The Early Effect of COVID-19 on Trauma and Elective Orthopaedic Surgery
by Paul Jenkins
Consultant Orthopaedic Surgeon & Clinical Director, Glasgow Royal Infirmary
Published 17 April 2020
Introduction
The COVID-19 pandemic has led to a cessation of non-urgent elective surgery and a reduction in trauma surgery. The disease results from inflection by a novel coronavirus first detected in China in 2019 (SARS-CoV-2). It’s detection and transmission within the United Kingdom (UK) has led to a national emergency response. Part of this has been to release hospital capacity and allow redeployment of staff to the care of patients with COVID-19. This has significantly affected Trauma & Orthopaedic Surgery. The NHS, along with the British Orthopaedic Association (BOA) have produced a BOAST guideline to help guide management of orthopaedic patients during the pandemic1-3.
There has also been concern that patients who have been infected with SARS-CoV-2 but who are pre-symptomatic may suffer morbidity and mortality if symptoms develop after orthopaedic surgery4. In the frail elderly population with fragility fractures COVID-19 can co-present with atypical features such as delirium. There are, however, cases where urgent trauma surgery is still vital to prevent life or limb threatening complications and long term disability. The care of patients with fragility fractures of the hip is particularly challenging as delays to surgery are recognised risk factor for significant complications5.
There is currently defined to be ongoing community transmission of the SARS-CoV-2 virus and therefore the personal protective equipment (PPE) directions of Table 4 of the Public Health England guidelines are in place6. This requires airborne PPE and infection control measures during any AGPs. For orthopaedic surgery this can relate to intubation and extubation at the start and end of the procedure. It also refers to the use of high speed devices that can theoretically aerosolise blood during the procedure7-9.
The aim of this paper is to investigate the early impact of COVID-19 on elective and trauma orthopaedic operating throughout one of the largest healthboards in the United Kingdom.
Patients & Methods
NHS Greater Glasgow & Clyde covers a population of approximately 1.2 million people and employs 44,000 staff. Adult inpatient trauma and elective orthopaedic services are delivered across four acute sites, with a further three ambulatory care hospitals providing day case surgery. Orthopaedic surgery is organised into three sectors throughout the healthboard.
Bluespier (Bluespier Clinical Systems, Droitwich, UK) is used as an electronic patient record throughout all orthopaedic departments. It is used to manage trauma orthopaedic admissions via an 'electronic whiteboard' and plan trauma operating lists.
The period studied was 1 March 2020 to 9 April 2020. The period of 'lockdown' was defined as 24 March 2020 onwards. A query was constructed to extract all procedures undertaken from 1 March 2020. These were compared with procedures undertaken over the same period in 2019. Operations were classified as trauma or elective. Analysis was undertaken with Microsoft Excel (V. 16).
No ethical permission was required as this study was undertaken on anonymised service usage data. No patient or staff identifiable data was extracted from the clinical system.
Results
The total number of orthopaedic procedures undertaken in the board area was 1,322 during the study period compared with 2,111 the previous year. This represents a reduction of 37.4% over the whole period.
Elective
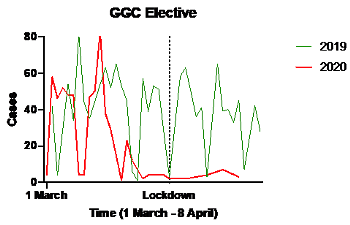
Elective cases fell by 57% from 1,357 cases to 588 over the time period (Figure 1). During the 'lockdown' period from 24 March 2020 onwards the number of elective procedures was reduced by 94.5% from 492 to 27. The cases that did occur were priority one cancer surgery and associated procedures and these were undertaken at a separate facility (Golden Jubilee National Hospital).
Trauma
Trauma surgery fell from 754 operative cases in 2019 to 734 case in 2020 - a 2.7% fall (Figure 2). When the lockdown period was analysed separately, there was a reduction in trauma operating from 279 to 162 – a 23.2% fall (Figure 3).
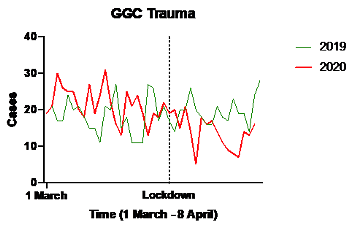
Figure 2: Trauma operating 2020 versus 2019
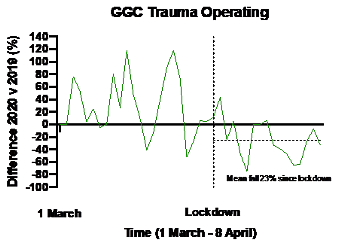
Figure 3: Percentage change 2020 versus 2019 in trauma operating
Discussion
During the period following 'lockdown', elective orthopaedic surgery fell by 94%, leaving only urgent cancer work ongoing, while there was a lesser fall in trauma operating of 23.2%.
There was an initial expectation that there would be a greater fall in trauma surgery as a result of the lockdown period. It was anticipated that the population would be undertaking fewer 'risky' activities such as sport. It was also hypothesised that there might be a fall in alcohol related injuries sustained during nocturnal entertainment. It was also expected that a fall in travel would result in a fall in road traffic accidents. There has however been an anecdotal rise in household DIY related injuries, particularly hand injuries. We have also noted a novel mechanism of injury with two hip fractures sustained by falling during the 'clap for the NHS' event a Thursday evening.
Due to the anticipated fall in elective and trauma surgery many staff have been redeployed to the care of patients with COVID-19. Access to trauma theatre has been reduced as a consequence. Meanwhile it is taking longer to perform surgery due to the classification of many orthopaedic techniques as aerosol generating procedures (AGPs).
As we look towards a post-lockdown period it is likely that there will be a rise in the incidence of trauma as the population returns to normal daily routines. This may occur before repatriation of redeployed staff as the 'flattened curve' will lead to a prolonged period of patients with COVID-19 requiring ICU and ward care.
Unless there is further research clarification of the risks of orthopaedic AGPs, theatre throughput will also not immediately rise. There is a lack of certainty over the specific infection risk of aerosol generating procedures. The prevalence of viraemia in COVID-19 infection is reported to be low9. It is agreed that viraemia tends to occur at a stage when patients are most unwell. There is no clear reported transmission mechanism of aerosolised blood containing virus causing active COVID-19. There is no evidence of bloodborne transmission blood transfusion services do not screen for SARS-CoV-211.
Future strategies will likely require the assessment of clinical signs and symptoms and testing of trauma patients for SARS-CoV-2 active infection and/or prior exposure. This will reduce the risk of patients developing COVID-19 in the post-operative period and may allow de-escalation of the level of PPE required in theatre.
The reduction in trauma operating has been lower than expected. This data highlights the need for ongoing realistic provision of trauma operating capacity. Further challenges are likely when lockdown starts to be lifted. These challenges can be addressed through testing and understanding of disease and immunity in patients and staff alongside greater understanding of the risk of orthopaedically generated aerosols.
References
- British Orthopaedic Association (2020). Emergency BOAST: Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html.
- NHS England, (2020). Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0274-Specialty-guide-Orthopaedic-trauma-v2-14-April.pdf
- NHS England, (2020). Clinical guide for the perioperative care of people with fragility fractures during the coronavirus pandemic. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0086_Specialty-guide-_Fragility-Fractures-and-Coronavirus-v1-26-March.pdf.
- Lei S, Jiang F, Su W, Chen C, Chen J , Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. Eclinicalmedicine 2020;100331 [Epub ahead of print].
- Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, et al. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep. 2018;8(1):13933.
- Public Health England (2020). COVID-19 Personal Protective Equipment. Available here: https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control/covid-19-personal-protective-equipment-ppe.
- Wenner L, Pauli U, Summermatter K, Gantenbein H, Vidondo B, Posthaus H. Aerosol Generation During Bone-Sawing Procedures in Veterinary Autopsies. Vet Pathol. 2017;54(3):425-36.
- Putzer D, Lechner R, Coraca-Huber D, Mayr A, Nogler M, Thaler M. The extent of environmental and body contamination through aerosols by hydro-surgical debridement in the lumbar spine. Arch Orthop Traum Surg. 2017;137(6):743-7.
- Jewett DL, Heinsohn P, Bennett C, Rosen A, Neuilly C. Blood-containing aerosols generated by surgical techniques a possible infectious hazard. Am Ind Hyg Assoc J. 1992;53:228–31.
- Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020;323 [Epub ahead of print].
- Chang L, Yan Y, Wang L. Coronavirus Disease 2019: Coronaviruses and Blood Safety. Transfus Med Rev. 2020. [Epub ahead of print].
