Non-technical skills & orthopaedic surgery: Beyond the eyes of a hawk, heart of a lion and hands of a lady
By Kalpesh Vaghela
| Winner of 2022 Robert Jones Gold Medal and Association Prize |
Introduction
“Don’t forget! To be a successful surgeon, you must have the eyes of a hawk, the heart of a lion and the hands of a lady.” Sir Lancelot Spratt, Doctor in the House 19541,2. Sir Lancelot Spratt’s description of a successful surgeon in the classic comedy Doctor in the House is of someone who possesses great knowledge and one who is technically gifted but one who lacks tacit, non-technical skills. As medicine has progressed into the 21st century there is a growing and compelling body of evidence to suggest that non-technical skills are critical in patient safety and surgical outcomes3. Root cause analysis of adverse events in surgery reveal that many underlying causes are behavioural, such as a lack of leadership or failure of communication rather than technical error4. These non-technical skills are currently not explicitly addressed in surgical training however, there is consensus amongst the surgical faculty that’s these skills are important and require dedicated teaching.
The term non-technical skills encompass a number of tacit or 'soft skills' which include situation awareness, team working, leadership, communication, managing stress, coping with fatigue and decision making (Figure 1). Non-technical skills can be further defined as the “cognitive, social and personal resource skills that complement technical skills, and contribute to safe and efficient task performance”5. Non-technical skills are also part of the human factors agenda. Catchpole defined human factors as “enhancing clinical performance through an understanding of the effects of teamwork, tasks, equipment, workspace, culture, organisation on human behaviour and abilities, and application of that knowledge in clinical settings”6. The terms non-technical skills, human factors and crisis resource management are interchangeable and relate to the same concepts.
This essay is structured to describe the importance of non-technical skills in surgical error and to explore its historical origins. It will then go on to review the development of non technical skills within the wider context of surgery and medicine. Finally, the essay will outline the progress made in orthopaedic surgery and summarise the leading research into the field.
Error in Medicine
A deficiency in non-technical skills rather than failures in technical proficiency has been linked to adverse outcomes in surgery. The Institute of Medicine published the report To Err is Human in 1999 which reported that 44,000 to 98,000 people die each year in US hospitals due to preventable medical errors8. James Reason’s seminal work on latent errors in medicine found that several small errors can be prevented by protective mechanisms however when these barriers are passed a major critical incident occurs9. He developed the 'Swiss-Cheese' model where accidents are caused by a sequence of flaws that are caused by operational staff (active failures) and latent unsafe conditions (resident pathogens). Reason argues that while human error is pervasive and inevitable, humans are resilient and have expertise which can be protective in an imperfect and threatening environment10.
Ken Catchpole et al. observed that some of these latent errors were due to failures of nontechnical skills. He found that errors in surgical technique had a strong association with situation awareness while other errors were related to the leadership and management skills of nurses11,12. Prof Charles Vincent found that non-technical skills can impact technical performance in surgery however, the precise extent of the effect remains to be elucidated13. Atul Gwande et al. analysed surgical critical incident reports from three hospitals and found that a breakdown in communication contributed to 43% of incidents with surgical team fatigue and stress contributing to 33% of incidents14.
A Historical Perspective
The concept of non-technical skills and crew resource management was borne in the aviation industry in the late 70s by the National Aeronautical and Space Agency (NASA). Failures in non-technical skills were implicated in many air crashes. Psychologist John Lauber studied communication in the cockpit. Whilst maintaining an overall hierarchy, co-pilots were encouraged to speak up and challenge their captains if errors were being made15,16. The delivery of non-technical skills training evolved from simple workshops to high fidelity full mission simulations with the aim of improving critical incident reporting and create a safety culture in aviation. The concept of crew resource management evolved into crisis resource management (CRM) and was adopted by several other high stakes industries such as nuclear power and medicine17.
Non-technical Skills in Medicine and Surgery
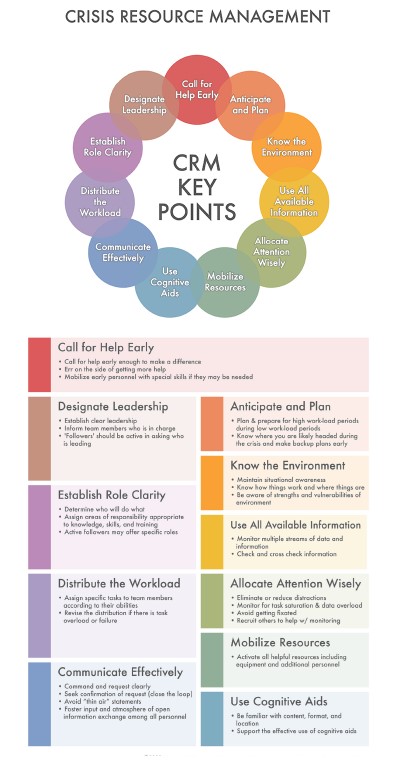
The medical professional quickly adopted CRM into their curricula, starting with the anaesthetists. David Gaba an anaesthetist at Stanford School of Medicine developed an Anaesthesia CRM course consisting of didactic lectures containing videos of anaesthetic 'mishaps' and then a two-hour intensive simulation session followed by de-briefing. The authors conclude that a mixed method course was effective at training anaesthetists about CRM where it was previously taught haphazardly18,19. They distilled the main points of CRM into a 15-point outline which is used extensively in the literature and forms the keystone of modern training in many medical and allied health care professional curricula including emergency medicine20, trauma teams21, scrub nurses22–25 and nursing.
Non-technical skills and CRM is also critical in successful surgical outcomes. Neily et al. conducted a study comparing the 1-year mortality of 108 Veterans Health Administration (VHA) hospitals who underwent a medical team training programme to a contemptuous control group. They found 18% reduction in annual mortality compared with a 7% decrease in the control group. Furthermore, a dose-response relationship for further training sessions was demonstrated with a reduction of 0.5 deaths per 1000 procedures occurred for every additional quarterly session27,28.
The Royal College of Surgeons of Edinburgh (RCS Ed) have pioneered non-technical skills training and research within the surgical context. The RCS Ed run the Non-Technical Skills for Surgeons (NOTSS) Masterclass which is an intensive one day simulation based course facilitated by a multi-disciplinary team of surgeons, anaesthetists and psychologists. The RCS Ed also facilitate the NOTSS in a Box e-learning resource which comprises of interactive online modules.
Steven Yule developed a behaviour rating system called the NOTSS assessment tool4. This allowed for objective assessment of non-technical skills and CRM points and therefore facilitated feedback. The NOTSS tool has been shown to be both a reliable and valid assessment tool29–31. Ken Catchpoles Oxford group went on to develop assessment tools evaluating the whole surgical team in a holistic approach. The Oxford Non-Technical Skills Scale (Oxford-NOTECHS I & II) has been used to assess team working in the operating theatre32,33. Observational Teamwork Assessment Tool (OTAS) comprises of a procedural task checklist centred on the patient, equipment and communication tasks and team behaviour constructs including cooperation and leadership34. This tool has been validated and translated worldwide taking into account local cultural practices35,36. A criticism of the current surgical non-technical skills assessment tools is that they are observer dependent which can affect reliability. In addition, most of the validation studies have been limited to the general surgical context. Three extensive systematic reviews of non-technical skills in surgery have produced mixed results. Wood et al found that the NOTSS and the NOTECHS tools were the gold standard in individual and team based non-technical skills assessment(37). Another review found high satisfaction ratings from surgical trainees with significant improvements in performance which did not decay over time. Oral feedback was found to be as effective as video feedback and single day courses were comparable to multiple day interventions38. Dedy et al. went on to review the effectiveness of training and assessment. The overall strength of evidence was rated as moderate for teamwork, low for patient centred communication and decision making, and very low for patient safety39. The literature is focused on qualitative methods to ascertain whether an assessment tool can differentiate between different levels of expertise (construct validation) or whether the tool is reliable.
Non-technical Skills in Orthopaedic Surgery
To the rest of the medical profession the non-technical skills and the orthopaedic surgeon is somewhat of an oxymoron. The long held belief that the orthopaedic surgeon is a “man of enormous build and great strength, if perhaps a little slow” is still perceived even today40,41. Some authors have attempted to dispel these myths. In the 2011 Christmas British Medical Journal Subramanian et al. found that orthopaedic surgeons had significantly higher IQ scores and grip strength than their anaesthetic colleagues42.
Whilst there has been significant development in non-technical skills within the context of anaesthetics and general surgery, rather less is known about its relevance in trauma and orthopaedic surgery. Trauma and orthopaedic surgeons face a unique set of challenges in the operating theatre through interaction with multiple team members. These include x-ray radiographers, scrub nurses and industry representatives who assist the surgeon. To address this imbalance, in 2013 the Department of Trauma and Orthopaedics at the Royal London Hospital combined forces with the Education Academy at Barts Health NHS Trust and developed a one-day novel, non-technical skills course specifically catered for orthopaedic surgeons43. The course begins with an overview didactic lecture about non-technical skills and participants complete a consent form which reassures them that the events in the scenarios are confidential and are designed to enhance learning rather than humiliate. They also complete pre-course questionnaires exploring their experience of non-technical skills to date. The course was attended by junior orthopaedic trainees, orthopaedic registrars as well as allied health care professionals such as scrub nurses and health care assistants thus promoting interprofessional learning.
Orthopaedic critical incident reports from the Royal London Hospital underwent inductive thematic analysis producing recurrent themes which were used to develop six scenarios that explore the 15 CRM points. These include: two clinic (angry patient and baby hip ultrasound clinic), two ward (inappropriate consultant behaviour and haemorrhage vs pulmonary embolism) and two theatre based (hemiarthroplasty cement reaction and equipment failure) scenarios43. A team of educationalists created discrete learning objectives for each scenario and mapped them to the orthopaedic curriculum. The course faculty consisted of orthopaedic consultants, anaesthetists, operating department practitioners and scrub nurses each with their own unique perspective and experience of non-technical skills.
Each scenario was observed through a two-way mirror system by the faculty and by other course participants in the debriefing room (Figure 4). This enabled the faculty to collate feedback points and the other participants to observe the behaviours and unique challenges of each scenario. All scenarios were also recorded using a high definition audio-visual system which allowed for video clips to be played back to the course participants if there was a specific CRM point being demonstrated. Upon completion of each scenario the participants were debriefed by appropriately trained faculty members. The course has now been run six times. In a study examining feedback from 26 orthopaedic registrars Heaton et al. found that they had a poor understanding of non-technical skills and their role in patient safety which improved after the course (Likert 3.0 to 4.2). They also found that the course provided an unthreatening learning environment and reported high levels of face validity of the scenarios43.


Vaghela et al. used the RCS NOTSS tool to assess the orthopaedic trainees and found that the scenarios could differentiate between differing levels of experience. Furthermore, there was high levels of inter-rater reliability between the multidisciplinary assessors including orthopaedic consultants, anaesthetists and scrub nurses who were trained in using the NOTSS tool. In the post course feedback analysis 100% of the orthopaedic registrars rated the multidisciplinary approach to learning non-technical skills as ‘very beneficial’. 85% of Orthopaedic registrars rated the scenarios as being ‘very realistic’. The structured de-briefing post-scenario sessions were rated ‘very useful’ by 92%. The allied healthcare professionals found that the course enhanced team working with the orthopaedic surgeons44.
The interest in bespoke non-technical skills courses for orthopaedic surgeons is gaining traction with other centres across the country developing simulation courses and presenting their results in conferences such as the British Orthopaedic Association Annual Congress 2017. The Torbay simulation centre have developed a simulation course for orthopaedic surgeons and used the NOTSS tool and an Objective Structured Clinical Examination (OSCE) marking scheme to assess the participants. They found that overall performance in nontechnical skills was below an acceptable standard. Analysis of clinical performance showed there was an unmet training need for non-technical skills and analytical thinking during emergencies45. The evidence presented suggests that non-technical skills training is often not delivered by traditional didactic or lecture based teaching but rather an amalgam of the apprenticeship model and simulation based learning.
The utility of simulation has also been demonstrated outside the confines of a simulation theatre. In-situ simulation is where the scenario is transported into a live clinical setting which has the benefit of adding realism and the opportunity for the team to practice actual emergency mechanisms within a hospital. Steinemann et al. demonstrated an improvement in teamwork and clinical performance in trauma teams in both simulated and actual trauma settings after completion of an in-situ simulation programme46. High fidelity manikins such as SimMan 3G also have the portability to be used out in the field and can be used during military trauma training in simulated combat zones47 Figure 5.

Perceptions of Orthopaedic Surgeons of Non-Technical skills
It is currently unclear from the literature how orthopaedic surgeons learn about non-technical skills apart from a few centres offering dedicated simulation-based training. To investigate this very question Vaghela el al conducted a qualitative study looking at the perceptions of orthopaedic trainees of non-technical skills training and reviewed the educational theory behind how trainees learn these tacit skills48.
They recruited two cohort’s orthopaedic trainees from the North-East Thames region of London. Cohort one were orthopaedic trainees who had undergone the dedicated Royal London immersive simulation course in non-technical skills and cohort two were trainees who had conventional training only. Semi-structured interviews were used to explore trainees’ perceptions of non-technical skills training. Audio recordings were transcribed verbatim and underwent Braun and Clarke’s inductive thematic analysis using NVIVO qualitative software49.
Ten semi-structured interviews were completed which included eight males and two female trainees. Orthopaedic trainees with a wide range of experience from first year orthopaedic trainees to fellows were interviewed. Seven interviews were completed for cohort one with 216 minutes of interview time; producing 39,903 words of transcription. Three interviews were completed for cohort two with 45 minutes of interview; producing 7,700 words of transcription. Thematic analysis revealed seven overarching themes (Figure 5).
In this seminal study, the orthopaedic trainees were found to have a good overall understanding of the concept of non-technical skills and their importance in positive patient outcomes and preventing errors. There was however unanimous agreement that nontechnical skills are an under represented and poorly acknowledged facet of orthopaedic training with most of the emphasis on technical proficiency.
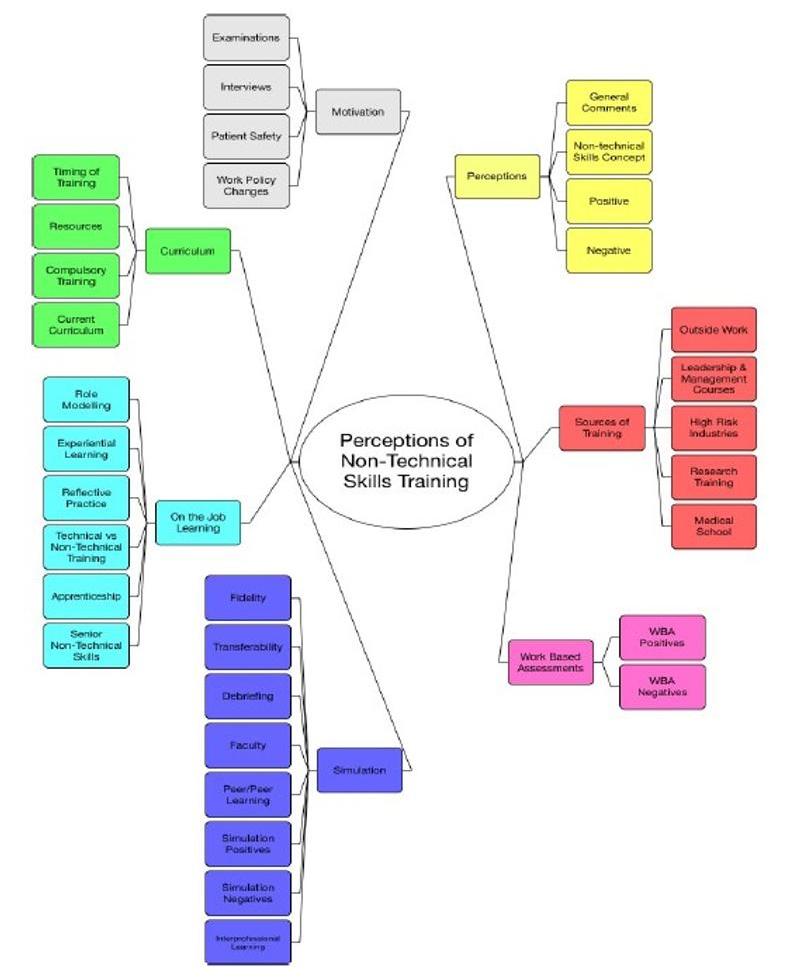
The two major methods of learning non-technical skills were immersive simulated scenarios and on the job learning each with their benefits and drawbacks. Simulation was found to be an excellent method of learning non-technical skills with participants reporting that the immersive scenarios had high face validity and the ability to learn from peers and allied health care professionals through debriefing. On the job learning was found to be more a nebulous method of acquiring non-technical skills where trainees reflected on their experiences and absorbed skills from their environment. They were also influenced by culture at work and from informal feedback from their consultants. The orthopaedic trainees were motivated to learn about non-technical skills to improve patient safety but also to progress in their careers as there is an increasing focus on these skills in postgraduate examinations and interviews. The role of work-based assessments (WBAs) in non-technical skills was unclear but need for an increased emphasis in the curriculum was suggested. Finally, orthopaedic trainees seemed to learn about non-technical skills from very early on in their careers in medical school, from other high risk industries and from outside work in general48.
References
- Drife JO. Arise, Sir Lancelot. BMJ. 1999 May 1;318(7192):1221A.
- Re: Arise, Sir Lancelot. The BMJ [Internet]. 2018 Jan 29 [cited 2018 Jan 29]; Available from: http://www.bmj.com/content/318/7192/1221.2/rr/682763
- Yule S, Paterson-Brown S. Surgeons’ non-technical skills. Surg Clin North Am. 2012 Feb;92(1):37–50.
- Yule S, Flin R, Paterson-Brown S, Maran N, Rowley D. Development of a rating system for surgeons’ non-technical skills. Med Educ. 2006 Nov;40(11):1098–104.
- Flin R, O’Connor P. Safety at the Sharp End: A Guide to Non-Technical Skills. 1 edition. Aldershot, England ; Burlington, VT: CRC Press; 2008. 336 p.
- Catchpole K, Ley E, Wiegmann D, Blaha J, Shouhed D, Gangi A, et al. A human factors subsystems approach to trauma care. JAMA Surg. 2014 Sep;149(9):962–8.
- Steven Yule RF, George G. Youngson. Enhancing Surgical Performance: A Primer in Nontechnical Skills. 1st ed. CRC Press; 2016.
- Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System [Internet]. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000 [cited 2017 May 10]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK225182/.
- Reason J. Human error: models and management. BMJ. 2000 Mar 18;320(7237):768–70.
- Reason J. The Human Contribution: Unsafe Acts, Accidents and Heroic Recoveries. 1 edition. Farnham, England ; Burlington, VT: Routledge; 2008. 310 p.
- Catchpole K, Mishra A, Handa A, McCulloch P. Teamwork and error in the operating room: analysis of skills and roles. Ann Surg. 2008 Apr;247(4):699–706.
- Catchpole KR, Dale TJ, Hirst DG, Smith JP, Giddings TAEB. A multicenter trial of aviation-style training for surgical teams. J Patient Saf. 2010 Sep;6(3):180–6.
- Hull L, Arora S, Aggarwal R, Darzi A, Vincent C, Sevdalis N. The impact of nontechnical skills on technical performance in surgery: a systematic review. J Am Coll Surg. 2012 Feb;214(2):214–30.
- Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery. 2003 Jun 1;133(6):614–21.
- Helmreich RL. Managing human error in aviation. Sci Am. 1997 May;276(5):62–7.
- Helmreich RL, Merritt AC, Wilhelm JA. The evolution of Crew Resource Management training in commercial aviation. Int J Aviat Psychol. 1999;9(1):19–32.
- Rhona Flin, Paul O’Connor, Kathryn Mearns. Crew resource management: improving team work in high reliability industries. Team Perform Manag Int J. 2002 Jun 1;8(3/4):68–78.
- DeAnda A, Gaba DM. Role of experience in the response to simulated critical incidents. Anesth Analg. 1991 Mar;72(3):308–15.
- Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc J Soc Simul Healthc. 2007;2(2):115–25.
- Reznek M, Smith-Coggins R, Howard S, Kiran K, Harter P, Sowb Y, et al. Emergency medicine crisis resource management (EMCRM): pilot study of a simulation-based crisis management course for emergency medicine. Acad Emerg Med Off J Soc Acad Emerg Med. 2003 Apr;10(4):386–9.
- Knudson MM, Khaw L, Bullard MK, Dicker R, Cohen MJ, Staudenmayer K, et al. Trauma training in simulation: translating skills from SIM time to real time. J Trauma. 2008 Feb;64(2):255-263-264.
- McClelland G. Assessing scrub practitioner non-technical skills: a literature review. J Perioper Pract. 2015 Feb;25(1–2):12–8.
- Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Development of a behavioural marker system for scrub practitioners’ non-technical skills (SPLINTS system). J Eval Clin Pract. 2013 Apr;19(2):317–23.
- Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Evaluation of the Scrub Practitioners’ List of Intraoperative Non-Technical Skills system. Int J Nurs Stud. 2012 Feb;49(2):201–11.
- Mitchell L, Flin R, Yule S, Mitchell J, Coutts K, Youngson G. Thinking ahead of the surgeon. An interview study to identify scrub nurses’ non-technical skills. Int J Nurs Stud. 2011 Jul;48(7):818–28.
- Levine AI, Jr SD, Schwartz AD, Sim AJ. The Comprehensive Textbook of Healthcare Simulation. Springer Science & Business Media; 2013. 718 p.
- Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. 2010 Oct 20;304(15):1693–700.
- Pawlik TM, Urbach DR, Halverson AL, Evidence-Based Reviews in Surgery Group. Is there an association between implementation of a medical team training program and surgical mortality? Can J Surg J Can Chir. 2013 Feb;56(1):65–8.
- Yule S, Rowley D, Flin R, Maran N, Youngson G, Duncan J, et al. Experience matters: comparing novice and expert ratings of non-technical skills using the NOTSS system. ANZ J Surg. 2009 Mar;79(3):154–60.
- Yule S, Flin R, Maran N, Rowley D, Youngson G, Paterson-Brown S. Surgeons’ nontechnical skills in the operating room: reliability testing of the NOTSS behavior rating system. World J Surg. 2008 Apr;32(4):548–56.
- Yule S, Flin R, Paterson-Brown S, Maran N. Non-technical skills for surgeons in the operating room: a review of the literature. Surgery. 2006 Feb;139(2):140–9.
- Mishra A, Catchpole K, McCulloch P. The Oxford NOTECHS System: reliability and validity of a tool for measuring teamwork behaviour in the operating theatre. Qual Saf Health Care. 2009 Apr;18(2):104–8.
- Robertson ER, Hadi M, Morgan LJ, Pickering SP, Collins G, New S, et al. Oxford NOTECHS II: a modified theatre team non-technical skills scoring system. PloS One. 2014;9(3):e90320.
- Undre S, Healey AN, Darzi A, Vincent CA. Observational assessment of surgical teamwork: a feasibility study. World J Surg. 2006 Oct;30(10):1774–83.
- Amaya Arias AC, Barajas R, Eslava-Schmalbach JH, Wheelock A, Gaitán Duarte H, Hull L, et al. Translation, cultural adaptation and content re-validation of the observational teamwork assessment for surgery tool. Int J Surg Lond Engl. 2014 Dec;12(12):1390–402.
- Sevdalis N, Lyons M, Healey AN, Undre S, Darzi A, Vincent CA. Observational teamwork assessment for surgery: construct validation with expert versus novice raters. Ann Surg. 2009 Jun;249(6):1047–51.
- Wood TC, Raison N, Haldar S, Brunckhorst O, McIlhenny C, Dasgupta P, et al. Training Tools for Nontechnical Skills for Surgeons-A Systematic Review. J Surg Educ. 2016 Dec 20.
- Doumouras AG, Keshet I, Nathens AB, Ahmed N, Hicks CM. A crisis of faith? A review of simulation in teaching team-based, crisis management skills to surgical trainees. J Surg Educ. 2012 Jun;69(3):274–81.
- Dedy NJ, Bonrath EM, Zevin B, Grantcharov TP. Teaching nontechnical skills in surgical residency: a systematic review of current approaches and outcomes. Surgery. 2013 Nov;154(5):1000–8.
- Barrett DS. Are orthopaedic surgeons gorillas? BMJ. 1988 Dec 24;297(6664):1638–9.
- Fox JS, Bell GR, Sweeney PJ. Are orthopaedic surgeons really gorillas? BMJ. 1990 Dec 22;301(6766):1425–6.
- Subramanian P, Kantharuban S, Subramanian V, Willis-Owen S a. G, Willis-Owen CA. Orthopaedic surgeons: as strong as an ox and almost twice as clever? Multicentre prospective comparative study. BMJ. 2011 Dec 15;343:d7506.
- Heaton SR, Little Z, Akhtar K, Ramachandran M, Lee J. Using simulation to train orthopaedic trainees in non-technical skills: A pilot study. World J Orthop. 2016 Aug 18;7(8):475–80.
- Vaghela K, Lee J, Akhtar K. Development and validation of a multi-disciplinary orthopaedic non-technical skills course. BMJ Simul Technol Enhanc Learn. 2016 Nov 1;2(Suppl 1):A26–A26.
- R. Smith, M. Williams, T. Ball. High fidelity multi-disiplinary team simulation for the development of non-technical skills in Trauma and Orthopaedics (T&O): A feasibility study. BOA 2017 Annu Congr ACC Liverp UK. (74).
- Steinemann S, Berg B, Skinner A, DiTulio A, Anzelon K, Terada K, et al. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ. 2011 Dec;68(6):472–7.
- Bamford, R. Putting the Boot In intensive simulations based on training to prepare surgical trainees for practice. J Trauma Orthop. 2015;3(4):48.
- Vaghela K, Rice, S. Perceptions of Trauma and Orthopaedic Surgeons of Non-Technical Skills Training. MSc Thesis. [Royal College of Physicians]: University College London; 2017.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006 Jan 1;3(2):77–101.
- GMC. Good Medical Practice. GMC; 2017.
- ISCP [Internet]. [cited 2017 Jul 14]. Available from: https://www.iscp.ac.uk/.
