CORESS - A Confidential Reporting System for Surgery to disseminate lessons learnt from unexpected or adverse incidents
Authors: Robyn Brown, Dominic Waugh, Harriet Corbett and John Machin
CORESS - A Confidential Reporting System for Surgery to disseminate lessons learnt from unexpected or adverse incidents
Robyn Brown is an ST7 orthopaedic registrar who has led award-winning improvement projects and is currently focused on improving safety culture, civility, radiation protection and burnout. Robyn has a passion for patient safety and workforce welfare with past roles including HEE-SW Patient Safety Fellow, RCSEng Emerging Leaders Fellow and Severn Orthopaedics Welfare Representative. She is currently a CORESS Academic Fellow as well as being a BOA Culture & Diversity Champion.
Dominic Waugh is a Trauma and Orthopaedic ST5 on the West of Scotland rotation and current BOTA Treasurer. He is a committed advocate for surgical safety, having completed the inaugural BOTA–CORESS Fellowship and now serving on the CORESS Advisory Board. Through leadership and education, he supports national efforts to improve training, patient safety, and systems thinking, while helping trainees navigate the challenges of a surgical career.
Harriet Corbett is a consultant paediatric urologist at Alder Hey Children’s Hospital, Liverpool. Her clinical practice concentrates on bladder function and general paediatric urology. Harriet holds an NIHR Senior Clinical Research Practitioner Award and is an Honorary Senior Lecturer in Child Health at the University of Liverpool. She is passionate about surgical safety and is the CORESS Programme Director, having been a member of the advisory board since 2015.
John Machin is a consultant orthopaedic surgeon specialising in hip and knee surgery at Chelsea and Westminster Hospital. He is co-lead for Litigation at GIRFT, working with Professor Tim Briggs and NHS Resolution to ensure care is improved from reviewing clinical negligence claims. John has also co-authored and contributed to the GIRFT national reports and the NHS Patient Safety Strategy. John sits on the advisory board for CORESS.
What is the (ongoing) problem?
Adverse incidents, errors and ‘near misses’ in surgery continue to occur on a regular basis despite the efforts of key stakeholder organisations. Of the 370 ‘never events’ recorded by NHS England between April 2023 and March 2024, more than 80% were surgical incidents1. Previous analysis of trauma patients undergoing fracture fixation has demonstrated a surgical error rate of up to 8.7%, with up to 30% of these incidents having potentially significant consequences2. In 2023-24, NHS Resolution costs were £2.9 billion (1.5% of the NHS budget), with £58.5 billion set aside for future liability claims3. While the GIRFT litigation work stream, off the back of providing litigation data packs to all acute and specialist trusts in England, has highlighted a relative reduction in trauma and orthopaedic claims volume (including orthopaedic spinal surgery) from 10% in 2013/14 to 3.2% in 2023-243,4, the direct costs to the NHS Trusts continue to represent around £145 million per annum on average4. The costs incurred are not only financial: in 2015, it was estimated that up to 3.6% of hospital deaths were avoidable5. These numbers reinforce the need for robust systems to report, analyse and learn from patient safety incidents as they occur.
Errors must be recorded and analysed to ascertain how they can be prevented in future. Such reporting systems have traditionally focused around satisfying clinical governance frameworks, policy, and regulation. Although these systems are crucial for maintaining protection of the public, barriers to reporting patient safety incidents can prevent recording of incidents. While a fear of ‘blame’ and the associated cultural barriers remain a significant challenge to incident reporting in the National Health Service6, learning from error and effective dissemination of lessons learned remains an important means to prevent recurrence.
Whilst there have been a number of local and regional initiatives, as featured in this journal, which have supported the need to learn from mistakes and near misses there is a need to collect and share this important information on a national scale to share learning across the regions. There is an expectation from our patients that surgical teams learn from mistakes. NHS Resolution reported that the most common cause for claims was patients, ‘wanting to prevent similar things happening to others7.
What is CORESS?
Founded in 2006, the Confidential Reporting System for Surgery (CORESS) is a national reporting and learning system established exclusively to confidentially share lessons learnt from unexpected or adverse incidents in surgical practice with the surgical community. Adapting a similar model developed by the aviation industry following a series of high-profile accidents, CORESS adheres to the following principles overseen by an independent board:
- Complete confidentiality between the reporter and CORESS. This is to encourage submission of reports and attenuate any influence of a ‘blame culture’. Although reporter details are requested to submit a report, identifying details are known only to the CORESS programme director. All identifiable data is removed before a report is reviewed by the advisory board.
- The educational feedback to both the reporter and associated professional body must be excellent for there to be confidence in the credibility of CORESS.
- Reviewers must include those who actively practice their profession. Incident analysis from CORESS is provided by a pan-specialty advisory board of practicing surgeons from all specialties. Other advisory board members comprise lay people, surgical resident doctors, anaesthetists, nurses, legal representatives, members with human factors expertise, medical defence experts and representatives of Royal College, Association for Perioperative Practice representatives and the Getting It Right First Time Programme.
- The board is independent of any authority and is led by the CORESS programme director, who acts as an independent chair.
- The CORESS system is complementary to existing statutory, professional, and organisational measures for the protection of the public and does not replace them. CORESS does not replace any established trust or regulatory reporting system and reporters are encouraged to report to these systems if felt necessary.
Why should I submit to CORESS?
Unlike other reporting systems, CORESS does not systematically analyse and feedback information to NHS organisations. It is run by surgeons to disseminate feedback widely to the surgical community on the learning contained in reports in a manner that is both effective and anonymous.
Reporters are provided with a dedicated space for reflection following the incident before the benefit of an expert review which may highlight further learning points for review. Time and resource constraints, alongside psychological safety, often don’t allow this degree of learning in their clinical environment. A certificate of contribution is provided which can be included in their continuing professional development portfolio as evidence of contribution to surgical safety. This may be useful for resident doctors (for example, at annual review of competence progression), or as evidence for appraisal or revalidation.
More broadly, submissions are required to provide educational content for publications benefitting reporters, readers, and the whole surgical community. CORESS relies on engagement of the surgical community for them to then benefit from its content.
How and what do I submit to CORESS?
Any surgeon, surgical trainee or member of the surgical team may submit a case to CORESS, by an online reporting form (which can be accessed at https://coress.org.uk/online-reporting-form/ or by using the QR code in figure 4)8. CORESS encourages submissions related to patient safety issues where lessons can be learned and shared with the professional community (Figure 1).
Figure 1: CORESS Online Reporting Form. Any surgeon, surgical trainee or member of the surgical team may submit a case to CORESS easily via this simple form which can be accessed at https://coress.org.uk/online-reporting-form/.
Reports may concern any safety-related incident involving the reporter, other people, or a hospital / organisation where the reporter works. Incidents may include: diagnostic or operative errors, near misses, technical or maintenance failures, regulatory or procedural aspects or unsafe practices and/or protocols. Useful lessons may often be learned from incidents which do not result in adverse consequences and may only be known to the reporter.
Orthopaedic submissions have previously included examples such as:
- Escape of a humeral head fracture fragment onto the floor during a proximal humerus open reduction internal fixation (Figure 2).
- Colleague needlestick injury due to limited surgical field through loupes during an elective hand operation.
- Wrong site marking in a Total Knee Replacement.
The programme director receives case reports through the online reporting form, then removes all identifiable data before review by the advisory board. The board discussion aims to establish and formalise key learning points of the case. Those learning points are summarised into feedback comments (e.g. Figure 3) which are incorporated into published feedback articles in a range of surgical college journals as well as publication of a ‘Case of the Month’ on the CORESS website. Historic cases can be found on the resources page of the CORESS website and a searchable database will be available by the end of 2025.

Figure 2: An example CORESS case submitted via the online reporting form. The case was discussed by the Advisory Committee with reflective learning points then summarised ready for publication.
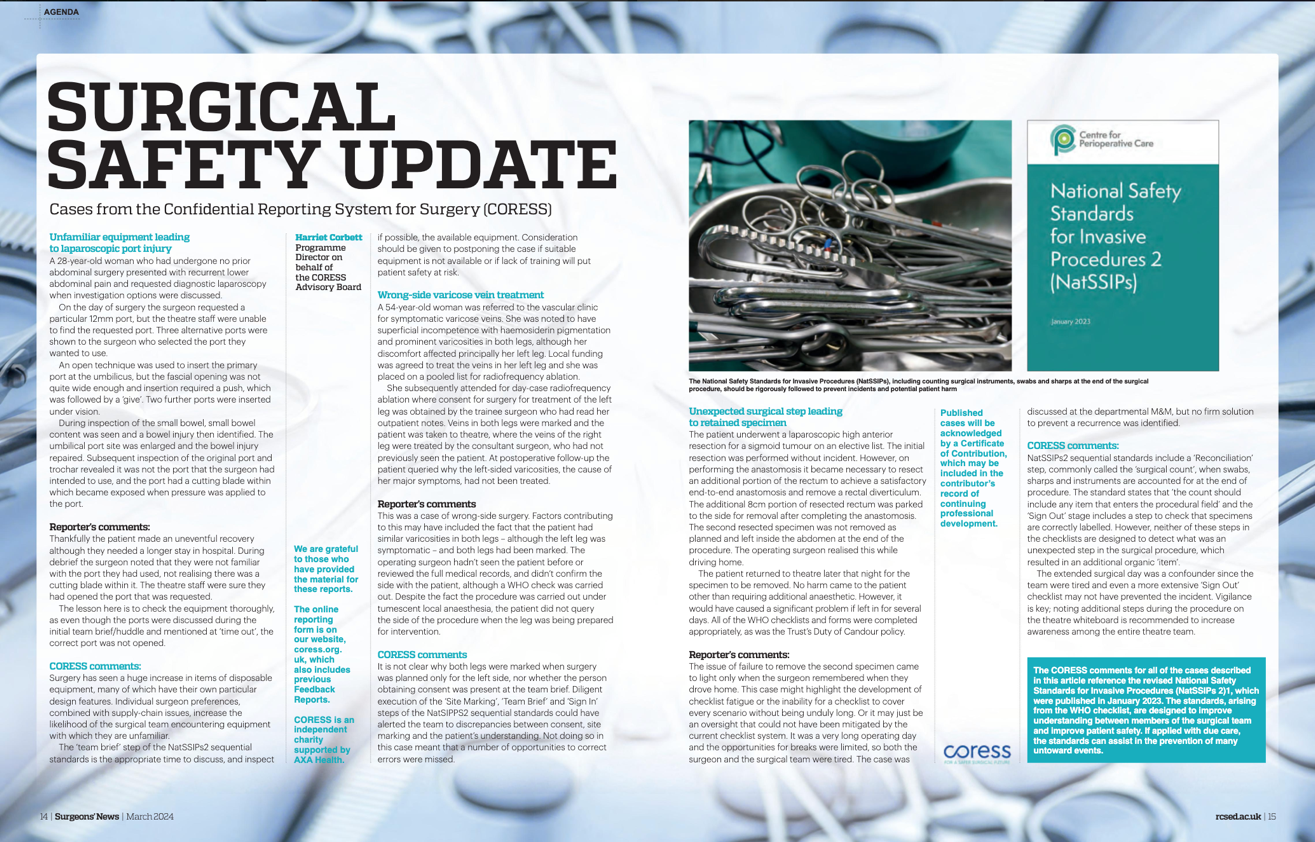
Figure 3: Example CORESS publications in RCSEd Surgeon’s News. Available at: www.rcsed.ac.uk/news-resources/publications/surgeons-news.
How can I read and use CORESS case reports?
Accessing published reports provides not only opportunities for remote individual learning, but also examples to use in group case-based discussions.
An archive of all cases are available for download on the CORESS website (https://coress.org.uk/reports-download) and published quarterly within journals such as RCSEng Annals and RCSEd Surgeon News. Many specialties also publish cases in their specialty-specific newsletters and journals. A database enabling specialty-specific categorisation and ‘search and retrieval’ of cases using keywords is under construction.
A Case of the Month is published on the CORESS website (https://coress.org.uk/case-of-the-month). Although these cases arise from a wide range of specialties, there are many generalisable learning points drawn out of them in which orthopaedic surgery can learn.
What else does CORESS do?
On a wider scale, CORESS interacts with other organisations including the Medicines and Healthcare Products Regulatory Agency, the Healthcare Safety Investigation Branch, Getting It Right First Time, NHS England and the National Confidential Enquiry into Patient Outcome and Death. CORESS has also made substantial contributions to the NHS England Never Events Taskforce, to the National Safety Standards for Invasive Procedures and to the National Patient Safety Response Advisory Panel.
Summary
Amongst the existing regulatory and governance mechanisms dominating patient safety frameworks, CORESS provides a psychologically safe system for surgeons to confidentially communicate and share learning from adverse events without fear of blame. Useful publications rely on active surgical community engagement through submissions that can then benefit both individual readers and the safety education curriculum.

Figure 4: QR code linking to CORESS website to submit incident report.
References
- NHS England. Provisional Publication of Never Events Reported as Occurring Between 1 April and 31 March 2023. Available at: www.england.nhs.uk/wp-content/uploads/2023/07/provisional-never-events-april-23-31-march-24.pdf.
- Bosma E, Veen EJ, Roukema JA. Incidence, nature and impact of error in surgery. Br J Surg. 2011;98(11):1654-9.
- NHS Resolution Annual Report and Accounts 2023/24 [Released July 2024] Available at: https://resolution.nhs.uk/wp-content/uploads/2024/07/NHS-Resolution-Annual-report-and-accounts_23-24_Access-1.pdf.
- Machin JT, Forward D, Briggs T. Clinical negligence: is orthopaedics learning from it? Bone Joint 360. 2020;9(4):6-10.
- Hogan H, Zipfel R, Neuburger J et al. Avoidability of hospital deaths and association with hospital-wide mortality ratios: retrospective case record review and regression analysis. BMJ 2015;351:h3239.
- Radhakrishna S. Culture of blame in the National Health Service; consequences and solutions. Br J Anaesth. 2015;115(5):653-5.
- Behavioural insights into patient motivation to make a claim for clinical negligence [Released August 2018] Available at: https://resolution.nhs.uk/wp-content/uploads/2018/10/Behavioural-insights-into-patient-motivation-to-make-a-claim-for-clinical-negligence.pdf.
- Smith F, Corbett H. The Confidential Reporting System for Surgery: CORESS. Ann R Coll Surg Engl. 2023;105(8):683-4.
