Unmasking problems due to disposable FFP3 masks: Snapshot survey on FFP3 masks usage by frontline healthcare professionals during COVID-19 pandemic
By R Rammohana, Viju Varadarajanb and Khitish Mohantyc
aSpecialist Trainee, Trauma & Orthopaedics, University Hospital of Wales, Heath Park, Cardiff, UK
bConsultant Anaesthetist, Princess of Wales Hospital, Bridgend, UK
cConsultant Trauma & Orthopaedic Surgeon, University Hospital of Wales, Heath Park, Cardiff, UK
Corresponding author email: [email protected]
Published 10 July 2020
Abstract
Purpose: Frontline healthcare professionals using protective face masks during the COVID-19 pandemic have reported symptoms such as facial bruising and skin damage over social media. This snapshot survey was aimed at evaluating the extent and severity of such adverse physical effects experienced by users of disposable FFP3 masks (Filtering Face Piece mask class 3).
Methodology: All healthcare staff using disposable FFP3 masks were invited to answer an online questionnaire. Data on duration of mask usage, tolerance time, extent of pain or discomfort, general and facial symptoms experienced were collected.
Results: We received 209 responses of which 47.4% (n=99) reported moderate-to-severe pain or discomfort after wearing FFP3 masks. Pressure marks over the face and nose (83.7%, n=175) and ‘thirst’ (66.1%, n=138) were the most common facial and general symptoms experienced respectively. The average duration of FFP3 mask usage was two hours or more in 83% (n=175) but only 66.5% (n=139) could tolerate it for 60 minutes or less. There was a statistically significant association between duration of usage and severity of pain or discomfort experienced (Kruskal-Wallis test, p=0.0007).
Conclusion: A high proportion of health care professionals experienced adverse physical symptoms following the use of disposable FFP3 masks, which is dependent on the duration of usage. Professionals working in intensive care units and theatre settings were more likely to experience severe symptoms. Safer alternatives such as full-face masks or powered respirators with hoods may need to be considered for the safety and well-being of healthcare staff during COVID-19 pandemic.
Introduction
COVID-19 is a respiratory infectious disease caused by novel coronavirus designated as Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). COVID-19 is predominantly transmitted by respiratory droplets, aerosols and through contact with contaminated surfaces1. As COVID-19 rapidly spread and transformed into a pandemic, frontline healthcare professionals (HCP) were advised to use Personal Protective Equipment (PPE). Face masks, also known as Filtering Face Piece (FFP) masks in Europe, are an essential and vital part of PPE offering respiratory and facial protection. FFP3 masks (Filtering Face Piece mask class 3) are the Respiratory Protective Devices manufactured according to the European Standard ‘EN 149:2009’2, with a filtration efficiency of at least 99%. For these masks to be effective, users should ensure that the mask achieves a good seal around the nose and cheeks and that there are no leaks around the margins. Fit testing is usually carried out before use of these masks in the clinical area. Use of FFP3 masks is recommended by Public Health England for all HCP carrying out Aerosol Generating Procedure (AGP) and when working in high-risk units where AGPs are carried out3. AGPs include intubation, tracheostomy and surgical procedures involving high-speed devices1.
As the number of COVID-19 cases increased exponentially, frontline HCP who used these disposable FFP3 masks as per recommendation, started reporting problems such as pressure damage to the skin, discomfort, bruising, etc. Photographs depicting such symptoms were posted over social and print media4,5. To evaluate the extent and severity of such physical effects and to identify any other adverse symptoms experienced by the users of FFP3 masks, this voluntary survey was undertaken. This survey was also aimed at identifying the average duration of usage and the tolerance time before it becomes uncomfortable.
Methods
This snapshot survey was conducted at hospitals providing secondary and tertiary level care from two neighbouring Local Health Boards. The target participants for the survey were the frontline healthcare professionals using disposable FFP3 masks when caring for patients with suspected or confirmed COVID-19 and also all personnel participating in AGP irrespective of the COVID status of the patient. The questionnaire was prepared and hosted online using Google Forms (Google LLC, California, USA). The link was advertised at various display boards in hospital clinical areas, circulated via emails and messenger applications. The survey was hosted online from 25th April 2020 to 17th May 2020. The respondents were allowed to share the links with their colleagues to gain more responses from the target group.
The survey form included introductory explanations detailing the purpose, inclusion criteria, data collection methodology and privacy statements. The survey was voluntary and anonymous, with no data identifying the respondents were collected. The survey consisted of questions and statements relating to the experience of using the disposable FFP3 masks, as listed in Table 1. The questionnaire included questions to identify the role of HCP and their average duration of FFP3 mask usage. Validated five-point Likert scale6 responses were used for questions relating to user satisfaction on fit testing of masks and intensity of discomfort after mask usage. Adverse physical symptoms experienced by HCP, if any, were recorded using multiple-choice responses, with free text option to record any other related symptom experienced by the respondent. These symptoms were further subdivided into general and facial symptoms. The participants were also asked to indicate the duration they could tolerate the mask before experiencing any discomfort.
|
Q1 |
In what role do you have to use FFP3 mask? |
Medical Doctor, Surgeon/Surgical Assistant, Anaesthetist, Theatre Personnel, Intensive Care Doctor, Intensive Care Nurse, Nurse in wards, Emergency unit Personnel, Other Healthcare Worker |
|
Q2 |
Were you satisfied with the method used for FIT testing of FFP3 mask? |
Completely Satisfied, Very Satisfied, Moderately Satisfied, Slightly Satisfied, Not at all Satisfied |
|
Q3 |
On an average, for how long do you continuously wear FFP3 masks? (for each instance of mask use) |
<1 hour, 1 to 2 hours, 2 to 3 hours, 3 to 4 hours, > 4 hours |
|
Q4 |
Do you experience any pain or discomfort after using FFP3 masks? |
None, Very Mild, Mild, Moderate, Severe |
|
Q5 |
Do you agree that the sealing straps of the current FFP3 are comfortable? |
Strongly Agree, Agree, Neither Agree nor Disagree, Disagree, Strongly Disagree |
|
Q6 |
Do you experience any of the following general symptoms after using FFP3 masks? (tick more than one if applicable) |
Cough, Dryness/Irritation of throat, Difficulty in breathing/Breathlessness, Thirst, Exhaustion, Claustrophobia, Change in voice, None of the above, Any other symptoms (free text option) |
|
Q7 |
Do you experience any of the following facial symptoms after use of FFP3 masks? (tick more than one if applicable) |
Facial discomfort, Bruising of Face, Pressure marks over Face and Nose, Itching or Burning of Face and Nose, None of the above, Any other symptoms (free text option) |
|
Q8 |
How long can you wear FFP3 masks along with full PPE before experiencing discomfort? |
30 min or less, 45 min, 60 min, 90 min, 2 hours, more than 2 hours. |
|
Q9 |
Any other comment or suggestions to improve user friendliness of FFP3 mask |
Free text |
Statistical analysis was performed using R software (version 4.0.0, R Foundation for Statistical Computing, Vienna, Austria). Role-based sub-groups and their categorical and ordinal responses were reported as proportions. We have reported both mean and medians for Likert scale responses, including the measure for spread of data i.e. Standard Deviation. For qualitative data, non-parametric tests were used to determine statistical significance. The statistical significance was set at p-value < 0.05.
Results
A total of 209 participants completed the survey questionnaire and shared their experience of using the FFP3 masks with us, as depicted in Figure 1. The most common user group were the operating department personnel (20.1%, n = 42) followed by the intensive care doctors (19.1%, n = 40 each). The ‘other’ group included emergency unit staff, medical doctors, nurses in wards and other healthcare workers. As the survey was kept anonymous, no other information about participants was available.
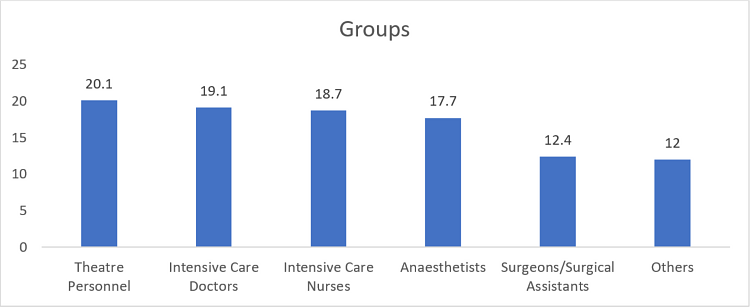
Figure 1: Participants and their relative frequencies depending on their roles (in percentage).
The Likert scale responses were each given a discrete number from one to five for data analysis as shown in Table 2. All HCP had to undergo fit testing before being able to use the FFP3 masks. The responses for questions on fit testing, intensity of pain or discomfort experienced, and comfort relating to the straps are as shown in Table 3. More than half the respondents were satisfied with the fit testing methods used (completely satisfied to very satisfied: 57.5%, n = 120). Moderate to severe discomfort or pain after wearing the mask was reported by 47.4% (n = 99). A similar proportion of respondents disagreed that the straps were comfortable (disagree to strongly disagree, 52.6% n = 110).
|
Completely Satisfied |
None |
Strongly Agree |
1 |
|
Very Satisfied |
Very Mild |
Agree |
2 |
|
Moderately Satisfied |
Mild |
Neither Agree nor Disagree |
3 |
|
Slightly Satisfied |
Moderate |
Disagree |
4 |
|
Not at all Satisfied |
Severe |
Strongly Disagree |
5 |
|
Question |
1 (in %) |
2 (in %) |
3 (in %) |
4 (in %) |
5 (in %) |
Mean Response |
Standard Deviation |
Median |
|
Were you satisfied with the method used for FIT testing of FFP3 mask? |
46 (22.1%) |
74 (35.4%) |
71 (33.9%) |
14 (6.7%) |
4 (1.9%) |
2.3 |
0.95 |
2 |
|
Do you experience any pain or discomfort after using FFP3 masks? |
7 (3.3%) |
29 (13.9%) |
74 (35.4%) |
86 (41.1%) |
13 (6.3%) |
3.33 |
0.91 |
3 |
|
Do you agree that the sealing straps of the current FFP3 are comfortable? |
3 (1.4%) |
40 (19.1%) |
56 (26.9%) |
78 (37.3%) |
32 (15.3%) |
3.5 |
1.01 |
4 |
The most common general symptom reported was Thirst (66.1%, n = 138) followed by dryness or irritation of throat (57.9%, n = 121). The most common facial symptom was pressure marks over face and nose (83.7%, n = 175) followed by facial discomfort (67.9%, n = 142). Figures 2 and 3 portray the common facial symptoms experienced by one of the participants.

Figure 2: Photograph of a participant showing facial bruising following FFP3 mask usage.

Figure 3: Photograph of a participant showing Pressure marks due to FFP3 mask usage.
The common symptoms reported under ‘any other symptoms’ were ear pain because of straps, dry skin, headache and dizziness. Figures 4 and 5 depict the percentages of general and facial symptoms reported by users.
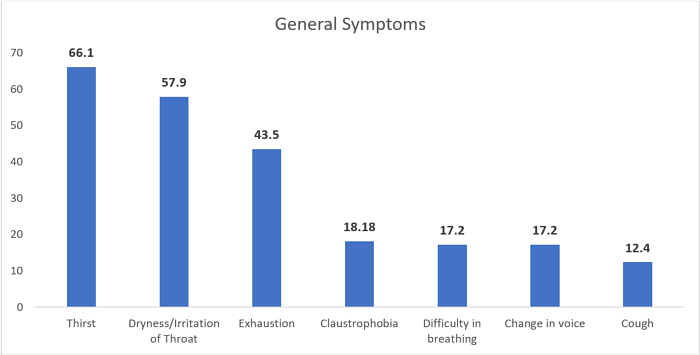
Figure 4: General Symptoms experienced by participants (in percentages).
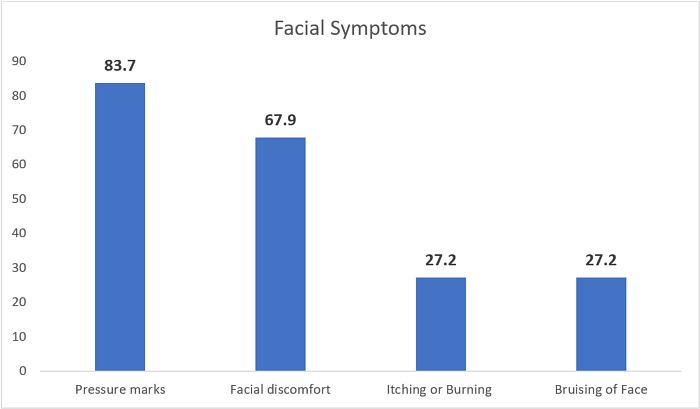
Figure 5: Facial symptoms reported by participants (in percentage).
As depicted in Figure 6, 83% of respondents used the mask for at least two hours or more (n = 175) at each instance of use. Of these, 40.7% (n = 85) used the mask for two to three hours and 29.7% (n = 62) used the masks for three to four hours. Two-thirds of respondents reported that they could tolerate wearing FFP3 masks continuously for 60 minutes or less (66.5%, n = 139) as depicted in Figure 7.
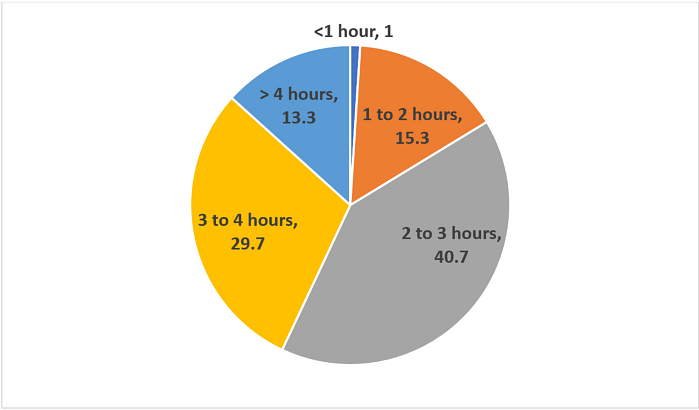
Figure 6: Average duration of usage (in percentage).
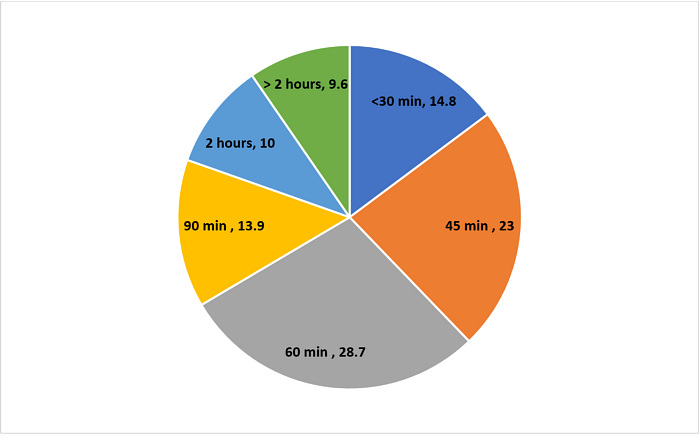
Figure 7: Responses for the question: “How long can you wear FFP3 masks before experiencing discomfort?” (in percentage).
We compared the duration of mask usage to the intensity of discomfort or pain experienced by the participants. As the duration of usage increased, the proportion of users experiencing moderate to severe symptoms increased (Figure 8). This association was statistically significant (Kruskal Wallis Test, p = 0.0007216).
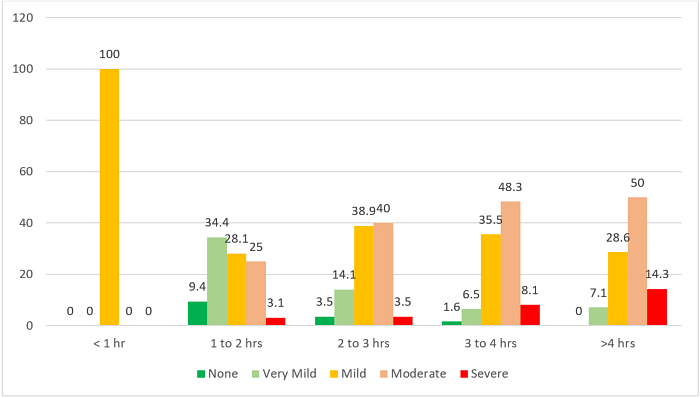
Figure 8: Intensity of pain or discomfort (Likert scale) reported by participants, classified depending on duration of usage. Values shown in percentage, calculated for each group.
We also noted that a statistically significant proportion of users within certain groups wore the masks for a longer duration than others (Kruskal Wallis test, p = <0.00001), and these groups reported a higher proportion of moderate to severe symptoms of pain or discomfort (Figure 9 and 10). The association between various user groups and the intensity of symptoms was statistically significant (Kruskal Wallis Test, p = 0.008).
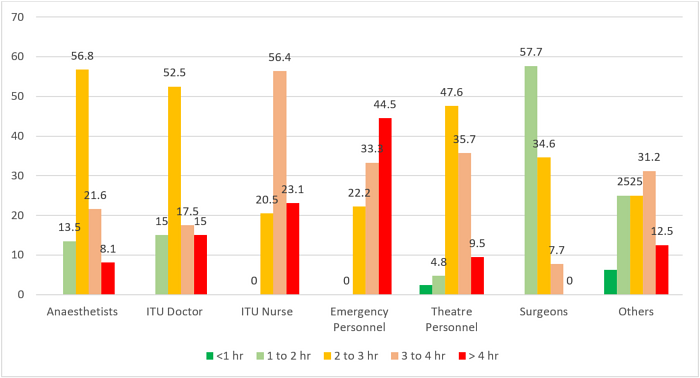
Figure 9: Duration of mask usage in various groups. Values shown in percentage, calculated for each user group.
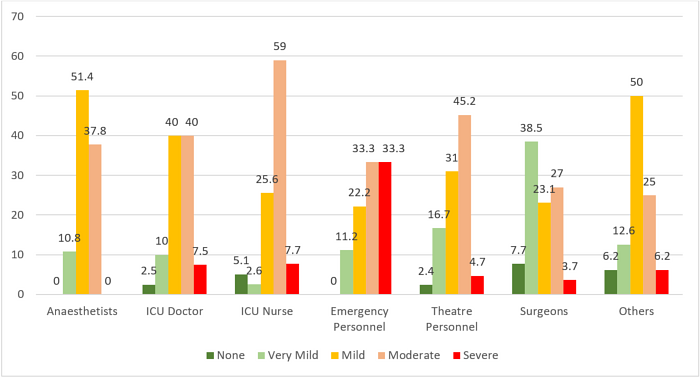
Figure 10: Intensity of pain or discomfort (Likert Scale) for each user group. Values expressed in percentage, calculated for each group.
Discussion
The initial measures adopted during the COVID-19 pandemic, by most countries including the United Kingdom, were aimed at ‘flattening the curve’, which is aimed at reducing the daily average number of new cases. The underlying intention was to decrease the number of cases to a level that can be managed effectively by the health care system. In a population which has never been exposed to the novel coronavirus, the virus will continue to transmit until enough susceptible individuals have been infected or vaccinated or a cure is found. Mathematical models predict rebound increase in the number of COVID-19 cases once the social distancing measures are lifted7 It is likely that HCP will continue caring for patients with COVID-19, for which continued use of PPE and appropriate respiratory protectors such as FFP3 will be necessary in the near future.
This survey has demonstrated that almost half of the respondents experienced moderate to severe pain or discomfort after wearing these masks, with two-thirds expressing their intolerance to use the masks beyond 60 minutes or less. Symptoms such as thirst, pressure effects on face and nose are prevalent in 66% to 80% of users. These symptoms can potentially affect concentration and performance of HCP, especially in settings such as the Intensive Care Unit (ICU) and operating theatres.
Pressure symptoms over nose after prolonged use can preclude further use of these respirators until the symptoms abate, which would mean the HCP cannot continue to work in high-risk clinical areas. This can adversely affect staff availability during the current crisis when units are already struggling to manage with a reduced workforce. Improper application of these masks by HCP, either to prevent or to manage early symptoms, can put them at risk of contracting or transmitting the infection to others.
As things progress, semi-elective or elective surgical services will eventually need to be resumed. Based on the findings of our survey, it is likely that more than half of users will experience discomfort during the course of a surgical procedure lasting more than 60 minutes. Key HCP working in ICU settings and Emergency Units, who wear the masks continuously for a longer duration, will be more affected than others.
Measures to alleviate pressure symptoms from masks such as application of hydrocolloid dressings8 or adequate training on correct usage9 can only work in the short term. We believe that our survey results provide enough evidence for healthcare systems to consider solutions that are safe, comfortable, economically viable and available in sufficient quantity for managing COVID-19 cases for an extended duration.
From the insights derived from this survey, we propose a few solutions that may counteract certain limitations of disposable FFP3 masks. Full-face Respirators or Half-face Respirators with wider straps are considered more comfortable to use and for longer duration as well10. These being reusable, can be a cost-effective device when considered for the duration it will be required for. The current guidelines from Public Health England also consider them a safe alternative to disposable FFP3 masks3. For HCP who routinely need to use these protective masks for longer duration can also use Powered Respirators with hoods or helmets with appropriate filters and positive pressure ventilation, which can provide more comfort to the user11. These options have a higher initial investment cost but offer more comfort and potentially less adverse symptoms to the user. Some hospitals have pioneered the use of indigenously developed respirator hoods to combat the challenges faced in procuring PPE12. The findings of this survey were presented at the Institutional Surgical Board meeting and received a positive response. Our future steps would be to re-evaluate user-experience once new measures are put in place by the health board.
To our knowledge, this survey is the only published evidence demonstrating user experience of using FFP3 masks in the current pandemic.Responses by HCP who are the most common users of these masks provide an accurate account of the problems faced by the users on a day to day basis which can be generalised. Recall bias and smaller sample size are some of the limitations of this survey.
Conclusion
This survey has demonstrated that the use of disposable FFP3 masks by health care professionals results in moderate to severe adverse symptoms in a high proportion of the users which is dependent on the duration of its use and is more prevalent amongst personnel working in Intensive Care, Emergency Unit and Theatre settings. Reusable full-face masks or powered respirators with hoods may need to be considered as safer alternatives to disposable FFP3 masks if the use of respiratory and facial protection devices is warranted for an extended duration in this current COVID-19 pandemic. The initial cost of the proposed respirators will be offset against the cost of disposable masks and staff sickness due to mask related illness.
Conflict of interest
All authors declare no conflicts of interest. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Public Health England (2020). COVID-19: infection prevention and control guidance. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/881489/COVID-19_Infection_prevention_and_control_guidance_complete.pdf.
- European Committee for Standardizaton (2009). EN 149:2001+A1:2009: Respiratory protective devices - Filtering half masks to protect against particles - Requirements, testing, marking Respiratory protective devices. Available at: https://standards.cen.eu/dyn/www/f?p=204:110:0::::FSP_PROJECT:32928&cs=1B0AB06FEB70E43960D46D1198C37CC09.
- Public Health England (2020). Recommended PPE for healthcare workers by secondary care inpatient clinical setting, NHS and independent sector.
- Heren K. Italy nurses battling coronavirus outbreak share photos of exhaustion as some left bruised by face masks. The Evening Standard. 2020 [cited 2020 Jul 4]. Available at: https://www.standard.co.uk/news/world/italy-nurses-coronavirus-outbreak-exhaustion-a4384861.html.
- Pearson-Jones P. NHS workers share exhausted selfies showing bruised faces long shifts. Daily Mail UK. 2020 [cited 2020 Jul 4]. Available at: https://www.dailymail.co.uk/femail/article-8139549/NHS-workers-share-exhausted-selfies-showing-bruised-faces-long-shifts.html.
- Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22 140:55.
- Ge Y, Sun S. Estimation of Coronavirus Disease Case-Fatality Risk in Real Time. Emerg Infect Dis. 2020. [Epub ahead of print.
- Payne A. Covid-19: Skin damage with prolonged wear of FFP3 masks. BMJ. 2020;369:m1743.
- Lam U-N, Md Mydin Siddik NSF, Mohd Yussof SJ, Ibrahim S. N95 respirator associated pressure ulcer amongst COVID-19 health care workers. Int Wound J. 2020 May 12. [Epub ahead of print].
- Coia JE, Ritchie L, Adisesh A, Makison Booth C, Bradley C, Bunyan D, et al. Guidance on the use of respiratory and facial protection equipment. J Hosp Infect. 2013;85(3):170-82.
- Health and Safety Executive (2013). Respiratory protective equipment at work, a practical guide. Available at: http://www.hse.gov.uk/pubns/priced/hsg53.pdf.
- Hepwoth T. Coronavirus: Hospital orders 5,000 respirator hoods. BBC News. 2020 [cited 2020 Jul 4]. Available at: https://www.bbc.co.uk/news/av/uk-england-hampshire-52476199/coronavirus-hospital-orders-5000-respirator-hoods.
