Major Conditions Strategy – interim report
The Department of Health and Social Care has published the interim report of the work to date to develop a Major Conditions Strategy. The Strategy, announced in January, will seek to tackle the six major conditions that contribute to the burden of disease in England, including musculoskeletal disorders.
Building on the NHS Long Term Plan, this is another attempt in a long history of such policy initiatives to reduce the burden of disease on the health system, increase healthy life expectancy and ‘reduce ill-health related labour market inactivity’.
The Strategy will support the Conservative Party manifesto commitment of gaining five extra years of Healthy Life Expectancy by 2035, and the Government’s levelling up mission to narrow the gap in Healthy Life Expectancy by 2030.
The Strategy will seek to tackle the major conditions which contribute to the burden of disease in England, namely:
- Cancers
- Cardiovascular diseases, including stroke and diabetes
- Chronic respiratory diseases
- Dementia
- Mental ill health
- Musculoskeletal disorders (MSK)
Proportional contribution of major health conditions to the total DALY burden in England (Source: Global Burden of Disease, 2019)
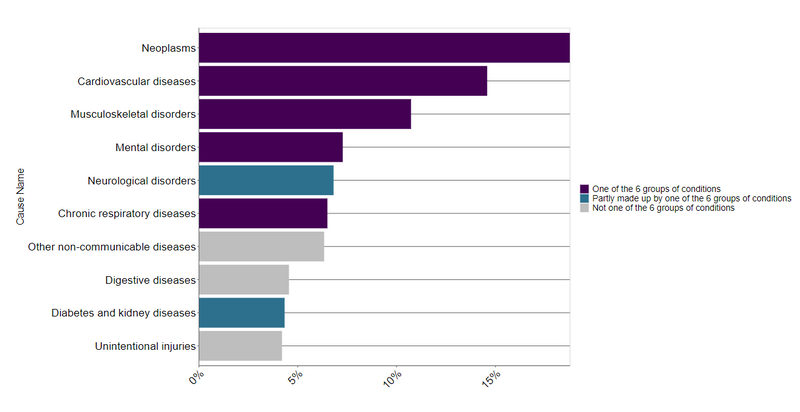
These areas account for around 60% of total Disability Adjusted Life Years in England.
Poor MSK health is the leading contributor to the global burden of disease, with 20 million people in the UK living with an MSK condition (see the State of musculoskeletal health). In addition, one in 8 report living with at least 2 long-term conditions, one of which is MSK related. MSK conditions are one of the leading causes of years lived with disability in the UK today, accounting for 21% of years lived with a disability (YLDs), with low back pain the top cause (see the State of musculoskeletal health). They are also one of the main reasons given for ill health inactivity, with 21% of those economically inactive reporting MSK conditions.
MSK conditions affect people across the life course and cover a range of conditions, including conditions of MSK pain such as osteoarthritis, back pain and fibromyalgia, osteoporosis and inflammatory conditions such as rheumatoid arthritis and spondylarthritis.
Prevention, early detection and treatment can enable people to live in good health, remain independent and connected to the community, reduce the pressure on health and social care services and support people with MSK conditions to thrive in work.
The report identifies that there is opportunity for significant improvement in both the prevention of MSK conditions and outcomes for people living with an MSK through physical activity, encouraging maintaining a healthy weight and balanced diet, education on MSK health and conditions, improved mental health, smoking cessation and alcohol moderation.
The report notes that many conditions of MSK pain have gradual onset and progression, meaning there is good opportunity for early identification and secondary prevention. Evidence shows that early identification, interventions in secondary prevention, long-term care and self-management, alongside timely referrals where necessary and utilising shared decision-making improve patient outcomes and can show positive return on investment. The interim report acknowledges that existing secondary fracture prevention initiatives, namely fracture liaison services, could present a viable and effective route to improving health outcomes and reducing years lost to disability for those at risk of osteoporotic fracture. The BOA is supporting the Royal Osteoporosis Society campaign with the Sunday Express for universal access to fracture liaison services.
The Spring Budget 2023 announced a package of measures to support individuals at risk or experiencing MSK conditions to live and work well, including:
- Integrating employment advisors into MSK pathways to help individuals with conditions return to or remain in work.
- Making best use of digital health technologies to support people with MSK conditions to better manage symptoms and remain in the workforce. This includes providing free access to digital therapeutics for MSK problems via the NHS App and other national digital channels.
- Designing and scaling up of MSK community hubs aligned with integrated neighbourhood teams to expand access to community based physical activity interventions, including access to vocational support, helping people with MSK conditions remain in or return to work.
- Exploring how best to support MSK primary and community service improvement and leadership, including improving collection of data, helping to give MSK greater parity with other conditions.
As part of the ongoing work to support and address MSK conditions, the government and NHS will:
- Improve secondary prevention and the use of non-pharmaceutical interventions, embedding a biopsychosocial and personalised approach and building upon the progress made through the NHS Long Term Plan, such as the integration of first contact practitioners, health coaches and social prescribers in primary care and the resources developed through the Best MSK Health Pathway Improvement Programme.
- Advocate the use of population health management methodologies to target the right kind of support based on individual circumstances and need to those who need it most, enabled by increased integration of care pathways and collaborative working across local health care services as well as social services and voluntary, community and social enterprises.
- Aim to improve services where medical treatment is necessary, including to ‘explore supporting the provision of fracture liaison services. This could include identifying people at risk of further osteoporotic fragility fracture and implementing strategies to reduce risk of future fracture (including falls) and mortality’.
Link to full interim report here.
