Private Healthcare Information Network (PHIN) update
4th March 2024
The updated version of Good Medical Practice came into effect on 30th January 2024. This includes advice on ‘Being open with patients about your fees and charges’ and within this there is now a section on the requirement to submit fee information to PHIN as set out in the Private Healthcare Market Investigation Order, 2014 as amended.
The majority of consultants are providing fee information, with 84% of Orthopaedic consultants submitting their data, however, only around 50% of consultants have validated their data, that is around 1,500 consultants that risk inaccurate data – which is submitted by the hospital – appearing on the website if they do not respond to the numerous prompts made by PHIN. Presumed publication of data is scheduled for Autumn 2024.
PHIN will launch a new portal for consultants during March 2024. The changes are based on feedback PHIN received from consultants and include:
- Consultants will be able to provide information on their fee arrangements with insurers, in addition to information about fees charged to private self-pay patients for consultations and procedures.
- Consultants will be able to nominate a delegate to work with them to submit and manage data to fulfil these activities.
- A Consultant Overview Report.
The new Overview Report will provide information about:
- Volumes of activity.
- Length of day (showing both inpatient and day case activity).
- PROMs information where these are collected for specific procedures (link to list).
- Adverse Events.
N.B. Volume, Length of Stay and Patient Feedback are the only consultant measures published on the public PHIN website – and only data verified by consultants will continue to be published. As currently, consultant data about Adverse Events, Never Events and PROMs will only be available privately in the PHIN portal.
Consultants with eight or fewer episodes of data in any publication period will not have data published; patient feedback will only be published when more than 30 responses have been received.
The Acute Data Alignment Programme (ADAPt)
The ADAPt initiative involves PHIN sharing the private Admitted Patient Care (APC) data it collects from independent providers with NHS England on a regular basis, with effect from April 2024.
To comply, providers will have to:
- Amend their privacy notices.
- Record patient opt-out data.
- Improve NHS number collection and submission.
Background
The Acute Data Alignment Programme (ADAPt) was initiated at a meeting between the Secretary of State for Health and Social Care and representatives from NHS Digital and the Private Healthcare Information Network (PHIN) on 9th January 2018. This followed the conviction in April 2017 of breast surgeon Ian Paterson for harming his patients. He practiced at the Heart of England Foundation Trust and Spire Healthcare. The Secretary of State asked the two organisations to work together to ensure that private healthcare data could be properly captured and analysed within NHS systems.
The ADAPt programme was established and is being jointly led by PHIN and NHS Digital (now part of NHS England), in partnership with the Department of Health and Social care (DHSC), NHS Improvement (now part of NHS England), NHS England (NHSE), the Care Quality Commission (CQC) and other bodies.
The ‘ADAPt vision’ is:
‘To bring about an alignment in data standards, measurement and reporting systems across NHS and private healthcare in order to enable greater transparency in quality and safety, and to support patient choice and opportunities for improving patient care.’
The Programme’s originally stated benefits were as follows:
- The provision of a joined-up view of a patient’s medical (hospitalised) history, irrespective of whether their treatment was in a public or private setting, thereby providing insights into quality and safety enabling better and safer care.
- The ability to derive comparable indicators across both care settings.
- Ability to analyse patient pathways across both NHS funded and private healthcare for example measuring the impact on the NHS of patient outcomes following private care and vice-versa.
- Increase the transparency of information across public and private healthcare sectors to the public, clinicians, commissioners, and others to support effective decision making.
- Improve the use of the NHS number in private healthcare settings, an essential element in enabling data sharing between the private and public care settings.
- Support the provision of data to other bodies who play a role in ensuring the quality and safety of health and care services (where a suitable legal basis exists) e.g. the Care Quality Commission (CQC), to improve their intelligent monitoring of independent hospitals.
- Support consultant revalidation with a more comprehensive set of workload and performance information.
- Support for whole population analysis and research by including the significant volumes of independently funded healthcare activity which has to date not been available for such analyses.
- Supporting better system alignment, efficiency and oversight between the private and NHS sectors.
- Reducing the burden on healthcare providers associated with duplicate flows of data.
Subsequent to these initially stated benefits, one of the key recommendations from the Paterson Inquiry included:
‘A single repository of consultant data in England detailing their practising privileges and other critical consultant performance data including volume of procedures undertaken to be made available to the public and mandated for use by managers and healthcare professionals in both the NHS and independent sector.’
Furthermore, following the launch of the new Outcomes and Registries Programme by NHS England, ADAPt will also provide a vital means of measure case ascertainment across the independent sector.
What is the scope of ADAPt?
- Included - APC data related to private patients treated at independent and NHS Private Patient Unit (PPU) hospitals located in England.
- Excluded - APC data related to private patients treated at independent and NHS Private Patient Unit (PPU) hospitals located in Wales, Scotland and N. Ireland.
- All other datasets collected by PHIN from independent and NHS Private Patient Unit (PPU) hospitals in the UK:
- PROMs.
- Patient Feedback.
- Adverse Events
The approach approved by NHS England and PHIN’s Board
The lawful basis for PHIN sharing the private APC data it collects from independent providers with NHS England on a regular basis will be a Direction from the Secretary of State for Health and Social Care, instructing NHS England to request the data from PHIN. PHIN will rely on Public Interest for the sharing of this data.
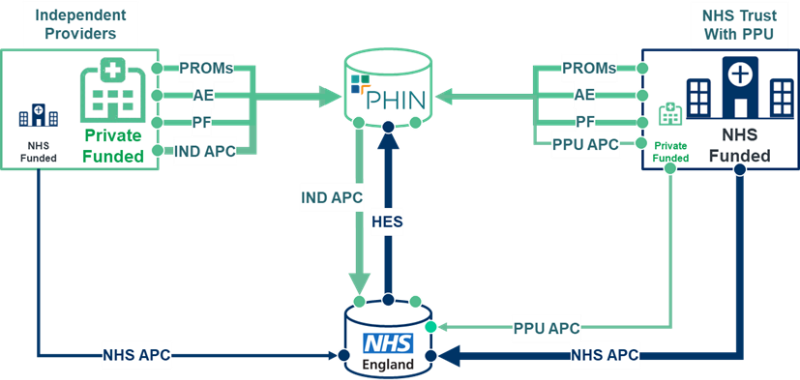
N.B. Only private APC data is in scope of ADAPt. The remaining datasets which PHIN collects (PROMs, Adverse Events and Patient Satisfaction), are all out of scope.
Is there an opt-out for data sharing with NHSE?
While not a legal requirement, the ADAPt Board has decided to allow private patients to opt-out of having their NHS Numbers shared for individual episodes of private care.
The ADAPt Board has also taken advice in regard to consultant data opt out and agreed that data submitted to PHIN with procedures attributed to consultants will be included in extracts onward submission to NHS England. There will be no opt-out for consultants.
