Green issues in anaesthesia
By Emma Evans
Consultant Anaesthetist, St George’s University Hospitals NHS Foundation Trust, SW London Clinical Lead Net Zero
Since the NHS set out its ambitions to reach Net Zero1 a great deal of deliberation and effort has gone into how to reasonably achieve this, including addressing the impact of volatile anaesthetic gases and other theatre practices on the carbon burden of surgery.
Surgical procedures are carbon heavy2, through the combination of consumables, clinical waste generated, energy demands of equipment, air handling units and temperature regulation required, as well as anaesthesia itself. Anaesthesia emissions are mainly due to the radiative climate impact of halogenated anaesthetic gases and nitrous oxide, in some cases, over many years.
So what have the anaesthetic fraternity done to address this burden?
Anaesthetists have risen to this challenge and use of desflurane, the highest impact agent with a GWP of 2,540 times that of carbon dioxide, has dwindled dramatically. In November 2022, the Royal College of Anaesthetists (RCoA) and Greener NHS set out their intent to decommission use by early 2024 apart from exceptional clinical cases. Desflurane had offered so much at its introduction into clinical practice in terms of recovery time and airway safety, particularly in bariatric surgery, but gradually both the clinical evidence for its superiority over other agents and its huge relative financial and emission burden, has left the majority of anaesthetists waving goodbye to it quite happily.


Achieving reductions in nitrous oxide emissions has been far more of a challenge and the emphasis has been more on identifying and eliminating poor manifold and pipeline processes than withdrawing this historical gas from anaesthetic practice. The national nitrous oxide mitigation project ‘Nix the Nitrous’3 followed improvement work in Scotland which demonstrated that up to 90% of manifold nitrous oxide never sees a patient. This reflects not only that 21st century anaesthetic practice now no longer mirrors historical infrastructure requirements for piped nitrous oxide, but also shines a light on the poor condition of many NHS estates. Greener NHS is now driving emissions reduction programmes and changes in national policy have followed suit. These include removing the requirement for piped nitrous oxide from building regulations and decommission mandates are now part of the NHS 2023/24 contract4. As such, multi disciplinary teams across the country are working collaboratively to eradicate nitrous oxide waste by decommissioning manifolds and installing cylinder supplies instead. We eagerly await data to demonstrate the effectiveness of this complex work. Along with its recent class C criminalisation status outside of medical care, nitrous oxide remains firmly under the spotlight.
Which anaesthetic technique is the least carbon intensive?
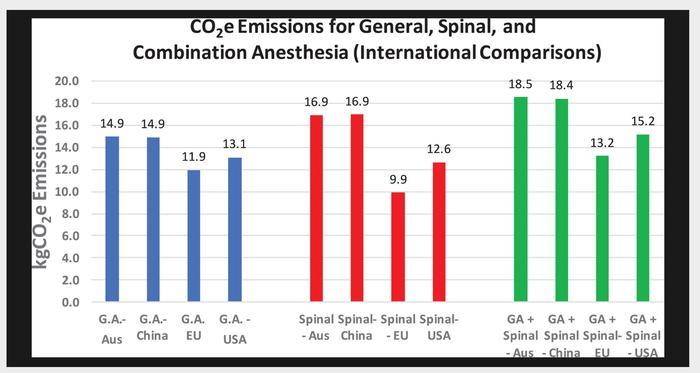
Decarbonising anaesthesia draws on the relative difference in carbon footprints between agents and techniques, both inhalational and intravenous. Total intravenous anaesthesia (TIVA) currently has a tiny relative carbon footprint even accounting for the need for plastics consumables, pumps and depth of anaesthesia monitoring. There is a caveat to this as more research may reveal the ultimate aquatic impact of propofol metabolites but for now TIVA rules the roost. Local or regional anaesthesia are also much lower carbon techniques than inhalational, particularly when combined with pragmatic oxygen flows, reusable sterile linens and renewable energy sources5. We now need teams to critically examine what surgery can feasibly be performed under these conditions while achieving the same clinical outcomes.
What framework are anaesthetists using?
Sustainable anaesthesia, like sustainable surgery, uses the framework of the four pillars of sustainable models of care6, some examples of which are:
|
Pillar |
Examples of work being done |
|
Disease prevention and heath promotion |
Providing information about the co benefits of optimising chronic health conditions or lifestyle on anaesthetic outcomes |
|
Patient empowerment |
Cllaborating on surgery school programmes, use of patient portals for information about anaesthesia, patient information about the carbon footprint of anaesthesia7 |
|
Lean service delivery |
Making every second count in theatre sessions, streamlined virtual pre-op assessment, growth of ambulatory work and one stop shops models of care with surgical colleagues, using data to improve utilisation |
|
Low carbon options |
Growing the use of reusables across airway equipment, linens, BP/saturation monitoring Decarbonising iv to po drug administration such as iv paracetamol, like surgical colleagues rationalising anaesthetic procedure packs, moving away from ethyl chloride for block assessment, debating the value of sterile gowns in line/block insertion, converting to use of alcohol based hand rub |
The RCS Green Theatre Checklist offers a comprehensive evidence base for much of the work that can still be done to decarbonise surgery and anaesthesia whilst evaluating the triple bottom line of high quality, safe clinical outcomes, carbon impact and what are often not insignificant financial savings. Going through sequential small PDSA cycles and accumulating incremental gains are key to innovating around current care pathways, moving towards one stop shop models of care and taking us beyond scope 1 and 2 emissions (below) where the mainstay of NHS emissions lies.
And at the core of all of this is the patient. The patient now who gains from our focus on the quality, cost and carbon impact of their analgesia, anaesthesia, convenient care pathways and energy efficient use of our clinical areas and the patient of tomorrow who gains from the cumulative contribution our actions make to the ability of the NHS to continue to be accessible and high quality into the future. Much of the work we seek to do just makes sense to the patient and the more we can involve them in co-designing our improvement work the better.
Ultimately collaboration is king. It extends to our roles as change makers, as advocates, and through our voices and actions both at home and at work. You will find other champions around you in the operating theatre and beyond and anaesthetists are totally with you on this agenda.
References
- NHS England. Delivering a Net Zero NHS. Available at: www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2022/07/B1728-delivering-a-net-zero-nhs-july-2022.pdf.
- Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta MF. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann Surg. 2020;272(6):986-95.
- Chakera A. (2020) Reducing the Impact of Nitrous Oxide Emissions within Theatres to Mitigate Dangerous Climate Change. Evidence-Based Policy Brief Dissertation. University of Edinburgh
- NHS England. NHS Standard Contract 2023/24 Technical Guidance. Available at: www.england.nhs.uk/wp-content/uploads/2023/03/08-nhssc-contract-technical-guidance.pdf.
- McGain F, Sheridan N, Wickramarachchi K, Yates S, Chan B, McAlister S. Carbon Footprint of General, Regional, and Combined Anesthesia for Total Knee Replacements. Anesthesiology. 2021;135(6):976-91.
- Mortimer F. The sustainable physician. Clin Med (Lond). 2010;10(2):110-11.
- Royal College of Anaesthetists. Your anaesthetic and the environment. Available at: www.rcoa.ac.uk/patient-information/about-anaesthesia-perioperative-care/your-anaesthetic-environment.
