JTO - June 2020
Volume 8 Issue 2
From the Executive Editor
Strange and strained times. Writing an editorial that will be read a few weeks later is always risky business but even more so when surrounded by such volatility. It is, however, the essence of so much of what we do; we make the best judgement we can in the circumstances that prevail and proceed. Whether those circumstances be a tricky problem in theatre or the fallout from a pandemic we carry on. This special edition of the JTO charts some of our efforts.
The normal printed JTO had been cancelled but then an opportunity arose to partially resurrect it as special on-line PDF version. To keep up with the ever changing world of COVID-19 we had already started publishing articles in a rapid turn-around Journal called the TJTO&C or the Transient Journal of Trauma Orthopaedics and the Coronavirus. This PDF version of JTO is in the main a compilation of those articles, with some updates and commentaries.
The swing in the pervading mood over the last eight weeks has been extraordinary; an acute fear of being overwhelmed by pandemic respiratory failure morphing into a pervasive threat of endemic Coronavirus. The articles we have chosen reflect this mood swing. Some document the redeployment and experiences of individuals in the acute phase. ‘An orthopaedic surgeon’s diary at the Nightingale Critical Care Unit’ page 18 will be read in the future in a way similar to how I heard my parents describe the Blitz. A personal story of ‘Coronavirus (COVID-19): My experience of testing positive’ page 16 will hopefully soon seem like a relic of a bygone age. They are a record of what happened, a Pepys diary of 2020.
There are more philosophical issues that arose. The article that promoted the most debate was that detailing SHiFT, a potential response to the anticipated collapse in resources which threatened. What would be the consequences of this on managing our normal urgencies, the exemplar for T&O being the hip fracture. It confronts triage of a condition with a risk of mortality, which for most of us has only ever been role play. We did it on our ATLS course but there was now the prospect of it happening for real. The Armageddon that was feared did not materialise but chronicling the planning exercise is of value.
The acute loss of resource may now be replaced by a chronic one. With a morass of unpredictability awaiting; slower operating, fewer beds, PPE, staff testing, patient testing, consent, residual fear, the list could go on. This continues to generate noise in the unending health dilemma of whether we need central diktat or local solutions; one with its inflexibility the other risking a postcode lottery.
A full retrospective can be had in a future bumper edition of JTO or a component of a Congress, but we have no idea when. Until then the TJTO&C will provide a forum.
It is now customary to sign off with the invitation or encouragement to keep safe, the inference often being to hunker down to stay alive. I like the adage that “Life is movement and movement is life.” I don’t think that this was intended to apply only to the muscles used in breathing. In T&O our most common objective is restoration of function, this should now be the objective for both society and the individual. Phase one of COVID-19 could be summed up as “Be safe, don’t do anything” now we need “Do something but safely!”
Those could just be hollow words but what better example could we have of the benefits of restoring function than Sir Tom. The raw statistics don’t look that good for a man in his late 90s with a hip fracture, but a broad smile and £33 million for the NHS is quite a result. We salute you Sir!
Bob Handley, Vice President Elect
References
Non-accidental injury in children in the time of COVID-19 pandemic
- United Nations Children’s Fund, Hidden in Plain Sight: A statistical analysis of violence against children, UNICEF, New York, September 2014. Available at: https://www.unicef.org/publications/index_74865.html.
- Caffey J. Multiple fractures in the long bones of infants suffering from chronic subdural haematoma. Am J Roentgenol Radium Ther. 1946;56(2):163-73.
- Cook Children's Newsroom (2020). Available at: https://www.checkupnewsroom.com/spike-in-severe-child-abuse-cases-likely-result-of-covid-19.
- Huang MI, O’Riordan MA, Fitzenrider BA, McDavid L, Cohen AR, Robinson S. Increased incidence of nonaccidental head trauma in infants associated with the economic recession. J Neurosurg Pediatr. 2011;8(2):171-6.
- Belfer RA, Klein BL, Orr L. Use of skeletal surveys in the evaluation of child maltreatment. Am J Emerg Med. 2001;19(2):122-4.
- Worlock P, Stower M, Barbor P. Patterns of fractures in accidental and non-accidental injury in children: a comparative study. Br Med J (Clin Res Ed). 1986;293(6539):100-2.
- Kemp AM, Dunstan F, Harrison S, Morris S, Mann M, Rolfe K, Datta S, Thomas DP, Sibert JR, Maguire S. Patterns of skeletal fractures in child abuse: systematic review. BMJ. 2008;377:a1518.
COVID-19 causes a SHiFT in the sands for proximal femoral fracture management?
- Lindley DV. (2006). Understanding Uncertainty. Hoboken: John Wiley & Sons.
- British Orthopaedic Association (2020). Emergency BOAST: Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html.
- Public Health England (2020). Reducing the risk of transmission of COVID-19 in the hospital setting. Available at: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/reducing-the-risk-of-transmission-of-covid-19-in-the-hospital-setting.
- Dr Foster Intelligence (2012). Hospital guide 2012. Available at: http://download.drfosterintelligence.co.uk/Hospital_Guide_2012.pdf.
- Wiles MD, Moran CG, Sahota O, Moppett IK. Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br J Anaesth. 2011;106(4):501-4.
- Johansen A. Talking about ceilings of treatment when clerking older trauma patients. The Transient Journal of Trauma, Orthopaedics and the Coronavirus. April 2020. Available at: https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/talking-about-ceilings-of-treatment-when-clerking.html.
- Hip Fracture Database. National Hip Fracture Database National Report 2013. London: Royal College of Physicians; 2013.
- Moulton LS, Green NL, Sudahar T, Makwana NK, Whittaker JP. Outcome after conservatively managed intracapsular fractures of the femoral neck. Ann R Coll Surg Engl. 2015;97(4):279–82.
- Gregory JJ, Kostakopoulou K, Cool WP, Ford DJ. One-year outcome for elderly patients with displaced intracapsular fractures of the femoral neck managed non-operatively. Injury. 2010;41(12):1273-6.
- Handoll HH, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst Rev. 2008;(3):CD000337.
- Institute of Medicine (IOM). 2007. Ethical and Legal Considerations in Mitigating Pandemic Disease, Workshop Summary. Chapter 4: Ethical Issues in Pandemic Planning and Response. Washington, DC: The National Academies Press.;2007.
A letter in response to: COVID-19 causes a SHiFT in the sands for proximal femoral fracture management? A plea for caution
- Cronin M, Mullins M, Pathmanaban P, Williams P, Dodd M. COVID-19 causes a SHiFT in the sands for proximal femoral fracture management? The Transient Journal of Trauma, Orthopaedics and the Coronavirus. 14 April 2020. Available at: https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/covid-19-causes-a-shift-in-the-sands-for-proximal.html.
- Anna Lewis. NHS issues warning as people 'wait too long' to seek emergency treatment for non-coronavirus issues. Wales on line, 16 April 2020. Available at: https://www.walesonline.co.uk/news/health/emergency-treatment-wales-nhs-warning-18101189.
- Lewis PM, Waddell JP. When is the ideal time to operate on a patient with a fracture of the hip? Bone Joint J. 2016;98-B(12):1573-81.
- British Orthopaedic Association (2020). Emergency BOAST: Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html.
- Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101(4):511-7.
- Handoll HHJ, Parker MJ. Conservative versus operative treatment for hip fractures. (Review). Cochrane Database Syst Rev.2008;(3):CD000337.
- Hornby R, Evans JG, Vardon, V. Operative or conservative treatment for trochanteric fractures of the femur. A randomized epidemiological trial in elderly patients. J Bone Joint Surg Br. 1989;71(4):619-23.
- Moulton LS, Gree NL, Sudahar T, Makwana NK, Whittaker JP. Outcome after conservatively managed intracapsular fractures of the femoral neck. Ann R Coll Surg Engl. 2015;97(4):279-82.
- Gregory JJ, Kostakopoulou K, Cool WP, Ford DJ. One-year outcome for elderly patients with displaced intracapsular fractures of the femoral neck managed non-operatively. Injury. 2010;41(12):1273-6.
- Surgical Royal Colleges of the UK and Ireland (2020). Guidance for surgeons working during the COVID-19 pandemic. Available at: https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v1/.
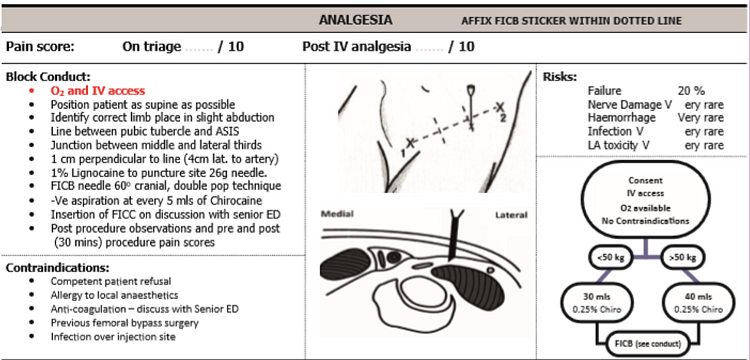
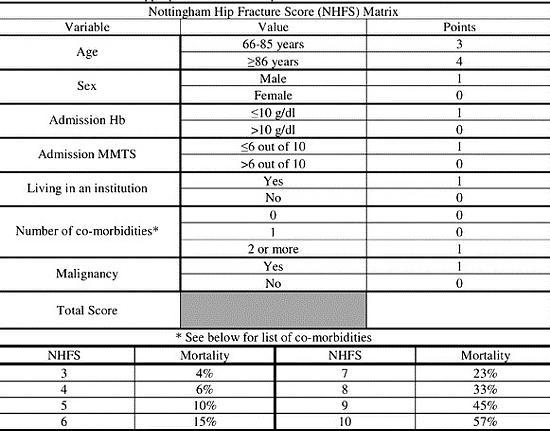
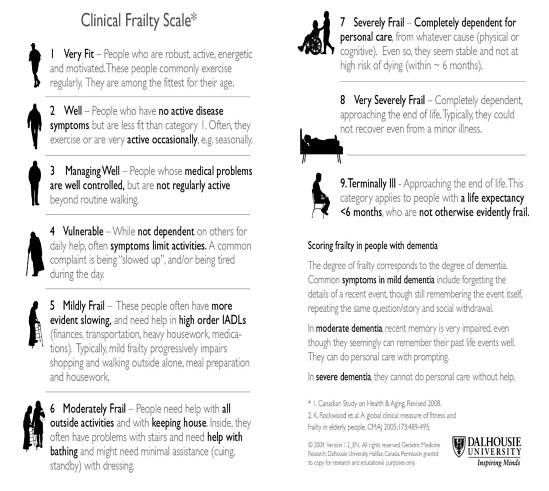
Appendices
COVID-19 causes a SHiFT in the sands for proximal femoral fracture management?
Appendix 1: Nottingham Hip Fracture Score
Appendix 2: Clinical Frailty Scale
Appendix 3: Analgesia ladder + Femoral nerve block criteria