overall, international agreement was low between surgeons (0.238).
Conclusion: Most UK-based surgeons work in the public sector and there is high inter-surgeon agreement in decision-making between UK surgeons. Surgery remains the main management modality with ORIF being the most popular choice, however, UK and USA-based surgeons were less likely to offer operative intervention. Further higher-powered studies are required to assess the infrastructure and cost implications of these findings.
163 - Optimizing Oxford Shoulder Scores with Computerized Adaptive Testing Reduces Redundancy While Maintaining Precision: An NHS England National Joint Registry Analysis
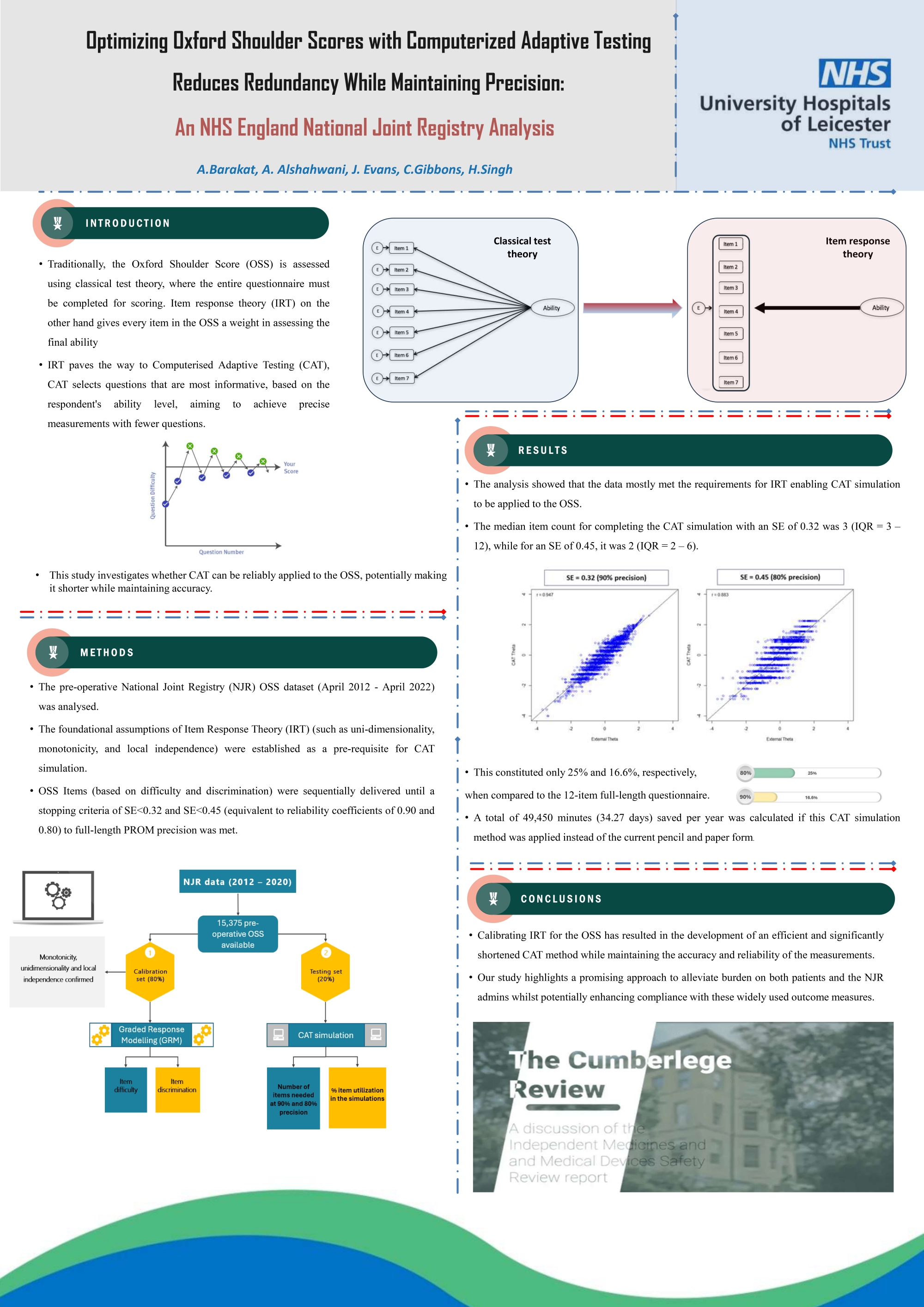
Ahmed Barakat1, Jonathan Evans2, Christopher Gibbons3, Harvinder Singh1
1University Hospitals Leicester, Leicester, United Kingdom. 2University of Exeter, Exeter, United Kingdom. 3The University of Texas MD Anderson Cancer Center, Texas, USA
Abstract
Background: The Oxford Shoulder Score (OSS) is a 12-item Patient Reported Outcome Measure commonly used for the assessment of shoulder surgeries. It was developed using a classical test theory for the scoring system. This study explores whether Computerised Adaptive Testing (CAT) implementation provides a shortened, individually tailored questionnaire whilst maintaining test accuracy.
Methods: Analysing the pre-operative National Joint Registry OSS dataset (April 2012 - April 2022), foundational Item Response Theory (IRT) assumptions for CAT were assessed. Uni-dimensionality, monotonicity, and local independence were established using Confirmatory Factor Analysis (CFA), Mokken scaling (H ≥ 0.3), and Yen’s Q3 statistic (cutoff > 0.2). A Graded Response Model (GRM) guided CAT simulation, considering item difficulty and discrimination. CAT compared sequential item selection with stopping criteria set at SE<0.32 and SE<0.45 (equivalent to reliability coefficients of 0.90 and 0.80) to full-length PROM precision. The frequency of item usage in the simulation was quantified by item utilization percentage.
Results: CFA exhibited satisfactory fit, presenting RSMSR of 0.06, CFI of 0.85, and TLI of 0.82. Monotonicity, measured by H value, yielded 0.482, signifying good monotonic trends. Local independence was generally met, with Yen’s Q3 statistic > 0.2 for most items. The median item count for completing the CAT simulation with an SE of 0.32 was 3 (IQR = 3 – 12), while for an SE of 0.45, it was 2 (IQR = 2 – 6). This constituted only 25% and 16.6%, respectively, when compared to the 12-item full-length questionnaire.
Conclusions: Calibrating IRT for the OSS has resulted in the development of an efficient and significantly shortened CAT method while maintaining the accuracy and reliability of the measurements. Through the reduction of redundant items and implementation of a standardised measurement scale, our study highlights a promising approach to alleviate the burden and potentially enhance compliance with these widely used outcome measures.
276 - The posterolateral ligament of the elbow: anatomy and clinical relevance
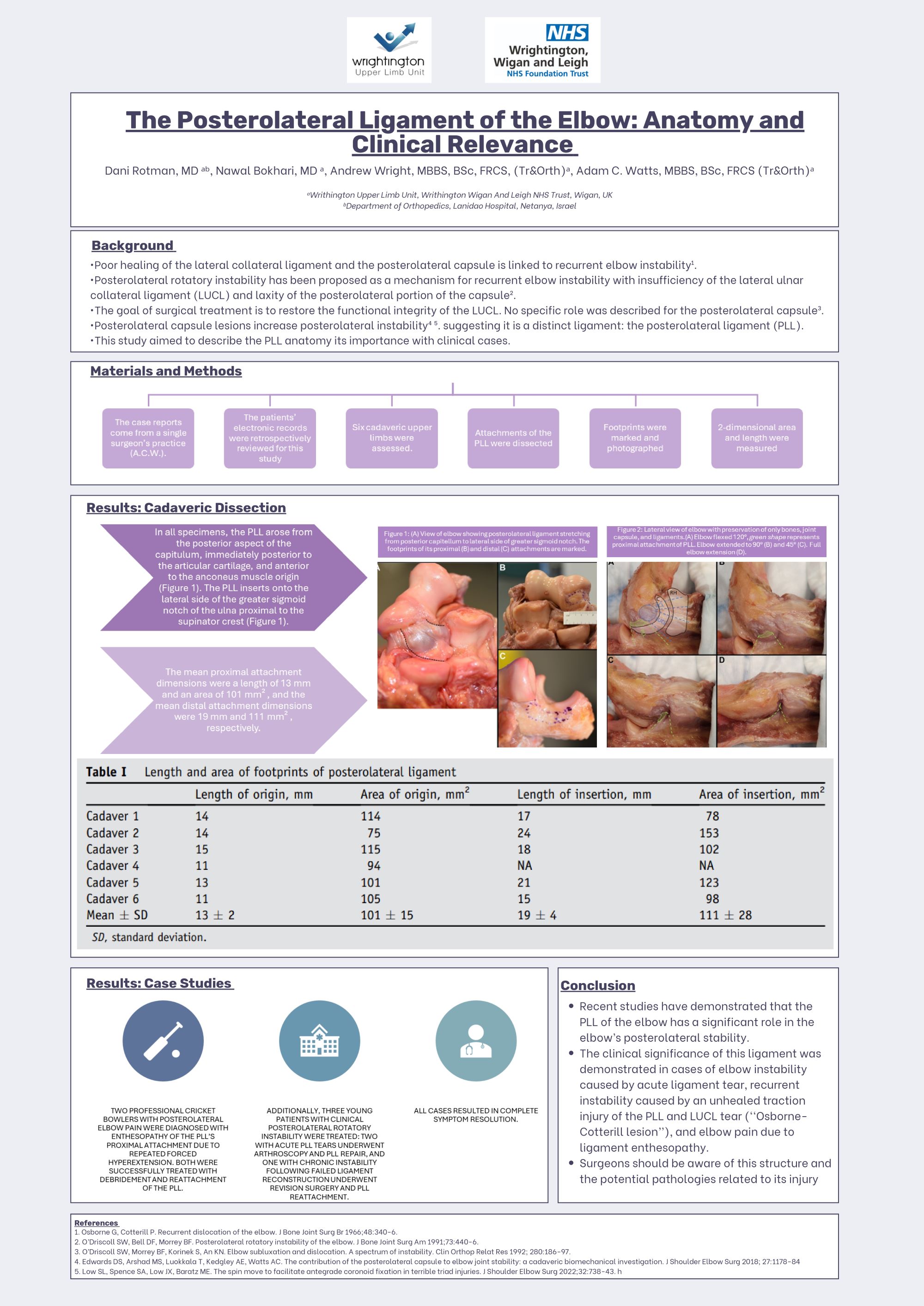
Dani Rotman1, Nawal Bokhari2, Andrew Wright2, Adam Watts2
1Department of Orthopedics, Laniado Hospital, Netanya, Israel. 2Wrightington Upper Limb Unit, Wrightington Wigan and Leigh NHS Trust, Wigan, United Kingdom
Abstract
The posterolateral capsule was recognized as an important structure for elbow stability but was later disregarded. Two recent biomechanical studies demonstrated its role in preventing posterolateral instability thus it should be identified as a distinct ligament. This study includes 2 parts: an anatomic study of PLL’s footprint and a collection of 5 cases of pathologic lesions of PLL.
Six cadaveric upper limbs were assessed. The attachments of PLL were dissected, footprints marked and photographed, and 2-dimensional area and length measured.
The mean proximal attachment dimensions were a length of 13mm and area of 101mm2. The mean distal attachment dimensions were 19mm and 111mm2. There were 2 cases of posterolateral elbow pain in professional cricket bowlers, diagnosed radiographically as enthesopathy of PLL’s proximal attachment on the posterior capitellum, probably due to repeated forced hyperextension of the elbow. Both patients were treated by debridement of posterior capitellum and reattachment of PLL, with complete resolution of symptoms. There were 3 cases of clinical posterolateral rotatory instability in young patients. Two athletes had an isolated acute tear of PLL and both had positive posterior draw test results but negative pivot-shift test results. Both underwent elbow arthroscopy and repair of PLL with resolution of symptoms. The third patient had long-standing recurrent elbow instability, following a failed lateral ulnar collateral ligament reconstruction, in the presence of an Osborne-Cotterill lesion. He underwent revision lateral ulnar collateral ligament reconstruction, bone grafting of the bony lesion, and reattachment of PLL, with complete resolution of symptomatic posterolateral rotatory instability.
The PLL has a significant role in the elbow’s posterolateral stability. Its footprints were described, and clinical significance was demonstrated in cases of elbow instability caused by acute ligament tears and elbow pain due to ligament enthesopathy. Surgeons should be aware of this structure and potential pathology related to its injury.
350 - Suture button bone block fixation for anterior shoulder stabilisation: a cadaveric study of the relationship to the suprascapular nerve.
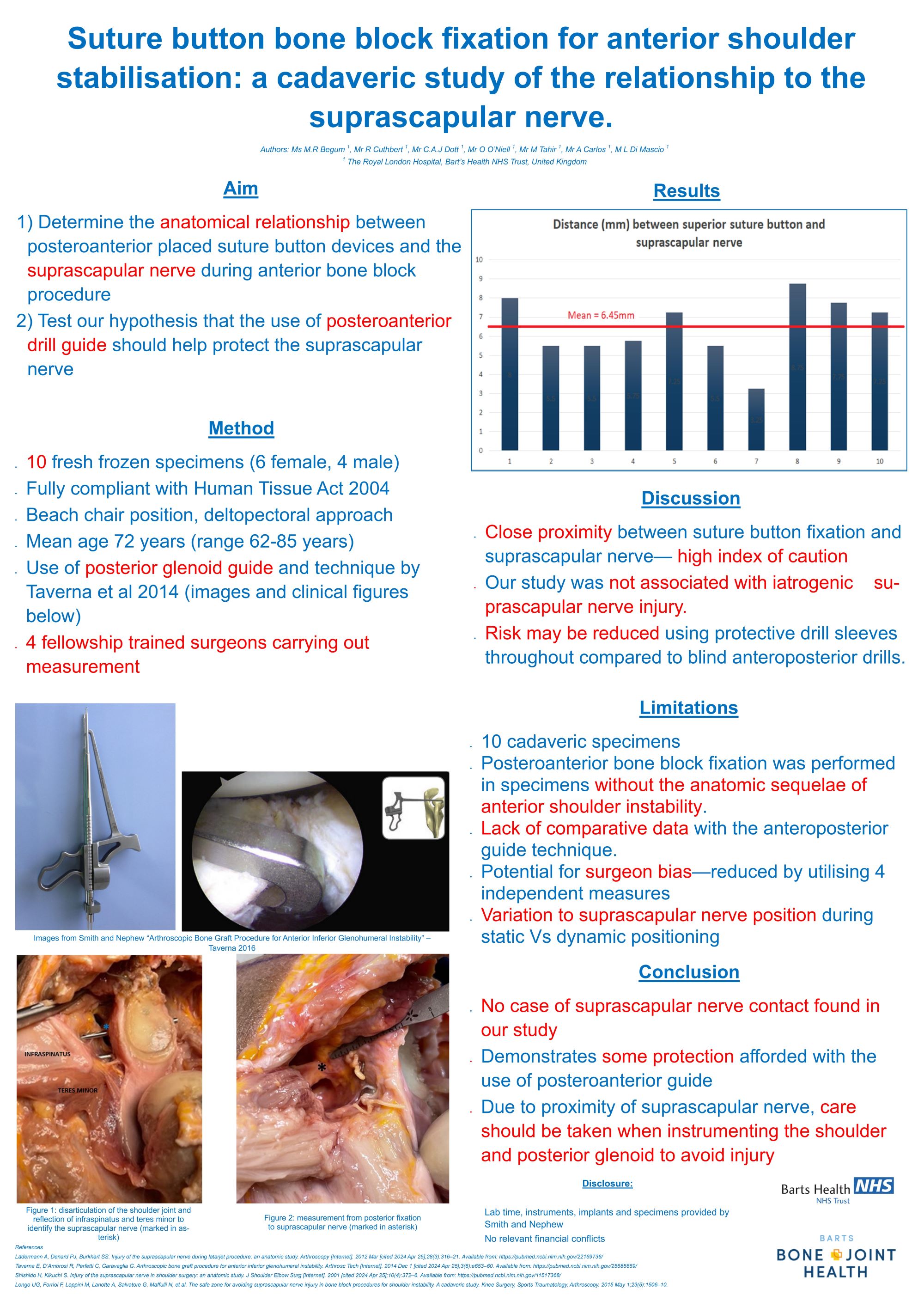
Musammad Rashida Begum, Rory Cuthbert, Cameron Dott, Owen O'Neill, Mo Tahir, Adrian Carlos, Livio Di Mascio
The Royal London Hospital, London, United Kingdom
Abstract
Background: Suprascapular nerve injury is a recognised complication of bone block procedures and coracoid transfers using screw fixation to address anterior shoulder instability secondary to the nerve’s proximity to the posterior glenoid and potential vulnerability to posterior screw penetration. The relationship of the suprascapular nerve has not been clearly established when utilising guides designed to perform such procedures using suture button fixation. Posterior-anterior fixation guides may reduce risk of iatrogenic suprascapular nerve injury by reducing the risk of medial/superior placement of fixation devices on the posterior glenoid. We present the first cadaveric study to assess the safety of posterior-anterior bone block fixation for anterior shoulder stabilisation using such guides to quantify this relationship.
Method: Anterior glenoid bone block reconstruction using suture buttons was performed in ten fresh frozen cadavers in accordance with established technique utilising the posterior-anterior drilling guide. Disarticulation of shoulder joint with elevation of infraspinatus and teres minor facilitated measurement of the relationship and shortest distance from the posterior drill holes and instrumentation in the glenoid to the suprascapular nerve.
Results: The suprascapular nerve was not compromised utilising the posterior-anterior glenoid guide and suture button fixation technique in all specimens. The mean distance from superior sleeve and tunnel to the nerve was 5mm in females and 6.8mm in males. The lowest distance from superior sleeve to suprascapular nerve was 3.25mm and the highest was 8.75mm.
Conclusion: The use of posterior-anterior referenced drill guides when performing suture button fixation of bone blocks for treatment of anterior instability appears safe with no cases of iatrogenic suprascapular nerve injury in the specimens examined. However, the proximity of the nerve underscores the need for caution throughout and although posterior-anterior referenced guides appear to assist in avoiding iatrogenic injury of the suprascapular nerve, anterior referenced guides alone may not afford similar protection.
446 - Suture slippage: the Weak Link of the Knotless Cuff Repair
Kushalappa Subbiah1, Matthew Donaldson1, Cameron Stephen2, Allan Young1, Benjamin Cass1
1Sydney Shoulder Research Institute, Sydney, Australia. 2Aberdeen Royal Infirmary, Aberdeen, United Kingdom
Abstract
Rotator cuff repairs show varying rates of healing. Type 1 failures are commonly seen in knotless double row repairs and existing literature has identified the lateral row anchor as the weakest link in the repair construct. Suture slippage has been shown to occur in the lateral row anchor, during the critical period following a repair. This slippage, occurring in the initial period, may potentially lead to gap formation and eventual repair failure.
Lab based study with analysis of 3 different suture materials (FiberTape, FiberWire and SutureTape) loaded into a single type of lateral row anchor (5.5 Swivelock) and tested in 2 different densities (osteoporotic and normal) of saw bone models. Testing utilised perpendicular traction of loaded sutures in a load cell with assessment of Maximum force (N) and Displacement (mm). The blocks were visually analysed and Cut through length(mm) was measured.
Suture type (P<0.001) and Bone density(P<0.001) have a significant effect on maximum force tolerance by the construct. FiberTape can withstand a much higher maximum force irrespective of bone densityies. Displacement data collected from the load cell, shows that suture type (P<0.001), irrespective of but not bone density (P=0.228) plays a significant role, with FiberTape having a comparatively lower displacement. Evaluation of cut through data shows that bone density (P=0.006), but not suture type (P=0.94), has a significant effect on cut-through.
Our study has shown a positive correlation between suture slippage and type of suture used along with density of bone. We conclude, and therefore recommend, that FiberTape should be used in a knotless construct as it has a higher Maximum force and shows less displacement when compared to other suture types. With lateral row anchors in osteoporotic bone, we believe that a change in angle of insertion can improve the interference fixation, but this needs future validation.
649 - Is there still a role for metallic anchors in shoulder stabilisation surgery? Minimum 10-year follow-up of 30 patients
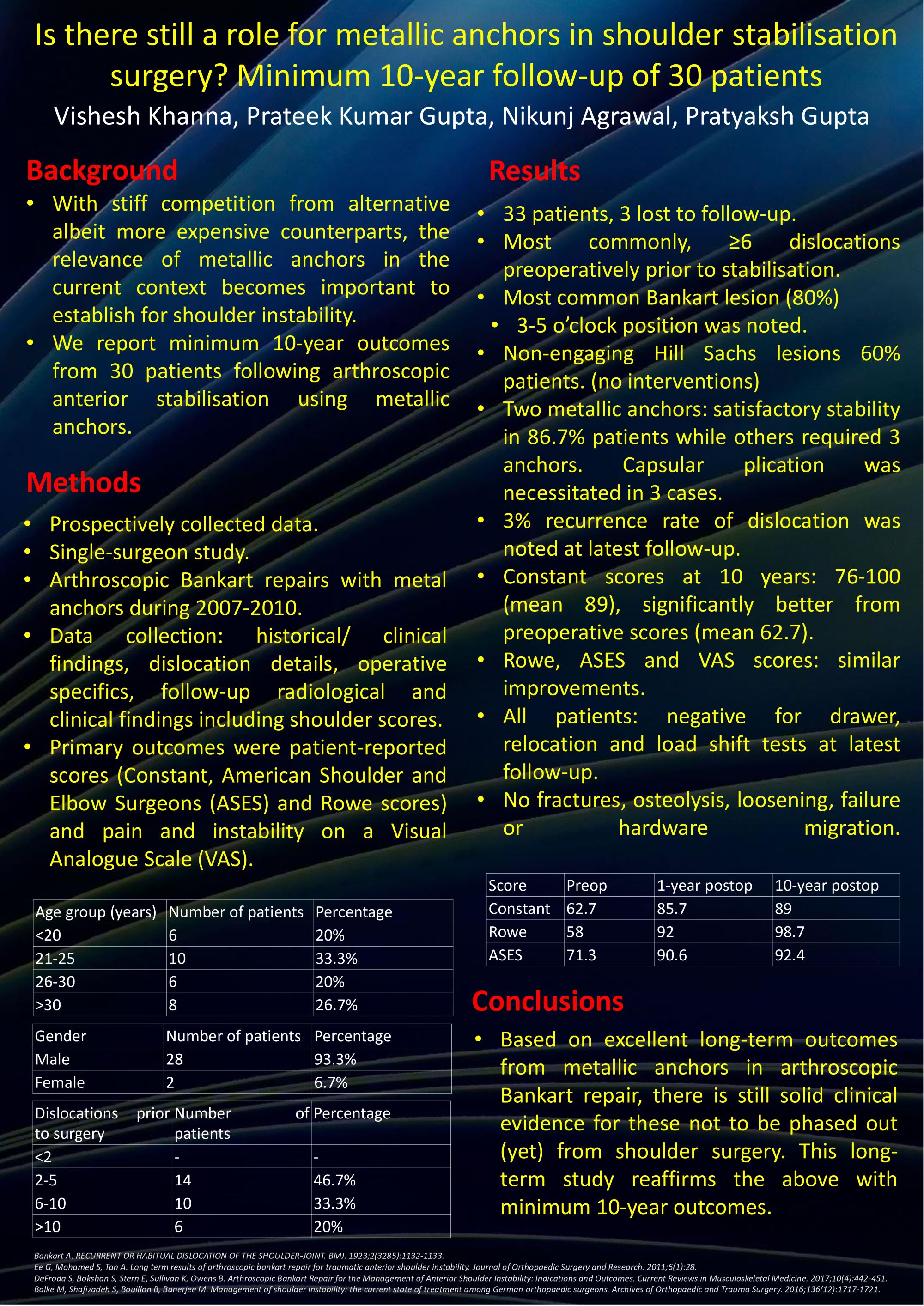
VISHESH KHANNA1, Prateek Gupta2, Nikunj Agrawal2, Pratyaksh Gupta2
1Wirral University Teaching Hospital, Chester, United Kingdom. 2Sir Ganga Ram Hospital, NEW DELHI, India
Abstract
Background: With stiff competition from alternative albeit more expensive counterparts, the relevance of metallic anchors in the current context becomes important to establish for shoulder instability. We report minimum 10-year outcomes from 30 patients following arthroscopic anterior stabilisation using metallic anchors.
Methods: Prospectively collected data from arthroscopic Bankart repairs performed using metal anchors during 2007-2010 was retrospectively analysed in this single-surgeon study. Comprehensive data collection included historical and clinical findings, dislocation details, operative specifics, follow-up radiological and clinical findings including shoulder scores. The primary outcomes were patient-reported scores (Constant, American Shoulder and Elbow Surgeons (ASES) and Rowe scores) and pain and instability on a Visual Analogue Scale (VAS).
Results: Among 33 patients matching the inclusion criteria, 3 were lost to follow-up. Less than half had between 2-5 dislocations prior to stabilisation while the majority had ≥6 episodes. In 80% patients, a Bankart lesion between 3-5 o’clock position was noted. Associated non-engaging Hill Sachs lesions were seen in 60% patients. These were deemed too small for any intervention. Two metallic anchors gave satisfactory stability in 86.7% patients while others required 3 anchors. Capsular plication was necessitated in 3 cases. A 3% recurrence rate of dislocation was noted at latest follow-up. Constant scores at 10 years postoperatively measured between 76-100 (mean 89), significantly better from preoperative scores (mean 62.7). Congruous improvements were also noted on Rowe, ASES and VAS scores. All patients were negative for drawer, relocation and load shift tests at latest follow-up. No occurrences of fractures, osteolysis, loosening, failure or hardware migration were seen.
Conclusions: Based on excellent long-term outcomes from metallic anchors in arthroscopic Bankart repair, there is still solid clinical evidence for these not to be phased out (yet) from shoulder surgery. This long-term study reaffirms the above with minimum 10-year outcomes.
677 - Superior Capsular Reconstruction in massive rotator cuff tears: a single surgeon outcome study based on NICE interventional procedures programme
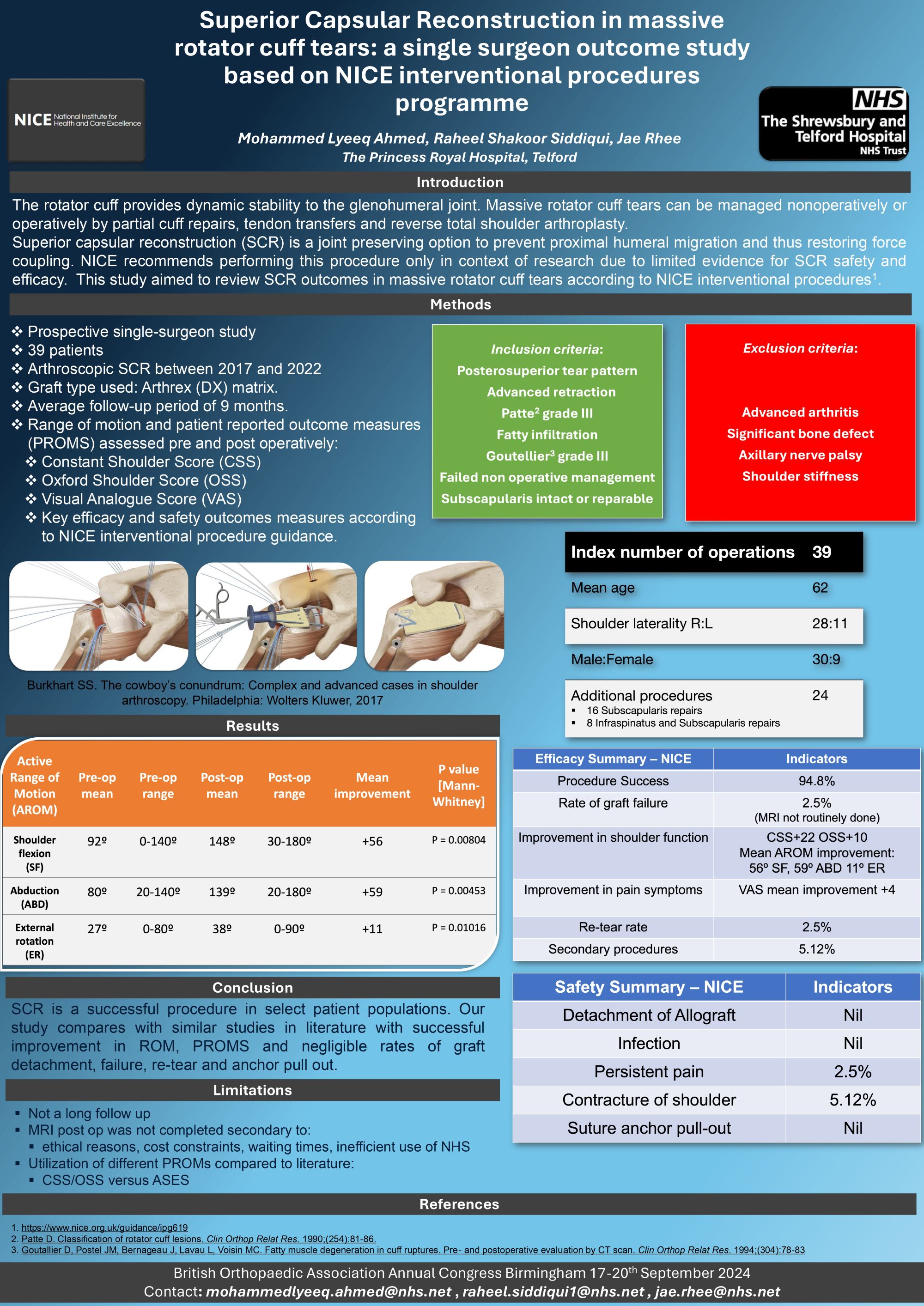
Mohammed Lyeeq Ahmed, Raheel Shakoor Siddiqui, Jae Rhee
The Shrewsbury & Telford Hospital NHS Trust, Telford, United Kingdom
Abstract
Background: The rotator cuff provides dynamic stability to the glenohumeral joint. Massive rotator cuff tears can be managed nonoperatively or operatively by partial cuff repairs, tendon transfers and reverse total shoulder arthroplasty. Superior capsular reconstruction (SCR) is a joint preserving option to prevent proximal humeral migration and thus restoring force coupling. NICE recommends performing this procedure only in context of research due to limited evidence for SCR safety and efficacy.
Methods: Prospective single-surgeon study. Thirty-nine patients who underwent arthroscopic SCR between 2017 and 2022 were included. The inclusion criteria were posterosuperior tear pattern, advanced retraction, fatty infiltration, failed nonoperative management and subscapularis intact or reparable. Graft type used was Arthrex xenograft (DX) matrix. Average follow-up period was 9 months. Range of motion and patient reported outcome measures (PROMS) including Constant Shoulder Score (CSS), Oxford Shoulder Score (OSS) and Visual Analogue Score (VAS) were assessed pre and post operatively. Key efficacy and safety outcomes measures selected according to NICE interventional procedure guidance.
Results: Mean ROM improvement post op were: 56° flexion (p=0.008), 59° abduction (p=0.004) and 11° external rotation (p=0.01). The CSS and OSS improved +22 (p=0.003) and +10 (p=0.001) respectively. VAS showed an improvement of +4 (p=0.02). Procedure success rate was 94.8%. The rate of graft failure and persistent post-op pain was 2.5%. Two patients had secondary procedures. No patients had graft detachment, infection, suture anchor pull-out.
Conclusion: SCR is a successful procedure in select patient populations. Our study compares with similar studies in literature with successful improvement in ROM, PROMS and negligible rates of graft detachment, failure, re-tear and anchor pull out.
Implications: Further randomized controlled trials and case-controlled studies should be conducted to on a larger population size to analyse long term outcomes of SCR in patients with massive rotator cuff tears.
825 - Assessing the effectiveness of suprascapular nerve block in the treatment of frozen shoulder: a systematic review and meta-analysis of randomised controlled trials

Jonathon Bennett1, Neal Patel2, Nakulan Nantha-Kumar3, Veronica Phillips1, Sandeep Nayar3, Niel Kang3
1University of Cambridge, Cambridge, United Kingdom. 2University College London, London, United Kingdom. 3Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom
Abstract
Background: Frozen shoulder is a common and debilitating condition characterised by pain and restricted movement at the glenohumeral joint. Various treatment modalities have been explored to alleviate symptoms, with suprascapular nerve block (SSNB) emerging as a promising intervention. This meta-analysis aimed to assess the effectiveness of SSNB in treating frozen shoulder.
Methods: The study protocol was registered with PROSPERO (CRD42023475851). We searched the Medline, Embase and Cochrane Library databases in November 2023. Randomised controlled trials (RCTs) comparing SSNB against alternative interventions were included. The primary outcome was any functional patient-reported outcome measure (PROM). Secondary outcomes were the Visual Analog Scale (VAS) for pain, range of motion (ROM), and complications. Risk of bias was assessed using the Cochrane risk-of-bias v2.0 tool.
Results: 12 RCTs were identified (702 patients, mean age 55 years). 8 RCTs were deemed “low” risk-of-bias and 4 raised “some concerns”. Comparator interventions included intra-articular steroid injection, hydrodistension, physiotherapy and placebo injection with 0.9% saline. 7 studies compared SSNB to intra-articular steroid injection, with SSNB resulting in greater improvement in the Shoulder and Pain Disability Index (SPADI) (mean difference -4.75; 95% CI -8.11 to -1.39; P=0.006) and external rotation (mean difference 11.64; 95% CI -0.05 to 23.33; P= 0.05). In 3 studies SSNB demonstrated better VAS (mean difference -0.31; 95% CI -0.53 to 1.79; P=0.004) compared to physiotherapy (+/- placebo injection). 1 study favoured hydrodistension over SSNB in improving ROM and VAS. There was no significant difference in outcomes between SSNB administered under ultrasound-guidance or using a landmark technique.
Conclusion and Implications: SSNB can be administered in the outpatient clinic with promising outcomes compared to intra-articular steroid injection or physiotherapy based on level 1 evidence. It can therefore be considered as a first-line treatment option.
881 - Complications with use of Locking Plate Fixation for Proximal Humeral Fractures: A Long-term Review
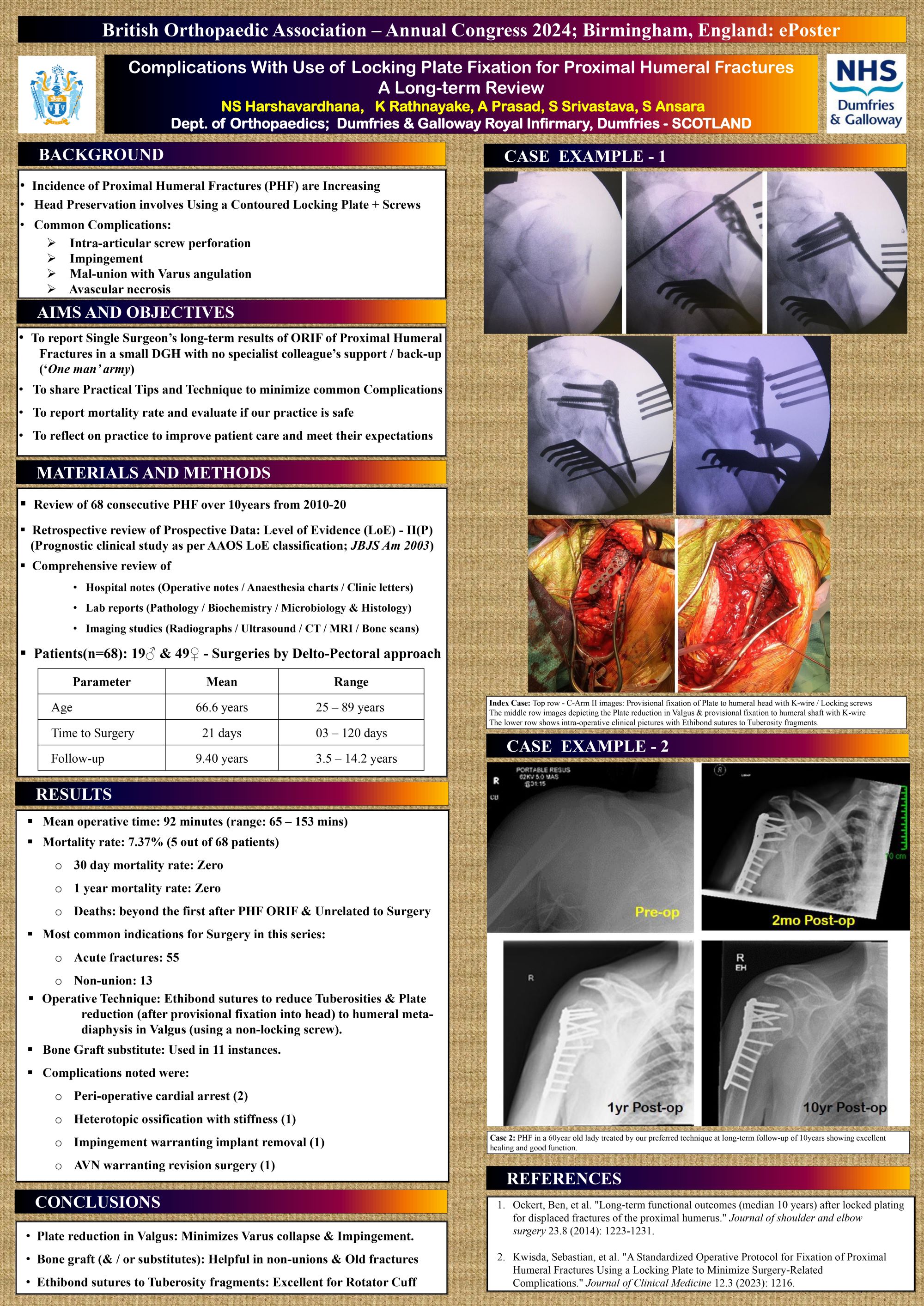
Nanjundappa S HARSHAVARDHANA, Kalana RATHNAYAKE, Ankit Prasad, Subodh Srivastava, Sameh Ansara
Dumfries and Galloway Royal Infirmary, Dumfries, United Kingdom
Abstract
Introduction: Proximal humeral fractures’ incidence is increasing and head preserving surgery involves fixation using a contoured locking plate that are associated with high complication rate (viz. intra-articular screw perforation, impingement, Mal-union with Varus collapse, Avascular necrosis[AVN] and need for Revision surgery).
Aim: The purpose of this study was to undertake a long-term review and share surgical technique and tips to minimize the above complications at a mean follow-up of 9.4years in a single surgeon’s cohort of 68 patients.
Methods: Sixty-eight patients (19M and 49F) with proximal humeral fractures that were operated by a locking plate fixation formed the study cohort against stringent inclusion vs. exclusion criteria. The mean age at surgery was 66.6years (range: 25–89y) and the mean follow-up was 9.4years (range: 3.5–14.2y). Serial radiographs were taken at first visit, pre-op, post-op and final follow-up. Adverse events causing unplanned return to theatres, instrumentation failure along with infections and AVN were recorded and managed appropriately. The operative technique included use of a Delto-pectoral approach and Ethibond sutures to reduce the tuberosities and performing a plate reduction (after initial fixation of chosen plate to the head fragment) to humeral meta-diaphysis in Valgus using a non-locking screw.
Results: 55patients were operated for acute fractures and 13patients presented had non-union with unacceptable function or on-going pain. All other 68fractures healed with improvement in Constant / DASH score and one patient warranted implant removal for plate-related complication.
Conclusion: Fracture reduction in slight Valgus and performing a plate reduction reduces the risk of Varus collapse and impingement. Bone graft (or its substitute) minimizes the risk of implant failure. These practical surgical tip minimizes the risk of need for re-operation at long-term.
Spines - Poster Abstracts
313 - Adopting Versatility: Imaging Alternatives for Spondylodiscitis Diagnosis In MRI-Contraindicated Cases
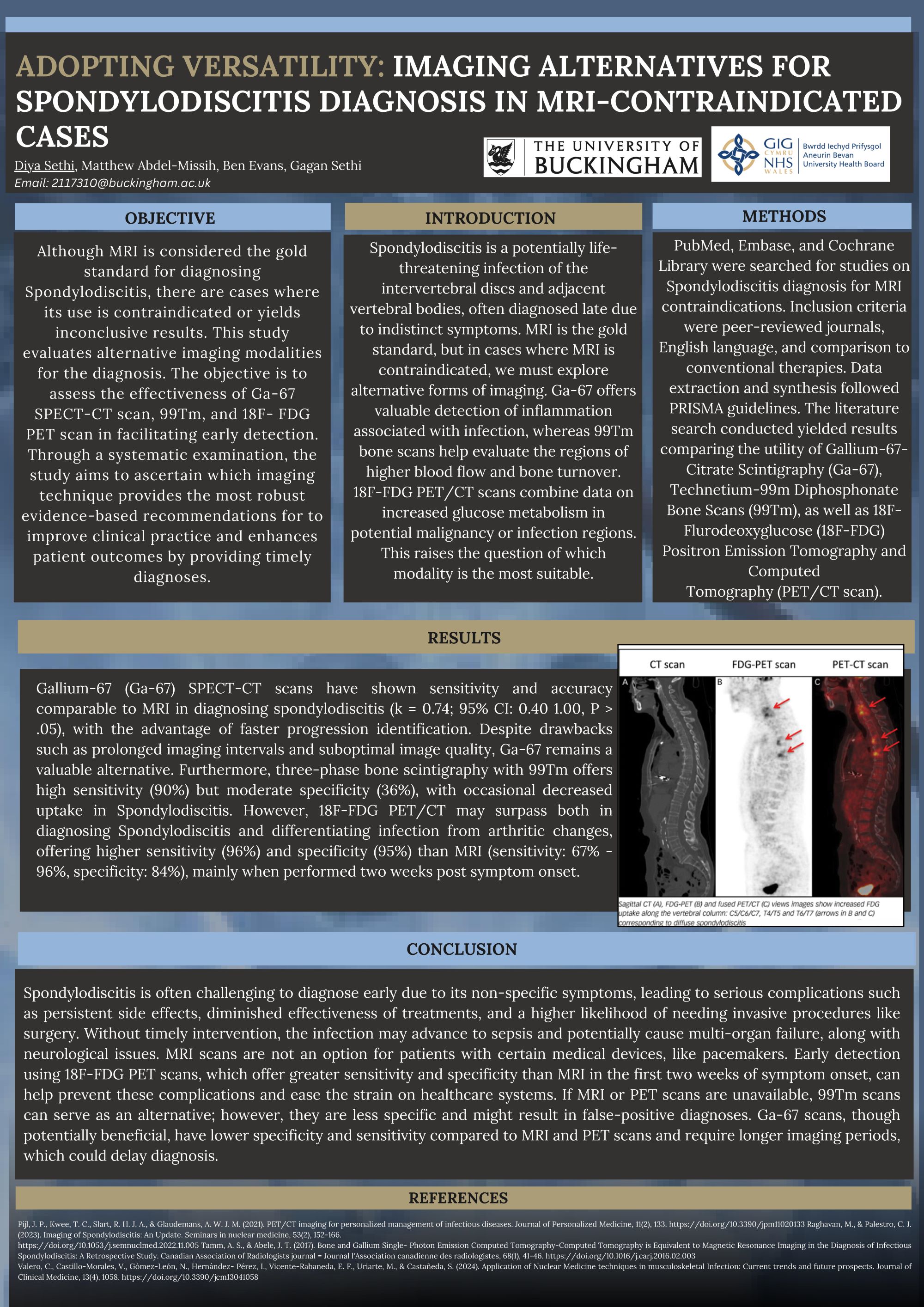
Diya Sethi1, Ben Evans1, Matthew Abdel-Missih1, Gagan Sethi2
1University of Buckingham, Crewe, United Kingdom. 2Aneurin Bevan University Health Board, Newport, United Kingdom
Abstract
Background: Spondylodiscitis is a potentially life-threatening infection of the intervertebral discs and adjacent vertebral bodies, often diagnosed late due to indistinct symptoms. MRI is the gold standard, but in cases where MRIs are contraindicated, we must explore alternative forms of imaging. This review aims to compare the efficacy of different available imaging modalities for such cases.
Methods: The literature search conducted on PUBMED, until February 2024 , yielded results for reviews comparing the utility of Gallium-67-Citrate Scintigraphy (Ga-67), Technetium-99m Diphosphonate Bone Scans (99Tm), as well as 18F-Flurodeoxyglucose (18F-FDG) Positron Emission Tomography and Computed Tomography (PET/CT scan). Only reviews in English were included and underwent rigorous evaluation, following PRISMA 2020 guidelines.
Results: Gallium-67 (Ga-67) SPECT-CT scans have shown sensitivity and accuracy comparable to MRI in diagnosing spondylodiscitis (k = 0.74; 95% CI: 0.40 - 1.00, P > .05), with the advantage of faster progression identification. Despite drawbacks such as prolonged imaging intervals and suboptimal image quality, Ga-67 remains a valuable alternative. Furthermore, three-phase bone scintigraphy with 99Tm offers high sensitivity (90%) but moderate specificity (36%), with occasional decreased uptake in Spondylodiscitis. However, 18F-FDG PET/CT may surpass both in diagnosing Spondylodiscitis and differentiating infection from arthritic changes, offering higher sensitivity (96%) and specificity (95%) than MRI (sensitivity: 67% - 96% specificity: 84%), mainly when performed two weeks post symptom onset.
Conclusion: There was no significant difference between the diagnostic capabilities of MRI and Ga-67. In contrast, 18F-FDG was better for early diagnosis, exhibiting a higher sensitivity and specificity in the first two weeks after symptoms presented than MRI. Moreover, 99Tm proved to be an inferior modality to the alternatives in diagnosing Spondylodiscitis. Research should aim to evaluate further using 18F-FDG as a first protocol candidate rather than MRI in early diagnosis.
471 - Artificial Intelligence and Machine Learning for Risk Prediction and Diagnosis of Vertebral Fractures: A Systematic Review and Meta-analysis
Srikar Namireddy1,2, Saran Gill1,2, Amaan Peerbhai1,2, Abith Kamath1,2, Daniele Ramsay1,2, Hariharan Subbiah Ponniah1,2, Dragan Jankovic3, Darius Kalasauskas3, Jonathan Neuhoff4, Andreas Kramer3, Florian Ringel3, Santhosh Thavarajasingam1,3
1Imperial Brain & Spine Initiative, London, United Kingdom. 2Imperial College School of Medicine, London, United Kingdom. 3Department of Neurosurgery, University Medical Center Mainz, Mainz, Germany. 4Center for Spinal Surgery and Neurotraumatology, Berufsgenossenschaftliche Unfallklinik, Frankfurt, Germany
Abstract
Background: The use of Artificial Intelligence (AI) and Machine Learning (ML) technologies for vertebral fractures has shown promising potential in enhancing diagnostic accuracy and efficiency. With increasing prevalence of vertebral fractures, the need for accurate diagnosis and prognostication becomes paramount.
Methods: This study assesses the effectiveness of AI algorithms in diagnosing and predicting risk of vertebral fractures. A comprehensive search was conducted across major databases, selecting studies that utilized AI for vertebral fracture diagnosis or prognosis, with a subsequent meta-analysis to quantitatively synthesize the findings. Diagnostic models were stratified based on the pathology for which they were tailored, namely non-pathological vertebral fractures, osteoporotic vertebral fractures, and vertebral compression fractures. The primary outcome measure was AUROC.
Results: Out of 14,161 studies initially identified, 79 were included in the final analysis, with 40 undergoing meta-analysis. AI based programmes can accurately diagnose and predict the risk of vertebral fractures (predictive AUROC= 0.82 [0.78-0.85]; osteoporotic vertebral fracture diagnosis AUROC= 0.92 [0.88-0.96]; non-pathological vertebral fracture diagnosis AUROC= 0.85 [0.81-0.88]; and vertebral compression fracture diagnosis AUROC= 0.87 [0.83-0.91]) at a significant level (p<0.001). Traditional models had the highest median AUROC (0.90) for fracture prediction. Deep learning models had the highest median AUROC for diagnosis of all 3 fracture types. Notably, high heterogeneity was observed among the studies (I² > 99%, p<0.001), suggesting a large variation in model design and performances.
Conclusion: AI technologies exhibit considerable promise in improving the diagnosis and prognostication of vertebral fractures, as evidenced by high accuracy levels in both domains. However, the observed heterogeneity and the high risk of bias in studies underscore the necessity for further research. Future efforts should focus on the standardization of AI models and validation across diverse datasets to ensure their clinical utility and effectiveness in diagnosing vertebral fractures.
Sports Trauma - Poster Abstracts
355 - Effects of an Untreated Medial Meniscal Ramp Lesion on the Biomechanical Properties...
...of the Tendon Graft during Anterior Cruciate Ligament Reconstruction and Histological findings of the Medial Meniscus: A Study in a Porcine Model
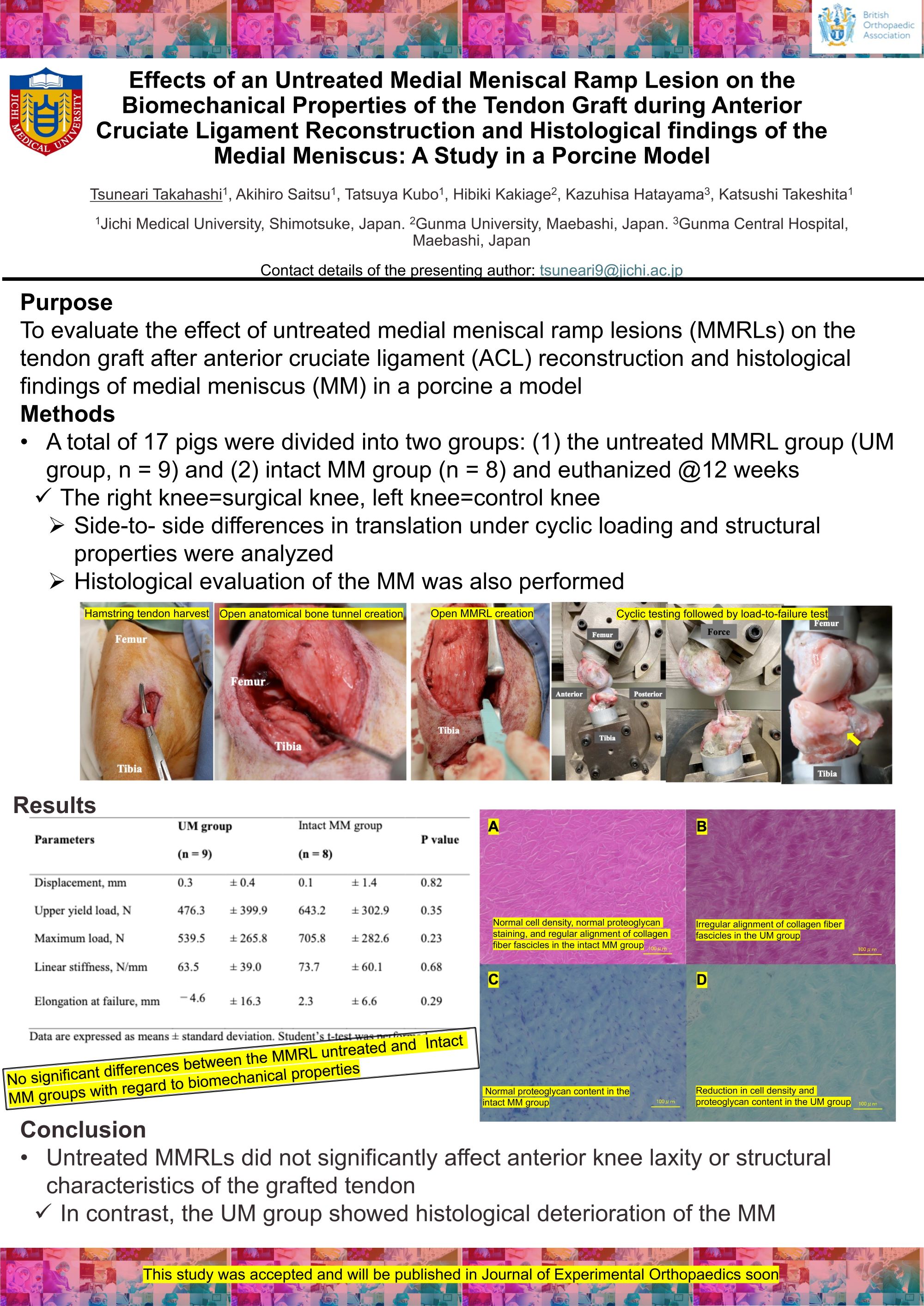
Tsuneari Takahashi1, Akihiro Saitsu1, Tatsuya Kubo1, Hibiki Kakiage2, Kazuhisa Hatayama3, Katsushi Takeshita1
1Jichi Medical University, Shimotsuke, Japan. 2Gunma University, Maebashi, Japan. 3Gunma Central Hospital, Maebashi, Japan
Abstract
Background: A few experimental studies have clarified the effects of meniscal ramp lesion (MMRL) repair after anterior cruciate ligament (ACL) reconstruction on tendon grafts whether untreated MMRLs affected the postoperative biomechanical properties and to present the histological findings of the MM in a porcine a model.
Methods: A total of 18 pigs were randomly divided into two groups: (1) the untreated MMRL group (UM group, n = 9) and (2) control group (n = 9). Among the included animals, 17 were euthanized 12 weeks after surgery. The obtained specimens were then tested cyclically (20 cycles, 0–40 N, 100 mm/min) in the direction of the native ACL and loaded to failure (50 mm/min) on a tensile tester. Side-to-side differences in translation under cyclic loading and structural properties were then analyzed. Histological evaluation of the MM was performed based on the Modified Mankin’s histological grading score and Modified Copenhaver classification score.
Results: No significant differences in upper yield load (UM group, 476.3 ± 399.9 N; control group, 643.2 ± 302.9 N), maximum load (UM group, 539.5 ± 265.8 N; control group, 705.8 ± 282.6 N), linear stiffness (UM group, 63.5 ± 39.0 N/mm; control group, 73.7 ± 60.1 N/mm), and elongation at failure (UM group, −4.6 ± 16.3 mm; control group, 2.3 ± 6.6 mm) were observed between the groups. However, the UM group had significantly worse Modified Mankin’s histological grading scores (1.8 ± 0.4 [1–2] vs. 0 ± 0 [0]; P < 0.001) and Modified Copenhaver classification scores (6.6 ± 2.4 [2–9] vs. 0.7 ± 1.1 [0–3]; P < 0.001) than did the control group.
Conclusion: Untreated MMRLs did not significantly affect anterior knee laxity or structural characteristics of the grafted tendon. In contrast, the UM group showed histological deterioration of the medial meniscal bodies 12 weeks after surgery.
Trauma - Poster Abstracts
25 - Cephalomedullary nailing for subtrochanteric proximal femoral fractures: Comparison of a single lag screw with a dual lag screw device
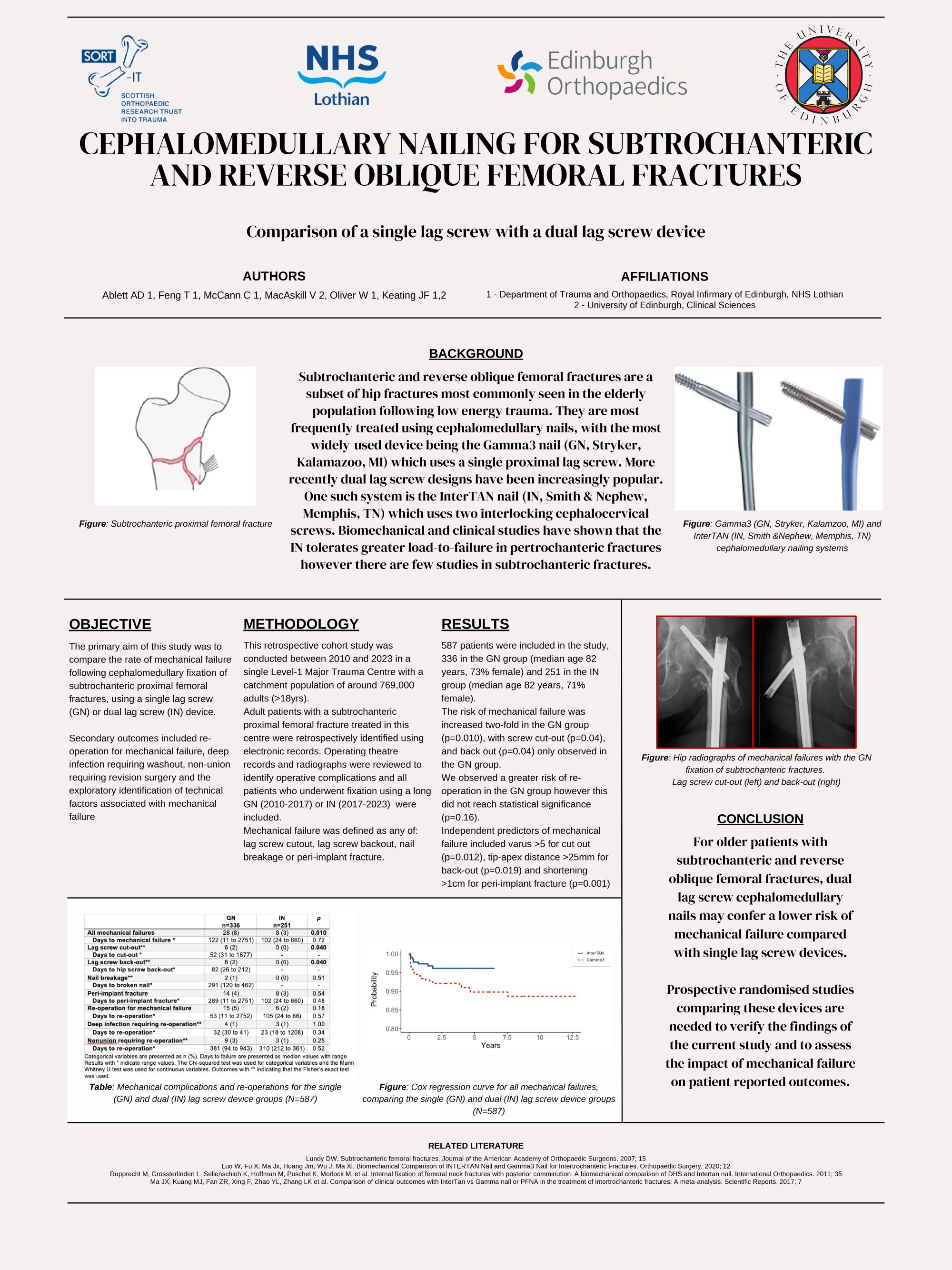
Andrew Ablett1, Conor McCann1, Tony Feng1, Victoria Maccaskill2, William Oliver1, John Keating1
1Royal Infirmary of Edinburgh, Edinburgh, United Kingdom. 2Edinburgh University, Edinburgh, United Kingdom
Abstract
Background: Subtrochanteric proximal femoral fractures are generally treated with cephalomedullary nail (CMN) fixation. We aimed to compare outcomes of subtrochanteric fracture fixation using a single lag screw (Gamma3 nail, GN) with a dual lag screw CMN (InterTAN nail, IN). The primary outcome measure was mechanical failure, defined as lag screw cut-out, back-out, nail breakage or peri-implant fracture. Secondary outcomes included re-operation for mechanical failure, deep infection, nonunion and technical predictors of mechanical failure.
Methods: Adult patients (≥18yrs) with a subtrochanteric proximal femoral fracture treated in a single centre were retrospectively identified using electronic records. All patients that underwent fixation using either a long GN (2010-2017) or IN (2017-2022) were included. Medical records and radiographs were reviewed to identify operative complications. Cox regression analysis was used to determine the effect of CMN design and technical parameters on mechanical failure and re-operation.
Results: 587 patients were included, 336 in the GN group (median age 82yrs, 73% female) and 251 in the IN group (median age 82yrs, 71% female). The risk of mechanical failure was increased two-fold in the GN group (adjusted hazard ratio (aHR) 2.55, p=0.018), with screw cut-out (p=0.04) and back-out (p=0.04) only observed in the GN group. However, there was no increased risk of re-operation for any indication (mechanical failure, p=0.16; deep infection, p=0.83; nonunion, p=0.38). Independent predictors of mechanical failure included varus >5° for cut-out (aHR 15.61, p=0.016), tip-apex distance >25mm for back-out (aHR 9.41, p=0.02) and shortening >1cm for peri-implant fracture (aHR 6.50, p=<0.001).
Conclusions: For older patients with subtrochanteric proximal femoral fractures, the dual lag screw design of the IN was associated with a lower risk of mechanical failure compared with the single lag screw of the GN. Dual lag screw designs may reduce the risk of mechanical complications for patients with subtrochanteric femoral fractures.
592 - Unveiling Financial Realities: The Substantial Economic Impact Of Centralised Complex Tibial Fracture Care In The UK
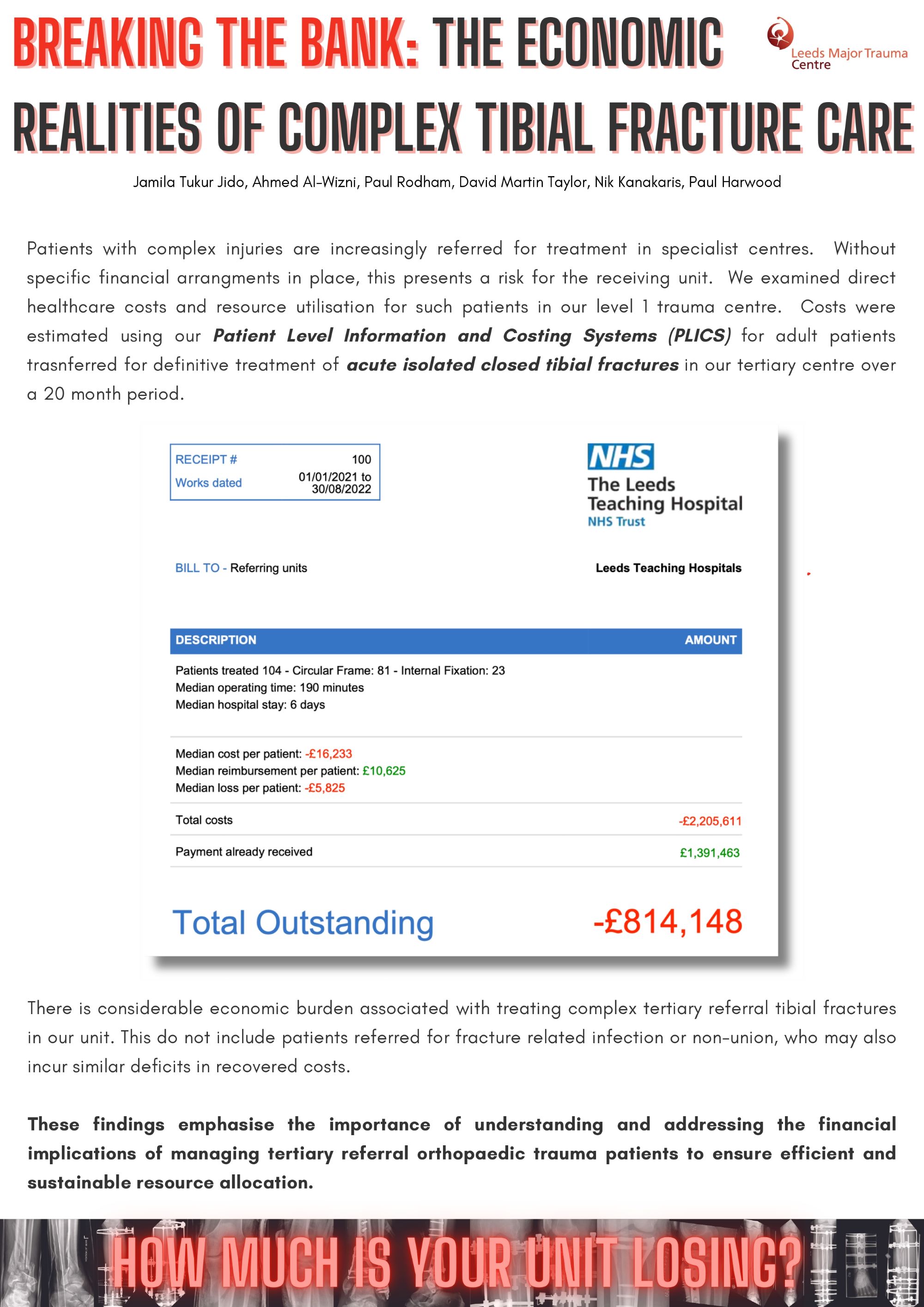
Jamila Tukur Jido1, Ahmed Al-Wizni1, Paul Rodham2, David Martin Taylor2, Nik Kanakaris2, Paul Harwood2
1University of Leeds, Leeds, United Kingdom. 2Leeds Teaching Hospitals, Leeds, United Kingdom
Abstract
Background: Management of complex fractures poses a significant challenge. Evolving research and changes to national guidelines suggest better outcomes are achieved by transfer to specialist centres. In the United Kingdom, the development of Major Trauma Networks was accompanied by relevant financial arrangements. These do not apply to patients with closed fractures referred for specialist treatment by similar pathways. Despite a surge in cases transferred for care, there is little information available regarding the financial impact on receiving institutions. Understanding the economic impact of centralising complex trauma care is critical to making these systems sustainable.
Objectives: To quantify the costs of, and reimbursement for, treating tertiary referral tibial fractures in a specialist centre in the United Kingdom
Study Design & Methods: This retrospective study examines data from a Level 1 trauma centre which includes a regional limb reconstruction unit. Patients were identified from our electronic referral system, used for all tertiary referrals. Transferred adult patients, undergoing definitive treatment of acute isolated closed tibial fractures in our tertiary centre, were included from a 2-year period.
Results: 104 patients were identified, there were 45 proximal (41), 18 diaphyseal (42) and 43 distal (43) fractures. 23 patients were treated by internal fixation and 81 with circular frames. Patients required a median of 190 minutes of total operative time and 6 days of hospital stay at a median cost of £16,233 each, median reimbursement was £10,625. The total cost of treatment for all 104 patients was £2,205,611 and total reimbursement was £1,391463, the median deficit per patient being £5825. The overall deficit over the 2 years was £814,148, there were significant positive outliers meaning that the average deficit per patient on this basis was £7,753.
Conclusions: This study reveals a considerable economic burden associated with treating complex tibial fractures.
597 - A Retrospective Review of Long-term Patient Reported Outcome Measures Comparing Unstable Ankle Fractures with and without a Posterior malleolus fracture
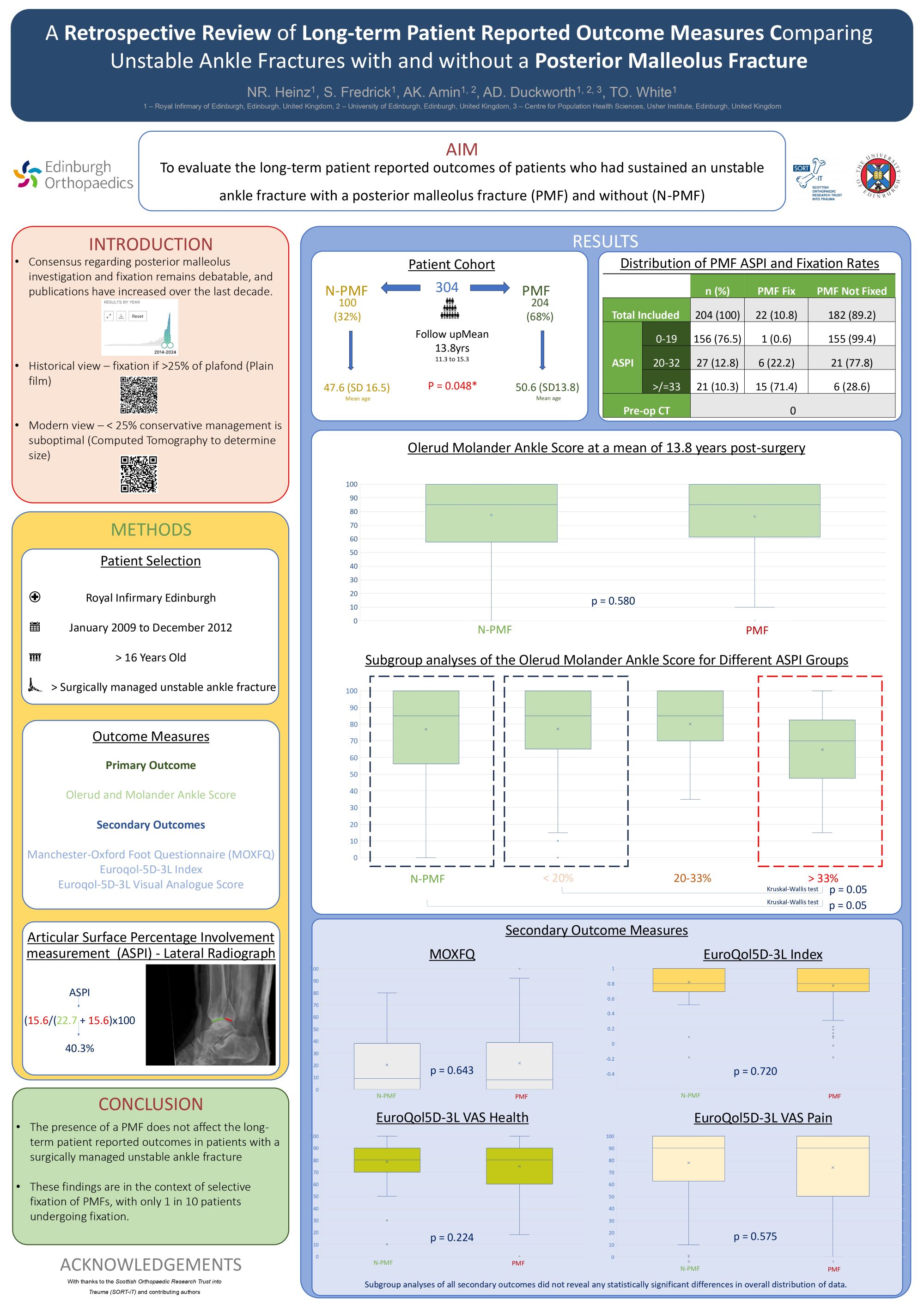
Nicholas Heinz1, Shawn Fredrick2, Andrew Duckworth2,1, Timothy White1, Anish Amin1,2
1Royal Infirmary of Edinburgh, Edinburgh, United Kingdom. 2University of Edinburgh, Edinburgh, United Kingdom
Abstract
Consensus regarding posterior malleolus investigation and management remains debatable. The aim was to evaluate the long-term outcomes of patients who had sustained an unstable ankle fracture with a posterior malleolus fracture (PMF) and without (N-PMF).
Patients over 16 years of age presenting to a single trauma centre between 2009 and 2012 with an unstable ankle fracture requiring surgery were included in the study. The primary outcome measure was the Olerud Molander Ankle Score (OMAS). Secondary outcomes were the Manchester Oxford Foot Questionnaire (MOXFQ) and EuroQol-5D-3L (EQ5D3L) Questionnaire. Patients received questionnaires at a minimum of 10 years post-surgery.
A total of 304/1500 patients have so far returned questionnaires, 204 (67%) PMF and 100 (33%) N-PMF. Patients with a PMF sustained their injury at a significantly higher age compared with those without a PMF (50.7 vs 47.6 years; p = 0.048). No patient received a pre-operative computed tomography scan. Only 10% of PMFs (22/204) were surgically stabilized. Comparison of median OMAS scores showed no statistical difference between groups (N-PMF 85 vs PMF 85, p = 0.580). There were no statistically significant differences for median MOXFQ (N-PMF 9 vs PMF 8, p = 0.643) and EQ5D-3L scores (N-PMF 0.8 vs PMF 0.8, p = 0.720). Subgroup analyses of PMF articular surface percentage involvement (ASPI) measured from presentation lateral plain radiographs showed that fractures with a PMF < 33% ASPI (178/204, 89.7%) showed no statistically significant difference for OMAS, MOXFQ and EQ5D when compared with the N-PMF group. Larger posterior malleolus fractures with ASPI of > 33% (21/204, 10.3%) did significantly worse than patients without a PMF for OMAS (p=0.012), EQ5D3L Index (p=0.035) and EQ5D3L VAS (p=0.040).
The lateral plain radiograph ASPI may be a useful tool regarding decisions for investigation and management of complex ankle fractures involving the posterior malleolus.
716 - Cerament bone void filler for the management of open fractures: Results from a major trauma centre over a 5 year period
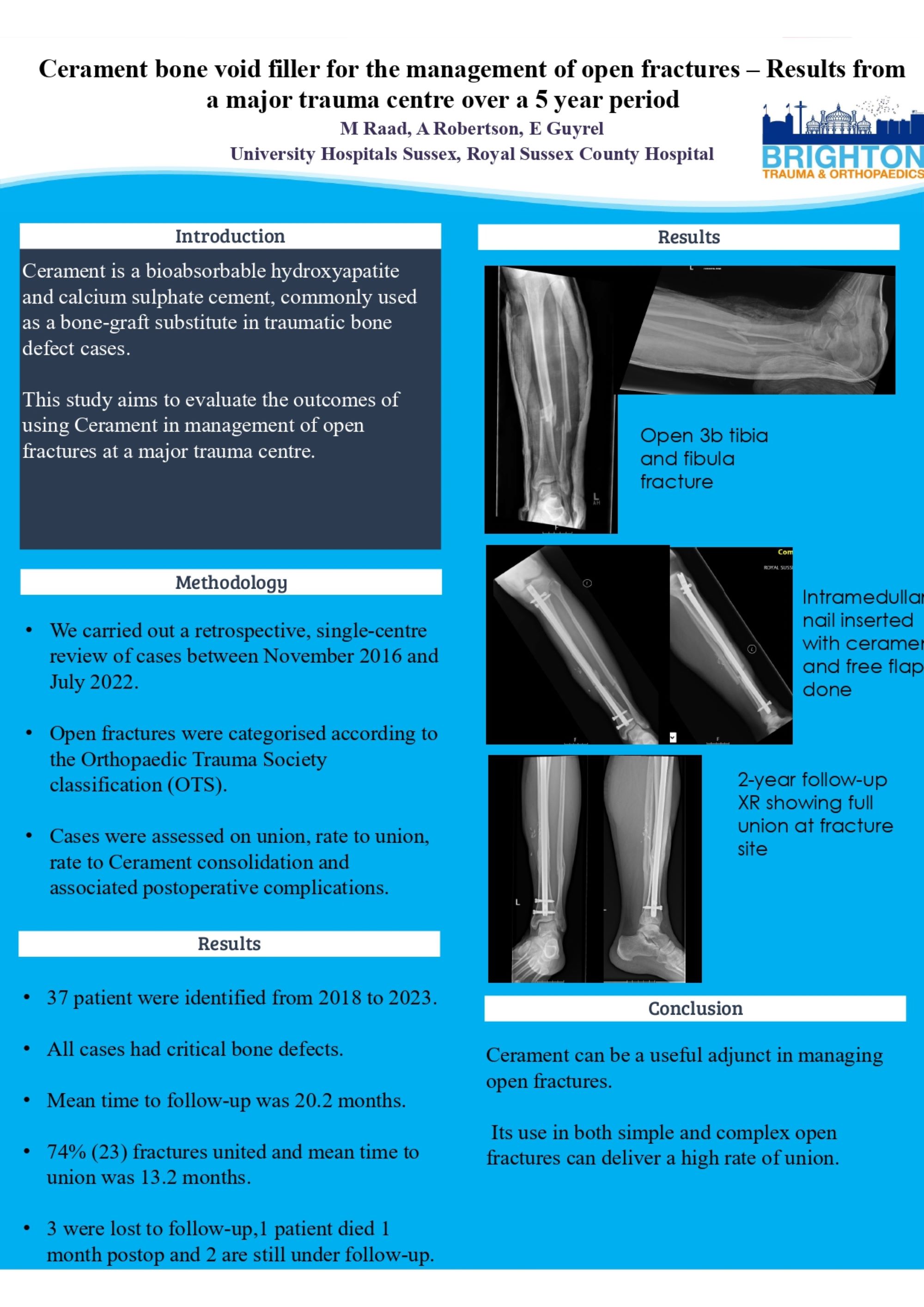
Marjan Raad, Peter Cay, Enis Guryel
University hospitals Sussex NHS foundation trust, Brighton, United Kingdom
Abstract
Background: Cerament is a bioabsorbable hydroxyapatite and calcium sulphate cement, commonly used as a bone-graft substitute in traumatic bone defect cases. This study aims to evaluate the outcomes of using Cerament in management of open fractures at a major trauma centre.
Method: We carried out a retrospective, single-centre review of cases between November 2016 and July 2022. Open fractures were categorised according to the Orthopaedic Trauma Society classification (OTS). Cases were assessed or union, rate to union, rate to Cerament consolidation and associated postoperative complications.
Results: Twenty-five patients were identified. Sixteen cases were classified as OTS simple open fractures and nine cases were complex open fractures requiring soft tissue reconstruction. One patient was lost to follow-up and one patient had limited follow-up beyond 5 months but showed evidence of progressive radiographic union. Of the remaining twenty-three cases, 19 cases (82.6%) went onto union with a mean time to union of 13 months (3 to 39 months). Persistent non-union remained in two cases (8.6%). Two cases had to return to theatre due to wound breakdown and infected skin graft respectively. The mean time to see Cerament consolidation on the radiograph was 12 months (3-39 months). One case had the complication of persistent weeping of Cerament from the wound. This self-resolved within two weeks. Limitations of this case series includes the lack of patient reported outcomes and the lack of complete follow-up in two patients (8%).
Conclusion: Cerament can be a useful adjunct in managing open fractures. Its use in both simple and complex open fractures can deliver a high rate of union.
859 - Comparison of clinical outcomes, operative duration and radiation exposure between suprapatellar and infrapatellar intramedullary nailing for tibial shaft fracture
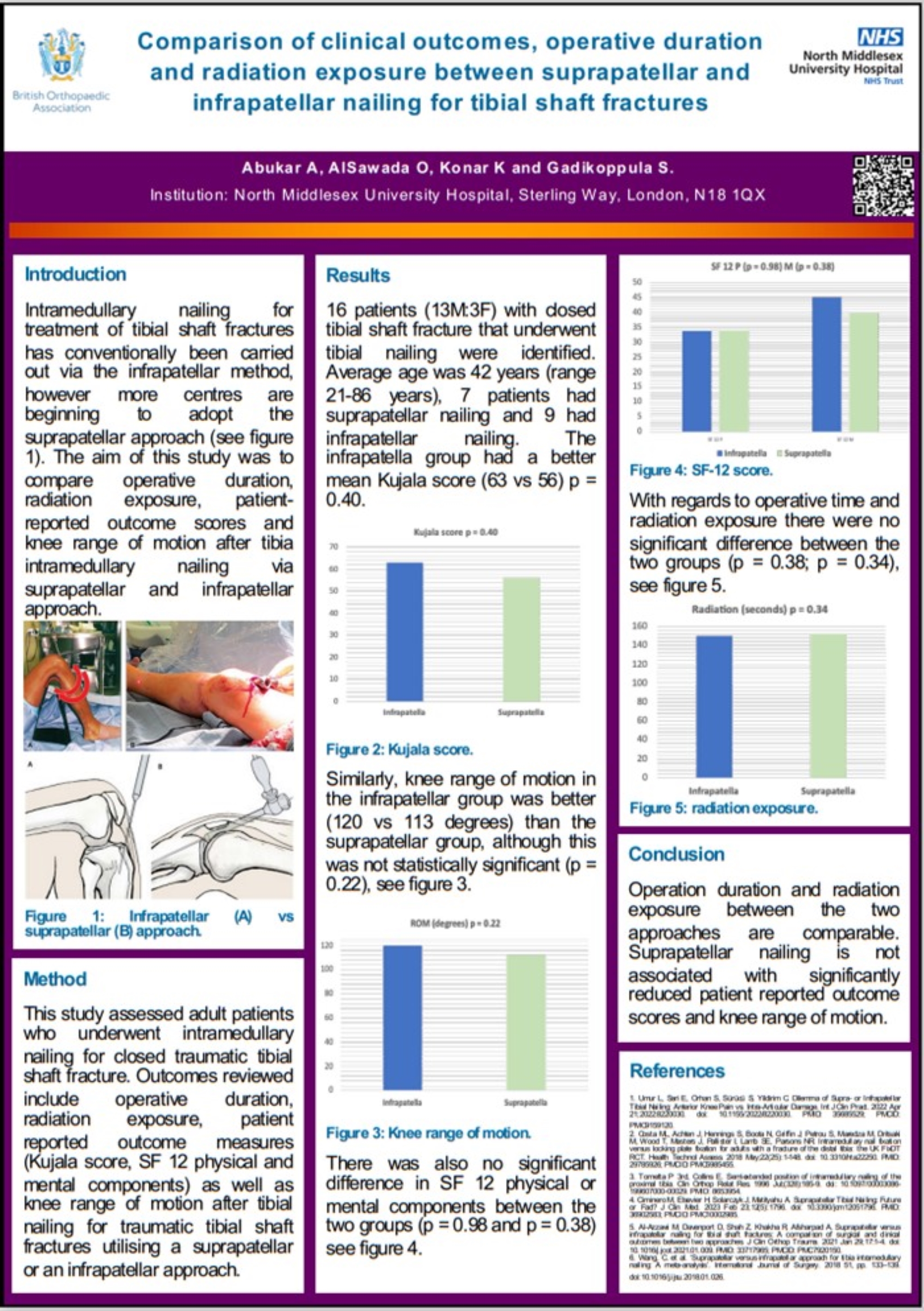
Amin Abukar1, Osama Alsawada2, Kishore Konar2, Srinivas Gadikoppula1
1North Middlesex University Hospital, London, United Kingdom. 2University College Hospital, London, United Kingdom
Abstract
Background: Intramedullary nailing for treatment of tibial shaft fractures has conventionally been carried out via the infrapatellar method, however more centres are beginning to adopt the suprapatellar approach. The aim of this study was to compare operative duration, radiation exposure, patient-reported outcome scores and knee range of motion after tibia intramedullary nailing via suprapatellar and infrapatellar approach at a DGH centre that did more infrapatellar approaches.
Method: This study assessed adult patients who underwent intramedullary nailing for closed traumatic tibial shaft fracture. Outcomes assessed include operative duration, radiation exposure, patient reported outcome measures (Kujala score, SF 12 physical and mental components) as well as knee range of motion after tibial nailing for traumatic tibial shaft fractures utilising a suprapatellar or an infrapatellar approach.
Results: 16 patients (13M:3F) with closed tibial shaft fracture that underwent tibial nailing were identified. Average age was 42 years (range 21-86 years), 7 patients had suprapatellar nailing and 9 had infrapatellar nailing. The infrapatellar group had a better mean Kujala score (63 vs 56) and knee range of motion (120 vs 113 degrees) than the suprapatellar group, although this was not statistically significant (p = 0.40; p = 0.22). There was also no significant difference in SF 12 physical or mental components between the two groups (p = 0.98 and p = 0.38). With regards to operative time and radiation exposure there were no significant difference between the two groups (p = 0.38; p = 0.34).
Conclusion: Operation duration and radiation exposure between the two approaches are comparable. Suprapatellar nailing is not associated with significantly reduced patient reported outcome scores and knee range of motion.
683 - Gravitational stress views overestimate ankle instability and may commit patients to unnecessary surgery: a prospective series with 10 year follow up
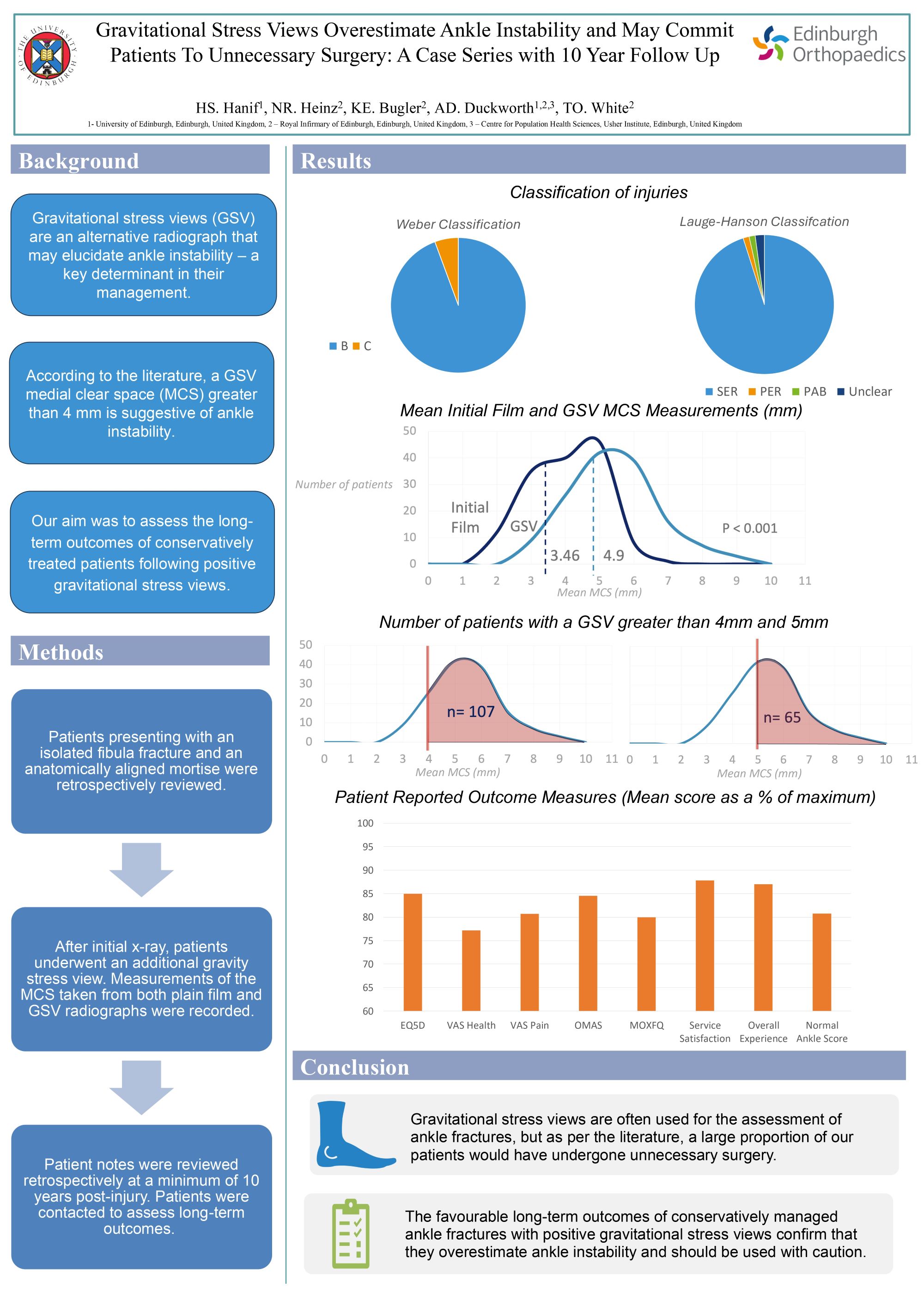
Nicholas Heinz1, Hamzah Hanif2, Kate Bugler1, Timothy White1, Andrew Duckworth2,1
1Royal Infirmary of Edinburgh, Edinburgh, United Kingdom. 2University of Edinburgh, Edinburgh, United Kingdom
Abstract
Gravitational stress views (GSV) may be a convenient and less painful alternative to manual stress testing. The aim of this study was to assess whether this test accurately predicts ankle instability.
Patients presenting to a single trauma centre between 2011 and 2013 with an isolated fibula fracture and a an anatomically-aligned mortise on initial plain film radiographs were reviewed. After initial x-ray, patients underwent a gravity stress view. Measurements and assessment of plain films were recorded and analysed. Electronic case notes and National Imaging Archives were reviewed retrospectively at a minimum of 10 years post-injury. Patients were contacted to complete patient reported outcome measures (PROMS).
One-hundred and forty-two (142) patients met the inclusion criteria and were included in the study. Mean initial film medial clear space (MCS) measurement was 3.46mm (SD1.0, range 1.0 to 6.0) compared to GSV MCS that was 4.9mm (SD1.3, range 2.0 to 8.8; p<0.001). No patient underwent surgery and all patients had successful conservative management with anatomical union seen at their 6 week radiograph. No patient returned with a complication related to their ankle fracture during the follow-up period. With a MCS acquired from GSV of >5mm, 65 patients would have undergone unnecessary surgical intervention. At MCS of >6mm, 26 patients would have undergone surgery unnecessarily and at a MCS of >7mm 10 patients would have had unnecessary surgery. To date, 50 patients have provided PROMs. Mean Olerud and Molander Score (OMAS) at 10 years was 86.63 (SD 23.27, 95% CI 79.47 – 93.79), Manchester Oxford Foot Questionnaire (MOXFQ) was 79.41 (SD 32.94, 95% CI 69.39 – 89.42) and Euroqol-5D-3L was 0.86 (SD0.22, 95% CI 0.79 – 0.93).
Stress views may over-diagnose instability in patients with an isolated fibula fracture in an otherwise normal initial radiograph.
Disclosure - None
