Andrew Jonesa, Harriet Lewisb and Peter Kempshallc
aST7 Trauma and Orthopaedics, Gloucestershire Hospitals NHS Foundation Trust
bCT2 Trauma and Orthopaedics, Gloucestershire Hospitals NHS Foundation Trust
cConsultant Orthopaedic Surgeon, Gloucestershire Hospitals NHS Foundation Trust
Corresponding author e-mail: [email protected]
Published 15 May 2020
Introduction
A fractured neck of femur continued to be a very common presentation to orthopaedic departments across the country during the coronavirus pandemic. Gloucestershire hospitals NHS trust manages 760 acute fractured neck of femur patients on average each year with 60% being intracapsular fractures. In line with NICE guidance1 and BOA BOAST guidelines hemiarthroplasty and total hip replacement are used to treat patients with this condition allowing patients to be mobilised post operatively, either on day of or day after surgery.
Routine practice in most centres across the UK, is to obtain a check radiograph after the procedure in order to evaluate the hip prior to discharge as there is a small risk of peri-prosthetic fracture, component malposition and implant dislocation2-5.
The driver for change in practice has been the lessons learned through the coronavirus pandemic and how to create a ‘new normal’ working pattern in the aftermath.
Reducing the movement of patients within the hospital was vital to decrease possible nosocomial transmission of COVID-19 and prompted an emergent change in practice to stop the routine check radiographs following hip hemiarthroplasty.
The change in practice has been closely audited over the six weeks of COVID-19 pandemic emergency hospital working pattern. No complications were observed with x-rays only being requested if patients are slow to mobilise, had excessive pain, oozy wound at day 10, or deformed limb post op.
From this change, to risk assess whether this could be sustainable for the future ‘new normal’ working and a change in local policy we retrospectively reviewed our practice over the last 3 years.
In this study, we aim to show that the change in practice generated in response to the COVID-19 pandemic is safe to be adopted as the ‘new normal’ and thereby not performing a routine check radiograph of postoperative intracapsular hip fractures.
Methods
The details of all hip fractures managed at our trust for 3 years (1st January 2017 - 31st March 2020) were obtained using the National Hip Fracture Database6. From this data, only those who had undergone a hip hemiarthroplasty or total hip replacement for intra-capsular fractures were included. Patients who had undergone fixation of an intracapsular fracture were excluded as these cases are done under image intensifier guidance.
For each patient, the post-operative imaging was reviewed using the hospital PACS system, to establish firstly if they had suffered any mechanical complications including fracture or dislocation, and if so, whether this was evident on the routine post-operative check radiograph or subsequent, specially requested radiographs, after a satisfactory post-operative check x-ray. Images were reviewed up to three months post date of surgery to look for early failures / complications.
Data was also collected regarding the time it took from surgery to check radiograph, and if a patient had multiple ‘check radiographs’.
The cost of an anterior-posterior and lateral hip x-ray was obtained from the accounts department, and compared to that in the literature7.
Results
During the time period, we managed a total 2,348 neck of femur fractures within our trust. Of these, 1,230 were intracapsular fractures managed with either a hip hemiarthroplasty (n= 999) or total hip replacement (n=231). 41 cases had no check radiograph on our PACS system. Of these patients, 29 clinically deteriorated and were placed on an end of life care pathway during the acute admission. An x-ray in this instance was not deemed necessary. The remaining 12 were discharged with no postoperative x-ray. This study group consisted of a total of 960 cases of hemiarthroplasty and 229 total hip replacements for inclusion in the analysis.
Of the 960 hemiarthroplasties, there was a 1.25% overall dislocation risk (12/960) at 90 days. Immediate postoperative dislocation was identified in 0.1% of cases (1/960) on the routine post-operative radiographs. Subsequent complications were noted after a satisfactory initial check radiograph. In the THR group, there was a dislocation rate of 8.3% (19/229), with an immediate postoperative dislocation rate of 1.3% (3/229) observed. The additional 16 cases were identified radiologically following appropriate clinical suspicion after having a normal post-operative radiograph.
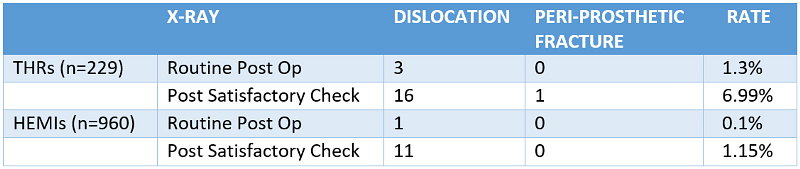
Table 1: Complications noted on post-operative radiographs
The mean number of days from surgery to check radiograph was 3.4 days (Interquartile Range 2-4 days) with an overall range of 0 to 26 days. Seventy-five (n=75) patients had more than one check radiograph due to inability to comply with radiographs being taken as a result of cognitive impairment or pain. This resulted in the total number of episodes being greater than the number of procedures performed. For the hemiarthroplasty cohort of patients there were 55 additional episodes compared with 20 in the THR group.
The cost of the imaging episode is based on NHS reference costs for 2018 using the U134 code. This is comparable to other costs published in the available literature7. The routine check radiograph includes two views, an anterior-posterior (AP) pelvis view, as well as an AP and lateral of the hip. Data from our accounts department based on code U134 provided a cost per patient of £29.19 for check radiographs.
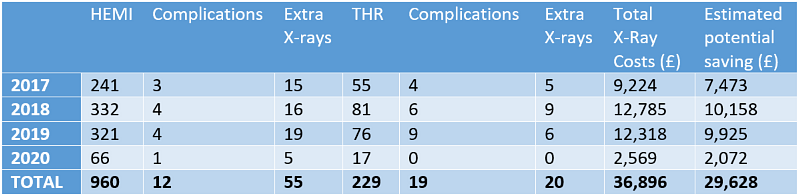
Table 2: The year on year estimated potential cost savings are shown in the table below, (prices to nearest pound).
Discussion
In our Trust, and similarly in many others across the UK, it was routine practice to take a check radiograph following treatment of intra-capsular neck of femur fractures treated with either a hemiarthroplasty or THR. However, the COVID-19 pandemic forced us to change practice.
Nosocomial transmission
This change in practice adopted by our trust was driven by the need to reduce the movement of staff and high-risk patients in particular, around the hospital and therefore help to reduce possible avenues of nosocomial transmission. The latest national level data from the BODS shows a 7% nosocomial transmission rate for hip fracture patients while in hospital.
Efficacy
To review and sustain this change, we have shown that the number of complications identified on this investigation is very low (0.1%) and therefore we feel the change is both efficacious and safe. The majority of complications occurred in patients who had previously had a ‘satisfactory’ post-operative radiograph, (see Table 1). This was most marked in the hemiarthroplasty group, where in almost 1,000 patients, there was only one case of dislocation noted on the check radiograph. The remaining 11 cases of dislocation occurred after the patient had what was deemed a satisfactory x-ray.
If patients were failing to progress or had a subsequent traumatic episode then a radiograph should be taken at that time. We believe that a request for investigation, based on clinical need, is a better use of resources and should be considered on a case by case basis rather than as a matter of routine.
In accordance with NICE CG124, all of our hemiarthroplasty patients are mobilised day one post operatively1. Low energy traumatic fragility fractures are most common in the clinically frail, elderly subgroup who often have multiple co-morbidities including dementia. Aside from minimising transfers around the hospital during the pandemic, minimising transfers for patients with an element of pre-existing cognitive dysfunction, or acute delirium is preferable. Other studies have demonstrated a possible link with a delay in discharge due to the x-ray, as well as it being a distressing for the patients with dementia8-11.
Cost
It has been an economic focus to reduce costs in the NHS in the last decade. We have shown that by sustaining this change in practice, as a result of the COVID-19 crisis, the estimated cost saving to NHS Trusts could be in the region of £10,000 per year. This doesn’t include the ‘hidden’ costs of portering requirements and the time for nursing staff being away from the ward to accompany patients, meaning the overall cost saving is higher.
As a result of the crisis, reducing costs to a depleted NHS system will be paramount for delivering and reintroducing a sustainable service. By stopping the routine use of post-operative check x-rays a potential contribution to these savings can be made safely as well as reducing pressure on radiology departments.
THR
This study has reported that the rate of complications is higher in the group having a total hip replacement, with 3 cases of dislocation noted on the check x-ray. Although the majority of complications did occur after a normal check x-ray, we believe a routine x-ray is beneficial in this group.
The group of patients undergoing THRs are generally younger, less frail and more active and potentially have a higher chance of requiring subsequent revision surgery12. When performing revision surgery, it is useful to know the original position of implants to assess for implant migration or loosening. For this reason, we believe that patients undergoing a THR should have a post-operative radiograph routinely for base line comparison.
Conclusions
Our study shows that the changes implemented as part of the COVID-19 pandemic response can be sustained safely as the ‘new normal’ procedure at a lower cost. The routine post-operative radiograph is not necessary as they do not influence the acute management of patients undergoing hemiarthroplasty.
We do advocate the continuing use for total hip arthroplasty.
References
- NICE (2017). Hip fracture management. Clinical Guideline [CG124]. Available at: https://www.nice.org.uk/guidance/cg124.
- Noon AP, Hockings M, Warner JG. Dislocated Thompson hemiarthroplasty – the management of the recurrent dislocator. Injury. 2005;36(5):618-21.
- Pace TB, Prather B, Burnikel B, Shirley B, Tanner S, Snider R. Comparative Outcomes Assessment: Hip Hemiarthroplasty as an Alternative to THA in Patients with Surgically Pristine Acetabulum – Is There Still a Role? ISRN Orthopaedics. Aug 12:2013.
- Champion LM, McNally SA. Dislocation after revision of hemiarthroplasty to total hip replacement. Injury. 2004;35:161-4.
- Bush JB, Wilson MR. Dislocation After Hip Hemiarthroplasty: Anterior Versus Posterior Capsular Approach. Orthopedics. 2007;30(2):138-44.
- Royal College of Physicians (2020). National Hip Fracture Database. Available at: https://www.nhfd.co.uk/.
- Chen A, Sabharwal S, Akhtar K, Makaram N, Gupte CM. Time- driven activity-based costing of total knee replacement surgery at a London teaching hospital. Knee. 2015;22(6):640-5.
- George J, Long S, Vincent C. How can we keep patients with dementia safe in our acute hospitals? A review of challenges and solutions. J R Soc Med. 2013;106(9):355-61.
- Chakravarthy J, Mangat K, Qureshi A, Porter K. Postoperative Radiographs Following Hip Fracture Surgery. Do they Influence Patient Management? Int J Clin Pract. 2007;61(3):421-4.
- Westerterp M, Emous M, Vermeulen MC, Erenberg JP, Van Geloven AAW. No Additional Value of Routine Check X-rays after Internal Fixation of Hip Fractures. Eur J Trauma Emerg Surg. 2013;39(2):163-5.
- Riley T, Mounsey E, Blake S. Post-operative screening of hip hemiarthroplasties in theatre. Orthopaedic Proceedings. 2012;94-B(SUPP_XII):10.
- Moerman S, Mathijssen NMC, Tuinebreijer WE, Vochteloo AJH, Nelissen RGHH. Hemiarthroplasty and total hip arthroplasty in 30,830 patients with hip fractures: data from the Dutch Arthroplasty Register on revision and risk factors for revision. Acta Orthop. 2018;89(5):509-14.
