The legal implications of treatment delays since the 2020 pandemic
Authors: Andrew Manktelow and Bertie Leigh
The legal implications of treatment delays since the 2020 pandemic
To say that the COVID-19 pandemic has created a challenge for orthopaedic care in the UK and beyond would be an understatement. Against a pre-existing backdrop of progressively increasing waiting lists the COVID-19 pandemic had a sudden multifactorial effect on the ability to deliver effective orthopaedic care. This change has not been coterminous with the pandemic. The simple truth is that the NHS is not acutely ‘challenged’ or ‘under stress’: it has been failing to deliver an appropriate service within a reasonable timescale which has probably resulted in harm to some patients.
When the pandemic started, the planning to prepare for the unknown was disruptive. How the virus and its transmission would affect routine practices in the emergency department, in the operating theratre and beyond was unknown and yet plans had to be made. Surgeons all remember meetings to discuss how services would need to be reconfigured, how doctors would need to be reassigned to support other services and how acute care could be delivered in the changed environment. All had to be re-organised at short notice and with little, if any, understanding of how things would progress. As doctors were alarmed by the reported experience from regions where the pandemic had progressed more rapidly, the anxiety created was disruptive in its own right.
Elective orthopaedic services were essentially shut down overnight. Many will remember being re-tasked to run minor injuries units. Many had the harrowing experience of working to support exhausted colleagues on medical wards and in the ITU. Re-learning old skills and working hard to apply ‘orthopaedic impetus’ to support other areas of medical practice. Preparations worked well in many situations, in other areas we might have been over prepared, however it would seem clear that in many, we were under prepared and ill-equipped for what transpired.
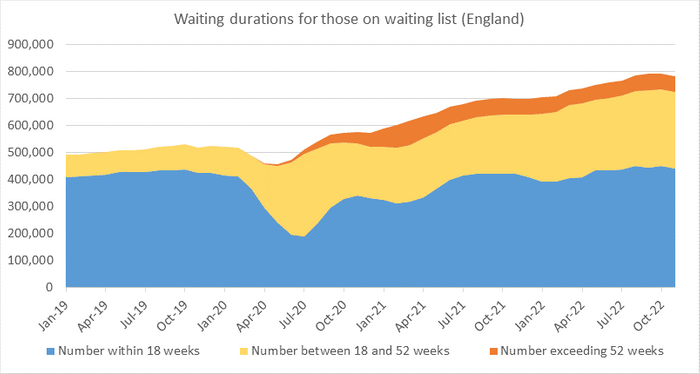
Circumstances were different in different areas of the country and at different times. The net effect was, and is, clear. Within elective orthopaedic surgery, NHS England data shows waiting times are now prolonged out of all recognition compared to those from prior to the pandemic and there is no evidence that things are improving. This is shown clearly in Figure 1, demonstrating how both the numbers of patients on waiting lists and the duration of their waiting time have increased since the start of the COVID-19 pandemic.
A huge amount of work is now being done with elective care centres and hubs designed to try and protect elective services from the unavoidable demands of emergency care within and away from orthopaedics. Behind the numbers are the practical consequences that are harder to encapsulate but are apparent to surgeons. Patients are now approaching elective surgery significantly deconditioned, poorly prehabilitated and with worsening comorbidity. Patients experienced worsened social support, isolation and anxiety during the COVID-19 pandemic that has further compromised their pre-operative situation. The lack of follow-up arrangements during the crisis, when face-to-face clinic appointments were stopped, led to patients re-presenting in very much more complicated situations. It has been difficult to review and identify bone loss or other factors of deterioration that have increased complexity. In the primary situation we are still dealing with cases with increased complexity where the bone has collapsed, where there has been progression of deformity. It is likely that surgical outcomes over time will be worse for many patients. Lengths of stay have increased with increased wound problems, infection and dislocation rates. It will take years for the full consequences of that situation to become truly understood and there is no evidence that things have reverted to normal.
Studies have demonstrated the impact of the COVID-19 pandemic on early clinical outcomes after total joint replacement. Anecdotally we are aware of cases, listed as routine that have now presented with very much more challenging bone loss and worse bone quality. Cases that were already complex are being admitted with 18 months of inactivity and deconditioning. These patients are likely to have worse outcomes. This additional technical complexity does not take into account the dreadful experience that many of our patients have had, waiting for much longer than we would wish, in pain with restricted mobility and in isolation. A number of patients have been promised dates for surgery only to be deferred, allowing further progression of their pathological process, then requiring more complex reconstruction. Staged procedures have experienced prolonged intervals sometimes leading to acute complications such as infection, fracture and instability. Inactivity in elderly patients leads to muscle wasting that is likely to be permanent and the cause of additional morbidity and multi-system deterioration. All elective surgeons will know patients who have suffered harm as a consequence of delay. Much of this is directly COVID-19 related, but some is not: it is better seen as a consequence of an imploding system. Against that background in elective surgery, other orthopaedic patients have been managed differently. Early in the pandemic there was a situation in which some fractures that might previously have had surgery were being managed conservatively. All of this will have had negative consequences for our patient outcomes.
Green et al, detailed the experience of a high-volume elective centre (South West London Elective Orthopaedic Centre) comparing activity prior to COVID-19 with that after the first wave in 20201. They identified that patients waited longer, had an increased length of stay, more in hips than in knees, and higher in revision. They identified and described disease progression, patient deconditioning with increased pain and restricted function. There was less patient prehabilitation and education prior to surgery and patients experienced less family support and increased levels of anxiety. They also identified a surgical effect with decreased activity, all of which compromised outcomes of routine elective surgery1.
In a widely-quoted work looking at the effect of joint replacement waiting lists, the Edinburgh Group reviewed their previous article detailing that patients described their experiences waiting for joint replacement as being a situation ‘worse than death’. They reported that the COVID-19 situation had compromised this yet further2.
Unfortunately a number of our patients contracted COVID-19 while under our care. Many will have suffered consequences of varied significance and some tragically died with COVID-19 related conditions. Orthopaedic surgeons will be concerned by how all this and the way it has compromised our practice and our patients is likely to be viewed within a medico-legal context.
The likely response of the law
The gist of negligence is damage: whether anyone is liable is a secondary matter. The lawyers and their clinical advisors start with the damage and then see whether it can be shown to have been caused by a breach of a duty of care. In any individual case there will be arguments about whether the patient would have done better with appropriate care, but in many cases, subjected to the various concerns detailed above, sensible experienced expert witnesses are likely to agree that they probably would have done.
Here it will be clear that there has been a failure to deliver optimal care, by a country mile in many cases. However there had been a growing assumption in the decades up to 2020 that sub-optimal care was wrong. In many cases this has never been entirely realistic. Some hospitals have traditionally attracted the best surgeons and other staff, with better resources and equipment. But in a court of law that has rarely been an effective defence for the less well-equipped general hospital. Now all that has changed utterly: sub-optimal care has become more common and the law will need to revisit the problem, being more careful in defining the limits of what is acceptable. What is the duty of care owed to the patient in a system that cannot function as it should?
The NHS has often kept patients waiting too long and the courts met this in 1980. Mr Hincks and others had been waiting far too long for hip replacement surgery because the Good Hope Hospital in Birmingham needed rebuilding. The Court of Appeal ruled that the Secretary of State’s duty to provide throughout England and Wales hospital facilities “to such extent as he considers necessary” must be qualified.
“The funds are voted by Parliament, and the Health Service has to do its best with the total allocation of financial resources.”
In words prophetic of the present situation Lord Justice Bridge identified four deficiencies beyond his reach:
“…as we all know as a matter of common sense, the health service currently falls far short of what everyone would regard as the optimum desirable standard. That is very largely a situation which is brought about by lack of resources, lack of suitable equipment, lack of suitably qualified personnel and above all lack of adequate finance.
“I feel extremely sorry for the particular applicants in this case who have had to wait a long time, not being emergency patients, for necessary surgery. They share that misfortune with thousands up and down the country. I only hope they have not been encouraged to think that these proceedings offered any real prospects that this court could enhance the standards of the National Health Service, because any such encouragement would be based upon manifest illusion.”3
That judgement set the tone for all subsequent applications to the court for judicial review of treatment decisions. The court will not direct the Secretary of State to provide a better financed health service and individual applicants have tried to show that resources were distributed irrationally to their detriment. A failure to finance more gender reassignment surgery was held to be a reasonable prioritisation. A failure to provide more cancer therapy to a dying child was a reasonable treatment decision.
However that does not tell us how the court would have handled an application for compensation for the extra pain a patient has suffered as a consequence of unreasonable delay. The courts will always flinch from anything that looks like usurping the function of the executive and legislature in creating policy, as it would be in telling the Secretary of State how much to spend, but that does not mean that it will not order the NHS to compensate those individuals who have suffered damage as a result of unreasonable delay.
Since 2009, the NHS Constitution has set out rights for patients, public and staff. This looks very much like a contract between the taxpaying patient and the NHS. The terms of the Constitution take care to make it clear that it does not intend to create new legally enforceable rights, but it does create unmistakeable objective yardsticks by which potential breaches can be measured.
Legal rights infringed by a virus?
In 2020 it was assumed that the law would be much more forgiving: no-one could reasonably be blamed for failing to admit patients where the failure to admit was due to the system being swamped by a highly contagious and frequently fatal virus for which we had no effective treatment. No-one could reasonably be held liable for that delay or its consequences. The nation acknowledged the NHS’s heroic failure to deliver the previous service by applauding on their doorsteps.
However, several things have changed since the lock-down. First and foremost, as those events have drifted into the memory, the courts will become more analytical in picking out precisely which delays can be shown to be due to the virus.
Second, because the Service has failed to recover: during 2022 no hospital was closed to admissions due to the virus. Delays due to that cause have elided with delays due to long term inadequacy of resource. Some is still directly attributable to the virus even after vaccinations and better treatment have made it less threatening to individuals, because there are still thousands of NHS beds diverted to the care of COVID-19 patients. Indirectly the virus still has an impact on the productivity of NHS facilities. Precautions against hospital acquired infections reduce throughput of patients. Staff have been depleted by the victims of the virus: a few have been killed or disabled, many more have been burned out or exhausted and we have increased sickness rates. Morale has been impacted by the realisation that the population who were prepared to come to their doorsteps to applaud NHS staff every Thursday evening were not led by a government that would ensure that their wages kept pace with inflation. We may be able to recruit new junior staff, but we cannot retain the experienced ones we need. All these contributions are much more softly focused.
How will a poor patient experience be viewed?
In time, long term PROMS and clinical outcomes will allow us to review things more objectively, but between now and then an increasing number of complaints will likely appear from patients who are rightly unhappy with their outcomes. It is not our purpose to debate these issues here, but the courts will have to decide which of them will provide a defence against a claim by a victim of delay. In theory, a sub-optimal service should make it harder for an individual to bring a claim: you cannot show that your damage is due to an unreasonable act or omission on the part of anyone. In reality such a proposition is a challenge to the ingenuity of the lawyers.
Can patients seek financial recompense if they felt forced to seek private care?
Many patients have sought care within the independent sector, funding expensive joint replacement surgery themselves. It is possible that such patients could seek financial compensation when they feel that they have had to seek self-funded independent care. Generally the NHS cannot be forced to reimburse patients for money they have spent elsewhere unless that service has been commissioned by an NHS provider.
How will a poor clinical outcome be viewed by the court?
In a claim that the NHS has failed to provide a safe or reasonable service, a patient could seek compensation for compromised fracture management, implant failures, inadequate remote reviews and increased complexity and complications of the surgery that they required. Certainly patients will seek compensation when the fractures have resulted in malunions and deformity over time if they can show that it is the consequence of a failure to provide treatment within a reasonable period of time. This will make it more important to create contemporaneous documentation of any MDT and the rationale for any delay or specific management plan. If the Trust wishes to defend an apparently unreasonable delay it must create detailed records that will withstand scrutiny, demonstrating not only that there was a lot of delay about, but that the priorities of this individual patient were recognised and carefully considered.
How will contracting COVID-19 while under our care be viewed?
Much of what we are describing stems from the fallacy of the altered perspective. At the height of the pandemic no-one could complain if they contracted COVID-19 while under our care for emergency or more routine elective treatment. As time moves on and expectations change such claims will be feasible. The difficulty is that in preparing such a defence we had to create records of what happened at a time when we did not know we would need them, or the need to defend claims was a long way down the list of priorities.
Clearly this is an area that will concern clinicians and likely provoke increased legal interest in the future. Many of the issues, while similar to existing case law will not have been tested formally in the courtroom. Only time will tell how understanding the courts will be when reviewing activity delivered by an already compromised service then dealing with an additional, unexpected and debilitating challenge.
References
- Green G, Abbott S, Vyrides Y, Afzal I, Kader D, Radha S. The impact of the COVID-19 pandemic on the length of stay following total hip and knee arthroplasty in a high volume elective orthopaedic unit. Bone Jt Open. 2021;2(8):655-60.
- Clement ND, Scott CEH, Murray JRD, Howie CR, Deehan DJ; IMPACT-Restart Collaboration. The number of patients “worse than death” while waiting for a hip or knee arthroplasty has nearly doubled during the COVID-19 pandemic. Bone Joint J. 2021;103-B(4):672-80.
- R v The Secretary of State for Social Services ex parte Alan Hinks, Marie Flemming, Marjorie Lloyd and Leslie Smith [1980] BLM 1:93.
