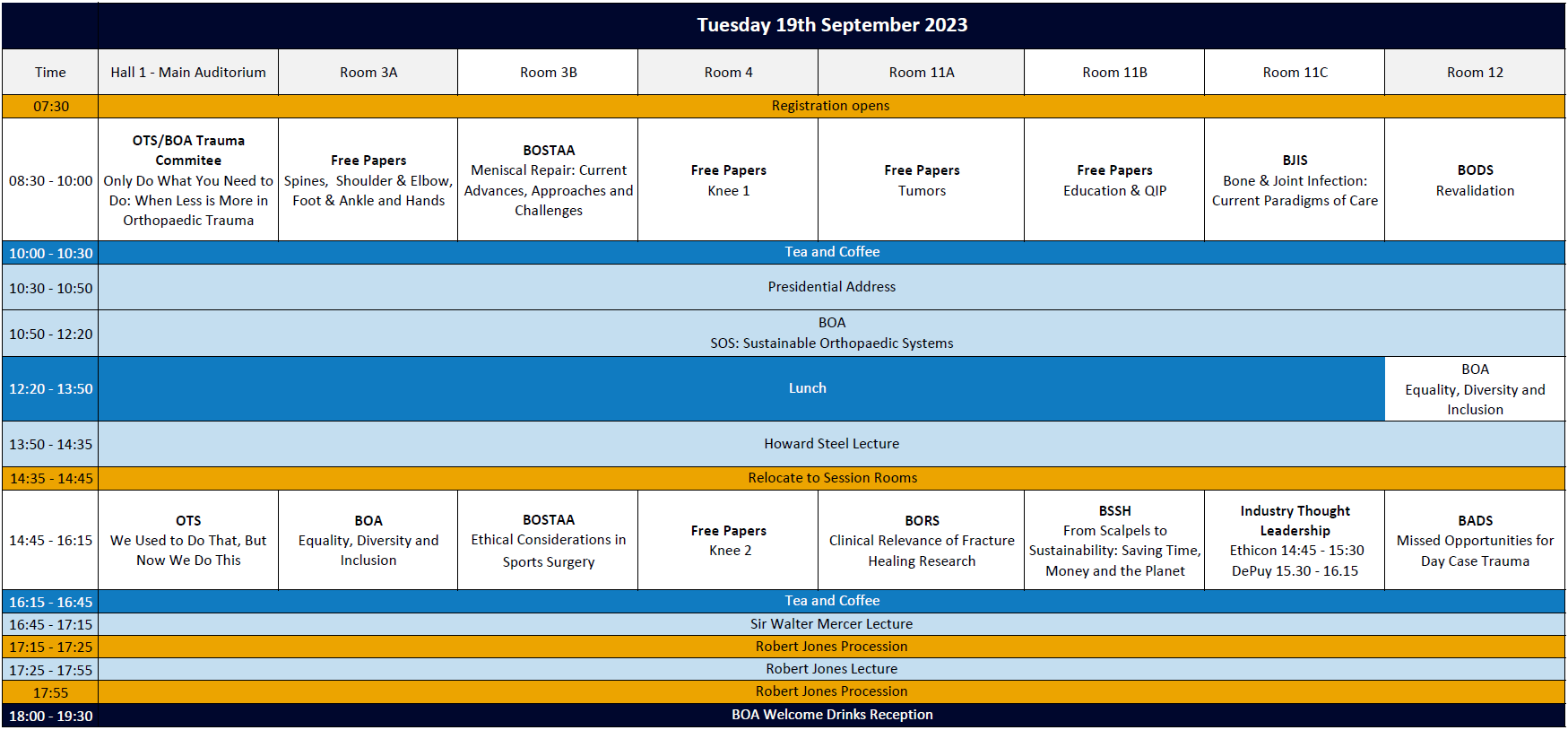
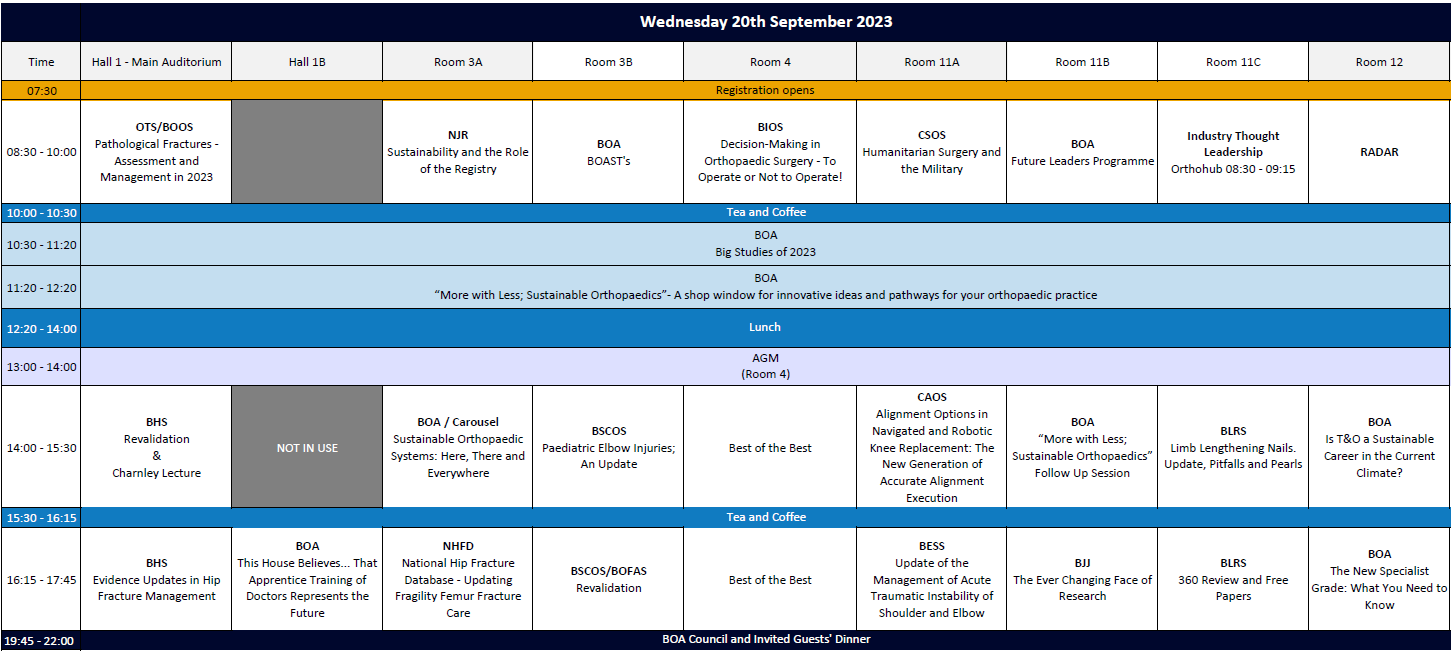
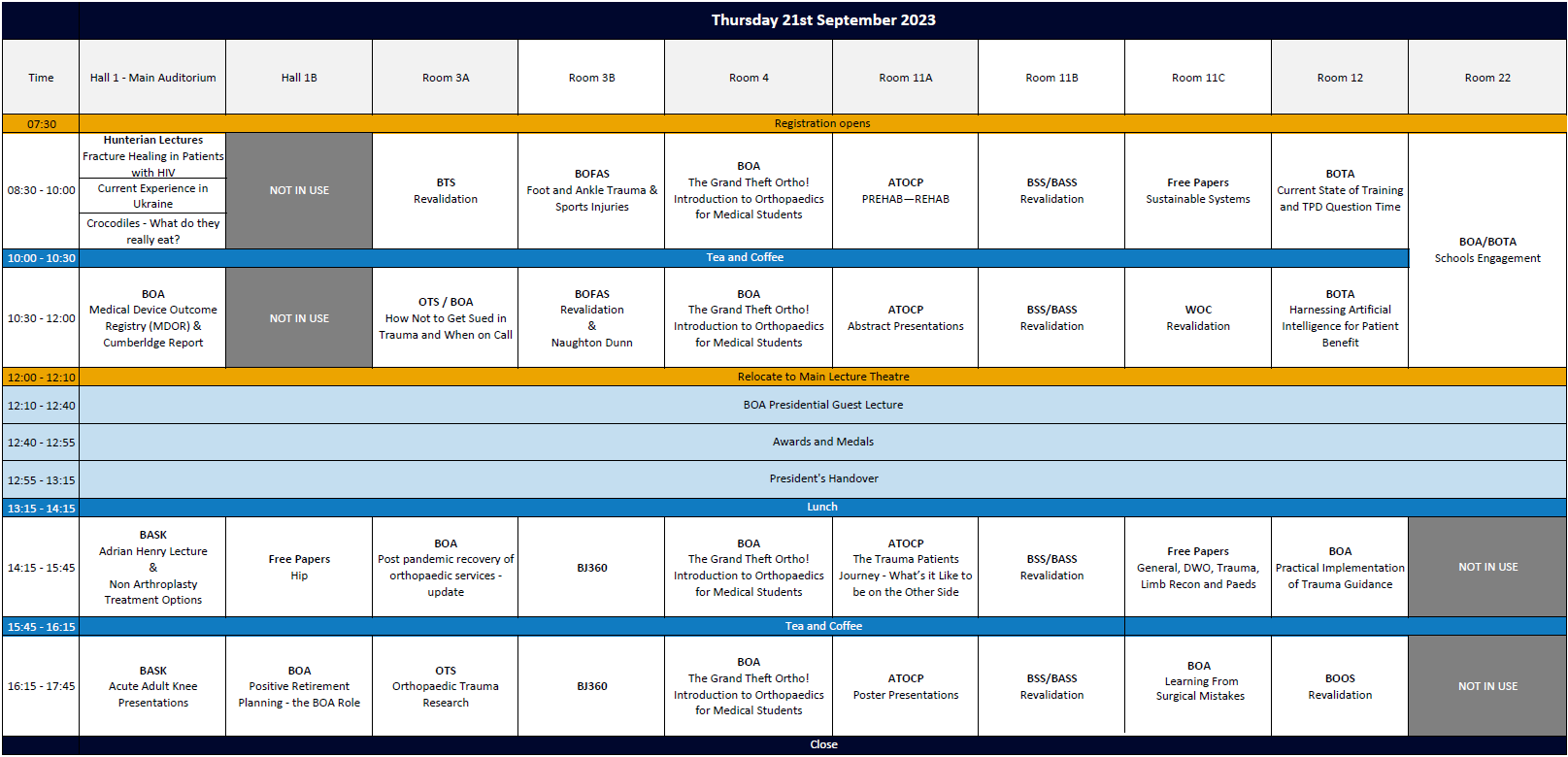
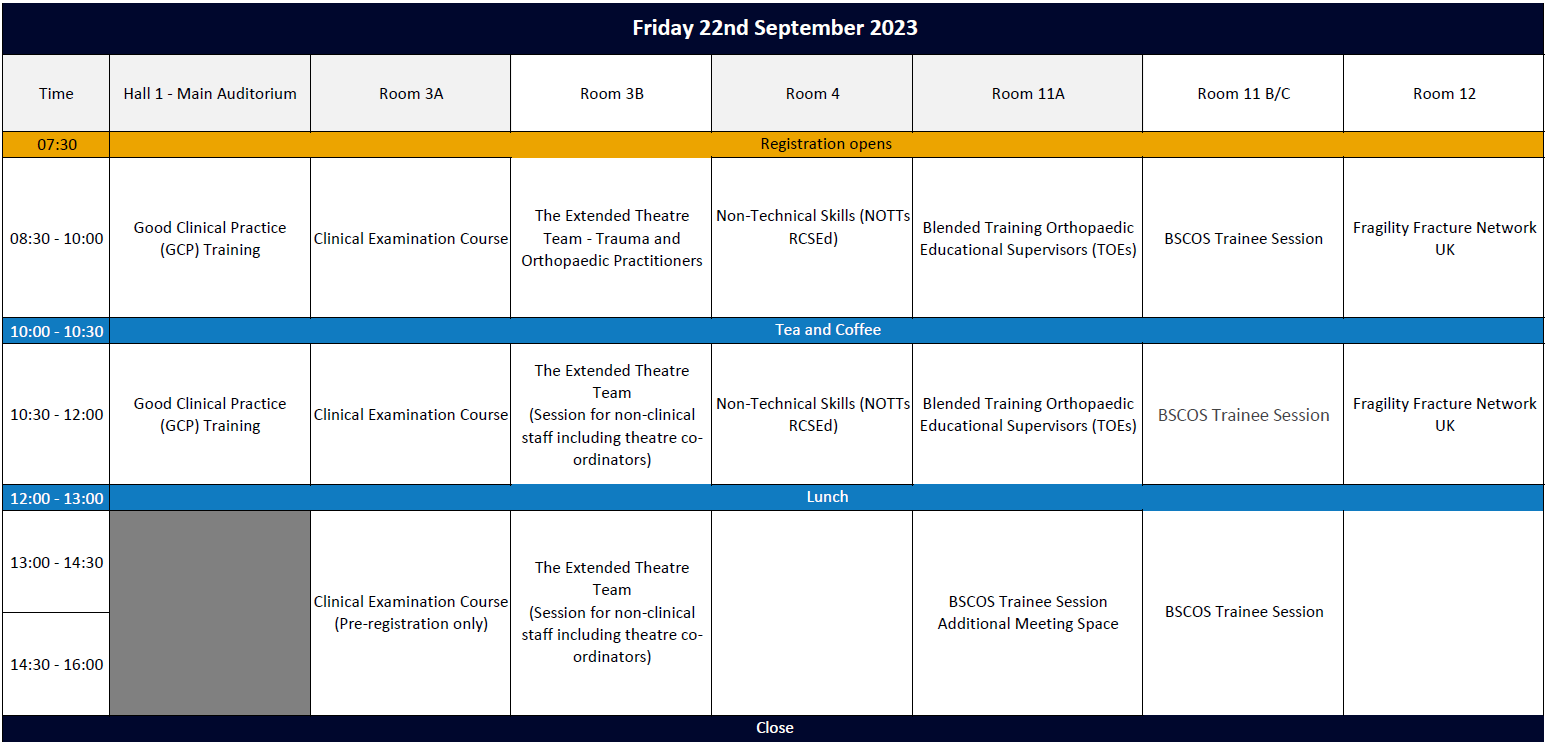
Programme
The theme for the BOA Annual Congress 2023 is 'Sustainable Systems'. Congress registrants can view session recordings by clicking the button below:
Congress session recordings
Return to the Congress homepage
Should you have any queries please contact the BOA Events team at [email protected].