Developing surgical simulation models
By Ian Pallister
Consultant Orthopaedic Surgeon, Swansea Bay University Health Board and Professor of Trauma and Orthopaedic Surgery at Swansea University
Introduction
Simulation offers the opportunity to learn new skills in a stress-free environment, to test the application of those skills and decision-making capabilities in immersive scenarios, and also to identify potential gaps in systems and processes.
Simulation is not new. However, when applied with clear educational goals in mind, it remains a potent means of enriching knowledge and skills.
In this brief article, I shall outline the process of development used to create the Surgical Anatomy Models (SAMs). Generous and far-sighted support through the Defence and Security Accelerator (DASA) has been essential in the development of these models, tailored to military patterns of injury, but easily adaptable for civilian purposes.
Something is better than nothing
Simulation forms an essential part of training in a wide range of skills, from practice drills in sports to military exercises. Important though courses such as ATLS have been in cementing the role of simulation in trauma education, I was always frustrated that the scenario would end at the identification of the need to perform a surgical procedure.
Spurred on by this, I decided to identify a procedure which was time-critical, with which I was very familiar and would lend itself well to creating a simple model.
My first efforts fell into the category of 'kitchen sink' simulators, with simple lower limb fasciotomy models built around Synbones®, with muscle groups represented by condoms stuffed with cushion filler (Figure 1). The fascia was cling film and fat and skin a surrounding layer of thick orthopaedic felt. Although crude, these models enabled participants to move from recognising the need for a fasciotomy in a simulation scenario, to being able to execute one. It was self-evident that, although something was better than nothing, the crude nature of the models hindered immersion in the experience. The next step was to attempt to sculpt muscle groups and use commercial special effects silicones to cast the limbs. This was a distinct improvement, but still lacked realism. Casting from life appeared to be an obvious solution. However the external soft tissue envelope would not match the commercially available Synbones®, nor the sculpted muscles (Figure 2). A different approach was needed.

Figure 1: Original Fasciotomy Simulation Model.

Figure 2: Casting from life.
The Starting-Point
Working in a hospital with a very dynamic Maxillo-Facial Laboratory proved to be a godsend. A patient very kindly gave permission for their CT scan data to be used as a starting-point to create truly realistic fasciotomy models. Scans from the umbilicus to the tips of the toes were available, which included an angiogram phase.
Assisted by PDR in Cardiff Metropolitan University, this CT data was segmented and 3D virtual models of the patient’s bones, muscle groups, blood vessels and soft tissue envelope were created. These were then printed in 3D and moulds made (Figures 3 & 4).
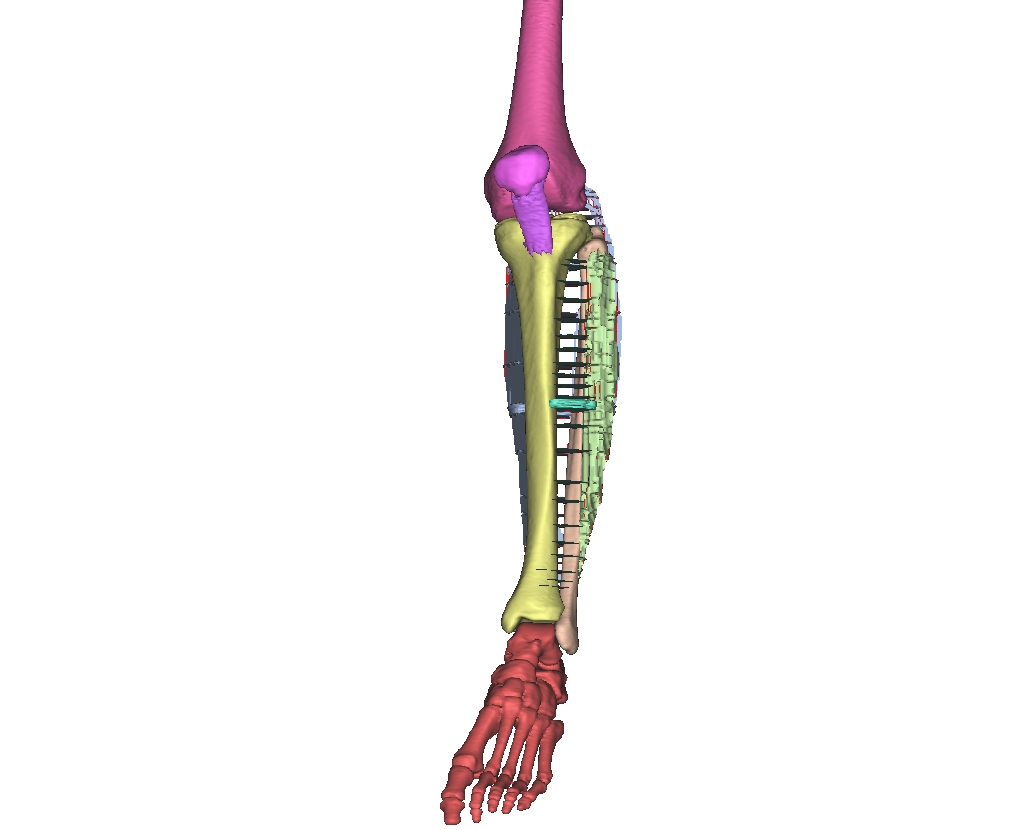
Figure 3: Initial data segmentation showing individual layers selected from CT images.
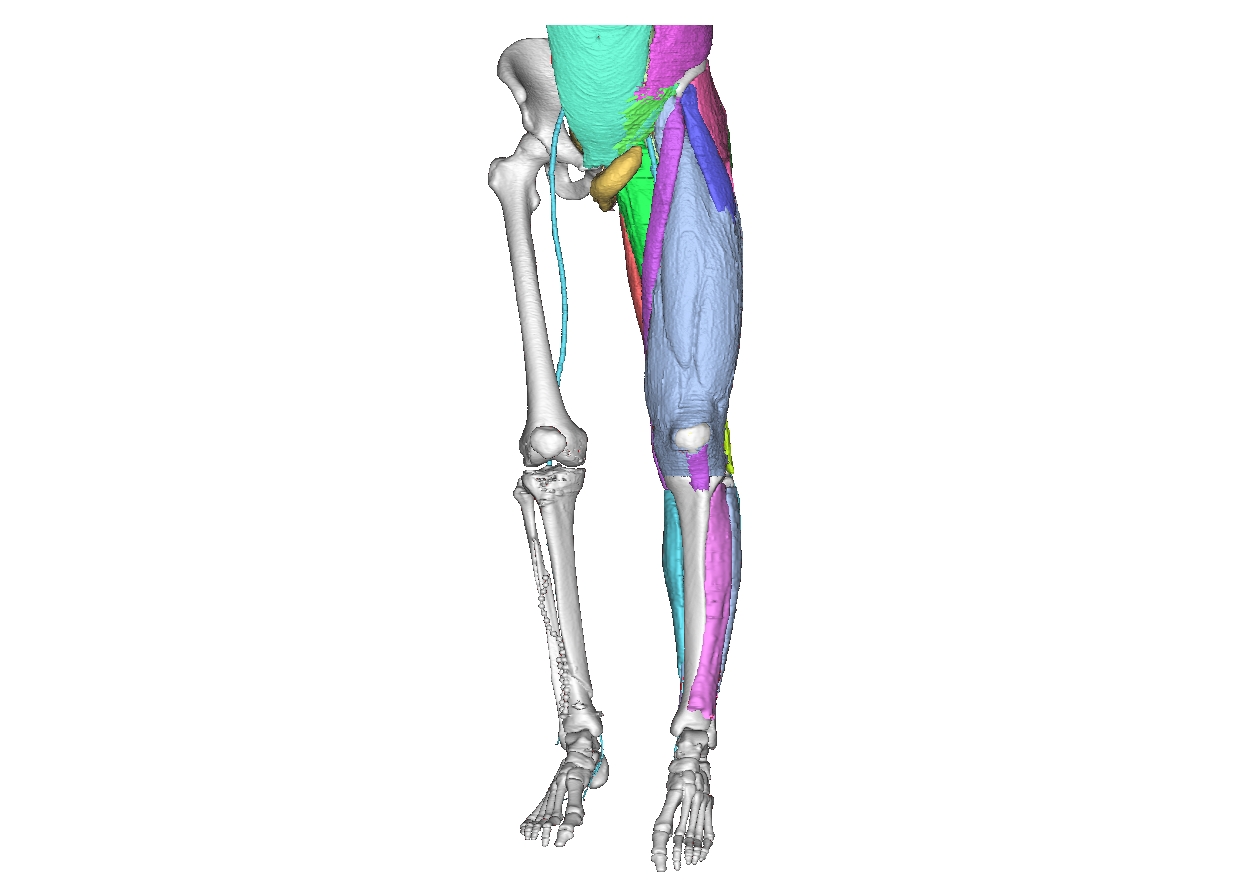
Figure 4: Anatomical 3D modelling.
Now we had the anatomical building blocks to create high-fidelity models for teaching fasciotomy in the lower limb. These models were a great improvement. However, surgery is a tactile art and some of the materials we were using did not faithfully reproduce the handling properties of, for example, subcutaneous fat.
Things took a great leap forwards in 2012 when DASA’s predecessor advertised a themed call for innovation in military combat casualty simulation. Having been completely unable to secure any meaningful development funding through civilian pathways, this was a vital lifeline.
The signature injury in the Afghan Conflict was inflicted by ground-level improvised explosive devices (IEDs). These devices would cause traumatic amputation of one or both lower limbs and cavitating pelvic injuries. The available CT data included the clinically relevant area. The terms of the call were applications should be made via a company rather than an academic institution, and so Trauma Simulation Ltd, a Swansea University spin-out company was formed and a bid made.
This was successful and we moved on to developing the first SAM model. Familiar though I am with pelvic trauma in the civilian setting, I needed the input of true subject matter experts in the this field. Fidelity in any model cannot be absolute. However it is crucial to identify the key steps in the execution of the simulated task. This process is known as task analysis. Alongside this, the handling properties of the simulator, whether aircraft or surgical model, are vital.
UK Defence personnel were (and still are) very engaged with this process and provided a wealth of guidance and feedback. The material properties of the simulated soft tissues improved dramatically with the involvement of MBI (Wales) Ltd in Bridgend, who also provided the physical location for the large-scale casting and assembly of the models. PDR contributed the know-how to design such large printed components which included the original moulds.
The models produced were 'one-off' pieces, which looked very good but were essentially single use. This made them prohibitively costly – especially as the model was so anatomically limited, so there was no scope for involvement of the wider team (Figure 5).

Figure 5: Simulated blast injury from IED
However, we had collectively developed the relationships to support task analysis far beyond my own area of specialisation, together with the technical capabilities for data segmentation, 3D printing of anatomical masters, moulds and material/handling properties. The stage was set for further development.
So far so good
The patient (now former patient) kindly agreed to return and MRI scans were performed to provide anatomical data for the production of a whole body model. After a series of further DASA contracts, SAM Mk VI is now in service with UK Defence1. The original 'one-off' model has evolved into a modular mannikin, into which a range of different anatomical inserts which contain different injury patterns can be placed (Figure 6).
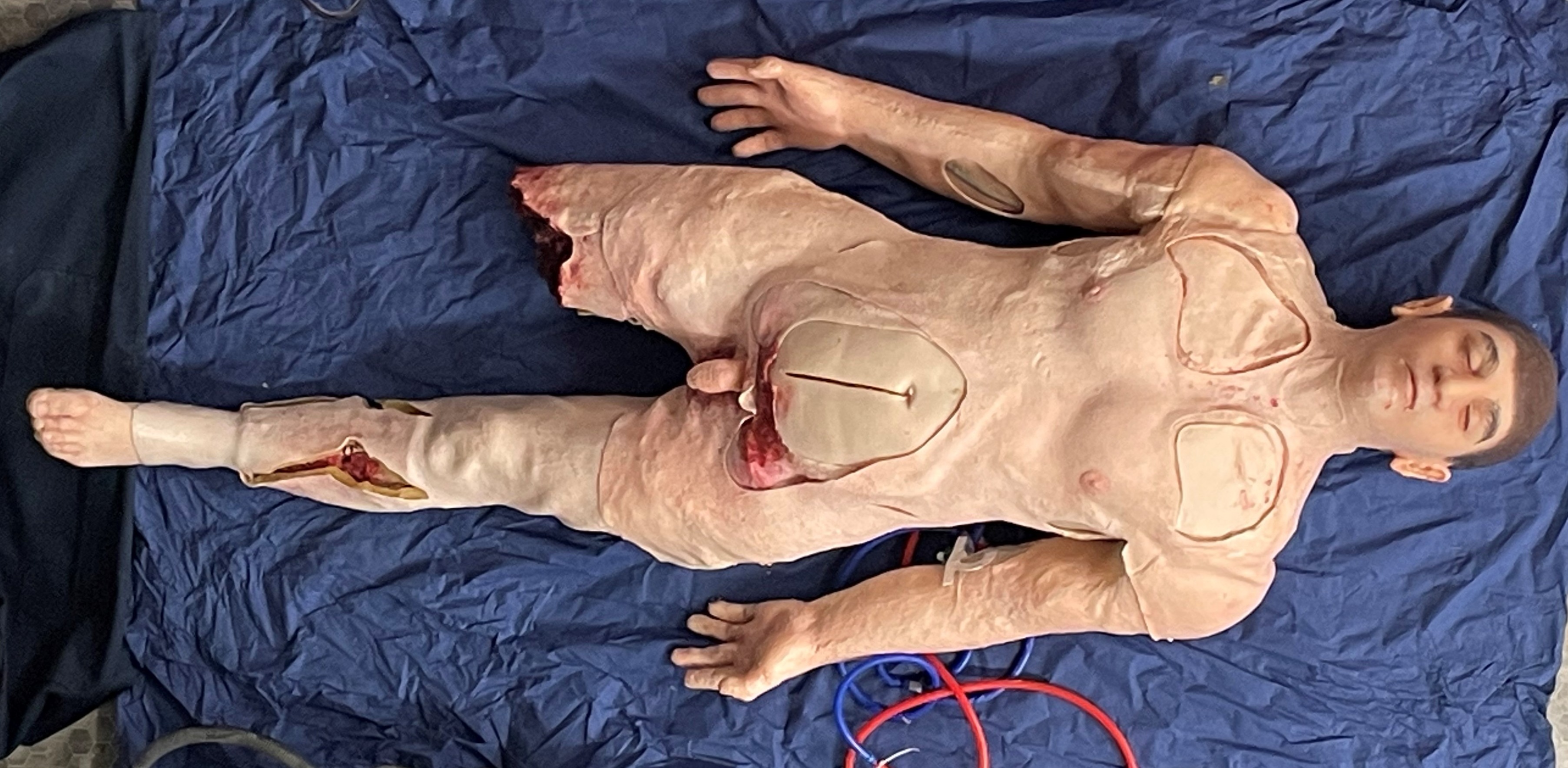
Figure 6: The modular mannikin.
Injuries to the junctional areas (e.g. the groin or shoulder) are a particular concern. Modern body armour is effective in protecting the trunk. More distal limb injuries can be temporised with the application of emergency tourniquets at the point of wounding. Haemorrhage from the junctional areas between the trunk and the limb can only be controlled by direct pressure or surgery. Hence the focus on these.
Here again, the guidance of military colleagues in the creating of the relevant anatomy in the junctional haemorrhage control inserts has been vital. Instead of attempting to make the whole body in its entirety, focus was turned onto these specific tasks and each area was developed separately as a task trainer, and then reverse engineered back into the whole body model.
Now the SAM Mk VI can arrive in 'ED' with the haemorrhage controlled with direct pressure, Cannulation (ante-cubital fossa or subclavian) can allow anaesthesia and once intubated surgery can go ahead (Figure 7). Once the bleeding from the injury to the common femoral artery has been controlled and the vessel shunted, the surgical team can then move on to fasciotomies of the lower leg. Major lower limb fractures or pelvic ring injuries can be simulated requiring emergency external fixation and in the case of the latter, pelvic packing.

Figure 7: SAM in action.
Following the draw-down from Afghanistan, Uk Defence have striven to minimise the effect of the Walker Dip in medical capabilities seen after the resolution of major conflicts2. The importance of this has been thrown into sharper focus in the light of current world events. All aspects of military service in the UK are now open to all genders. There is evidence that lack or representation hinders engagement in simulation, moreover data indicates higher mortality rates amongst female combat casualties than amongst males3,4. In the light of these considerations, we recently applied all of the lessons learnt in the development of a female model with extended capabilities.
The future
Task training and immersive simulation both have their place. Developments with virtual reality hold great promise for the future. Indeed for minimally invasive procedures, some of the systems appear very good. However, the real-world capabilities of such approaches do not presently allow for realistic instrument handling in open surgery. Nor do the systems allow for realistic immersive simulations for a whole team.
Continued development is the key to improved performance. With support from CitizenAID, the Vascular Surgery Society and the Blond-Macindoe Foundation we have developed point of wounding care models, an abdominal aortic aneurysm model and an upper limb escharotomy model5,6.
Simpler basic surgical skills simulation models are also being used in our local core trainee bootcamp.
Immersive simulation in the civilian setting allows all the steps in the chain of care to be replicated. This includes even the correct labelling and despatch of cross-match samples. While this is a seemingly simple task compared to surgical haemorrhage control, it is one of the few errors which may critically endanger a patient!
Declaration of Interest
Professor Ian Pallister is Founder and Director of Trauma Simulation Ltd, a Swansea University Spinout Company.
Acknowledgments
My friends and colleagues who have made this possible, my former patients who have allowed us to use their data and especially Surgeon Captain Adam Stannard RN, Lieutenant Colonel Rob Faulkoner, Chris Streets, Commanding Officer of the Institute of Naval Medicine Rtd, Maj. Gen Tim Hodgetts Rtd, Mark Midwinter Prof Clinical Anatomy, University of Queensland, Brisbane, Australia, Prof Mark Waters MBI (Wales Ltd) and Prof Dom Eggbeer PDR Cardiff Met University. Finally, DASA for being receptive to my ideas, James, Leigh and Jess for their artistry and craftsmanship, and my wife for tolerating endless prototyping.
References
- SSwain CS, Cohen HML, Stannard A, Faulconer ER, Pallister I. Bringing damage control surgery simulation to life: developing a novel surgical anatomy model within immersive military trauma surgery simulation. BMJ Mil Health. 2024;170(2):141-5.
- Walker AJ. The ‘walker dip’. Journal of The Royal Naval Medical Service. 2018;104:173-6.
- McGregor AJ. Sex Matters: How male-centric medicine endangers women's health and what we can do about it. Hachette UK; 2020.
- Cross JD, Johnson AE, Wenke JC, Bosse MJ, Ficke JR. Mortality in female war veterans of operations enduring freedom and Iraqi freedom. Clin Orthop Relat Res. 2011;469(7):1956-61.
- Gibson JAG, Gorse SH, Pallister I, Cubitt JJ. Surgical simulation training for escharotomy: A novel course, improving candidate's confidence in a time critical procedure. Burns. 2023;49(4):783-7.
- Hay-David AGC, Herron JBT, Thurgood A, Whittle C, Mahmood A, Bodger O, et al. A Comparison of Improvised and Commercially Available Point-of-Wounding Tourniquets in Simulated Traumatic Amputation with Catastrophic Hemorrhage. Mil Med. 2020;185(9-10):e1536-e1541.
