Learning from UK orthopaedic cases
Author: Heidi Mounsey
Download PDFOrthopaedic surgery is a specialty dealing with a wide range of musculoskeletal conditions. Serious complications following surgery are rare, but medico-legal cases may arise due to the life-changing impact they can have on mobility and function.
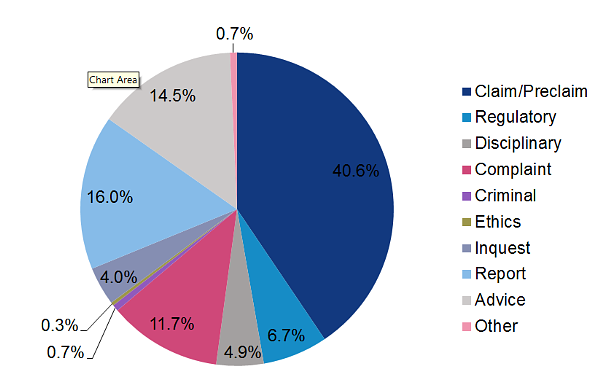
Medical Protection analysed more than 1,800 cases including claims, pre-claims complaints, General Medical Council investigations, local disciplinary procedures and inquests. The value of our highest case payment was over £3.6 million.
Claims
The below are the most common types of procedures leading to a claim:
- Knee surgery: including total knee replacement, knee arthroscopy, and anterior cruciate ligament reconstruction. Common themes included failure to offer conservative management or to explain the limitations of the proposed procedure. The highest payment was over £550,000.
- Hip surgery: the majority of claims were brought in relation to elective hip replacements and revision surgery. Common factors included selection of the wrong sized components, malposition of components and failure to perform or correctly interpret postoperative x-rays. Alleged negligent outcomes included leg length discrepancy, restriction of mobility, nerve damage, infection or dislocation. Many patients who claimed required correction surgery. The highest payment was over £300,000.
- Metal on metal hips: in some cases a product liability claim was brought against the manufacturer. Allegations directed at Medical Protection members included ‘mixing and matching’ of components. This sometimes led to increased metallosis or accumulation of metal debris in soft tissues. Contributing factors included failing to review patients, failure to monitor metal levels in the blood, failure to perform imaging and failure to offer revision surgery.
- Spinal surgery: claims often related to lumbar nerve root decompression or spinal fusion. Common factors included incorrect choice of procedure and allegations of poor surgical technique or misplacement of metalwork. Consequences included pain and weakness, development of bladder and bowel incontinence. The highest payment was over £3.6 million.
- Hand surgery: in particular, procedures such as trigger finger release, Dupuytren’s contracture release, ganglion excision and carpal tunnel surgery when performed in a ‘one-stop’ setting. Common factors included failure to discuss the options and assuming that conservative management had been offered or trialled by the GP. Allegations were made in relation to poor surgical technique resulting in consequences such as nerve injury, leading to loss of function of the hand.
- Foot surgery: complications arising from hallux valgus correction surgery, including tendon and nerve damage resulting in complex regional pain syndrome and abnormal gait. Common factors included the risks of chronic pain and/or neuropathic pain not being discussed prior to surgery.
- Fractures: missed fractures around total hip prostheses. Common themes included not adequately examining the patient or arranging further imaging; and inadequate assessment.
Regulatory (GMC) and disciplinary investigations
GMC cases have followed referral from patients, relatives or colleagues. The common themes were:
• Allegations of poor surgical competence, including higher than expected complication rates, poor functional outcomes, or lack of experience for the operations performed.
• Patients’ or colleagues’ dissatisfaction with the manner or attitude of the surgeon.
• Inadequate communication when surgery was delayed or cancelled.
• Bullying, harassment or assault of colleagues.
• Failure to supervise junior staff in theatre.
• Poor postoperative management of complications.
• Allegations of theft of equipment from the hospital.
• Failure to attend when requested while on-call.
• Performing private work during NHS time or using NHS resources to do so.
• Alcohol and drug misuse.
• Probity issues, including fraudulent use of codes when billing in private practice or authorship of publications.
• Criminal convictions arising from personal life.
• Use of experimental joint replacement prostheses without adequate informed consent or governance.
Inquests
The purpose of an inquest is to find out who died, when, where, how and in what circumstances. We identified the following themes:
• Postoperative deaths due to pulmonary embolism – in some cases where postoperative prophylactic anticoagulation
had not been provided or had been stopped due to bleeding from the surgical incision.
• Other complications including sepsis, bowel ischaemia or obstruction and haemorrhage.
Complaints
Similar themes to those outlined above were seen, but also included:
• Inaccurate completion of medico-legal reports, for example in relation to personal injury compensation claims.
• Development of pressure sores postoperatively.
• Inappropriate examination of patients.
• Dismissive attitude during consultations.
• Delay in organising further care such as physiotherapy.
• Failure to inform patients of investigation results.
Top tips to minimise risk
This is not an exhaustive list of recommendations, but some key learning points.
• Ensure your surgical technique is regularly updated and in line with current best practice such that it would be supported by your peers.
• Discuss the possible benefits and risks of all potential surgical or conservative treatment options. Consider what is most important to that individual.
• Listen to what your patient would consider to be a successful outcome. Understand concerns and expectations.
• Explain complications, including the possibility of chronic pain. Explain what can be done to manage complications. Document these discussions.
• Never pressurise patients into giving consent to have surgery.
• For elective operations always leave sufficient time after the consultation before scheduling the procedure.
• Remember consent is a process and not simply a signature on a form.
• Do not assume that another practitioner has held an informed discussion with the patient about all the available options.
• Give patients clear information about all costs involved and what their rights are to refunds/return of deposits.
• Double-check that the information has been understood and decisions are informed.
• Ensure a perioperative management plan is in place, including assessment of venous thromboembolism risk.
• At discharge, review the requirement for ongoing anticoagulant.
• Ensure any postoperative deterioration, complication or falls are communicated, investigated and managed.
• Consider the Medicines and Healthcare products Regulatory Agency guidance when providing follow up of patients with metal on metal hip replacements: www.gov.uk/drug-device-alerts/all-metal-on-metal-mom-hip-replacements-updated-advice-for-follow-up-of-patients.
• Demonstrate empathy in your consultations.
• Remember that accurate and clear documentation is the cornerstone of any medico-legal defence.
• Ensure you are fully indemnified to carry out the relevant procedure in the UK.
Additional resources
• Medical Protection workshops and masterclasses: www.medicalprotection.org/uk/hub/workshops-masterclasses.• Getting It Right First Time (GIRFT) report on spinal services: https://gettingitrightfirsttime.co.uk/surgicalspecialty/spinal-surgery.
• British Association of Spinal Surgeons (BASS) guidance on consent: https://spinesurgeons.ac.uk/patient-area/consent.
• Royal College of Surgeons of England standards and research: www.rcseng.ac.uk/standards-and-research/standards-and-guidance.
