‘Bones, burnout, and beyond’: Strategies for supporting T&O staff and patients in a changing landscape
By Sumedh Sridhar
Fourth Year Medical Student, University of Leicester
|
This is the winning essay from the 2023 BOA Medical Student Essay Prize With the changing demographics and working practices within T&O, how can we sustain the workforce and standards of care currently provided within the NHS? |
Introduction
In recent years, trauma and orthopaedics (T&O) has experienced significant changes in patient and staff demographics, resulting in shifts in working patterns. The COVID-19 pandemic has accelerated this rate of change1, and globally, NHS staff retention rates have decreased due to issues such as staffing shortages, stress, and pay2. It is imperative that we increase our efforts to recruit and retain staff to maintain the high standards of care that the NHS has been providing for the last 75 years. Failure to do so will hinder our ability to address the healthcare challenges that will inevitably arise from changing population characteristics3.
Patient demographics
The UK's growing, ageing, and increasingly multimorbid population presents various challenges to the healthcare sector, and this trend is projected to continue4. According to the Office for National Statistics, there will be an additional 7.5 million people over the age of 65 living in the UK by 20695. Predictions from the NIHR-funded PACSim model suggest that by 2035, 67.7% of this 65+ population will be multi-morbid6. The age of onset of multi-morbidity is decreasing, with obesity and obesity-related diseases becoming more prevalent7. The average age of a major trauma patient has also significantly increased since 1990, resulting in more complicated cases due to multi-morbidity8. As a result, orthopaedic services will continue to face high demand from a population suffering from more orthopaedic pathology for a greater proportion of their lives.
To address these challenges, public health initiatives focusing on preventing obesity and increasing physical activity would have undeniable benefits for all NHS sectors. Fewer cases of preventable obesity-related orthopaedic pathology will reduce future caseloads and the prevalence of multi-morbidity. Information could be disseminated through educational campaigns in schools and workplaces, or through short informative leaflets given to patients after consultations. Additionally, initiatives aimed at preventing falls among older adults could also help reduce the number of orthopaedic injuries and fractures in this population, further reducing the burden on orthopaedic services.
Working practices
T&O staff are currently facing several challenges, including the highest number of patients waiting for treatment due to the shutdown of elective services during the pandemic9. Combined with the pension crisis and work-related stress, high burnout rates and reduced staff morale are running rampant2, with many orthopaedic consultants retiring at relatively young ages10. The 2021 British Orthopaedic Association burnout survey showed that 90% of respondents were either burnt out or at risk of burning out11. Junior staff have been particularly affected, with reduced training opportunities12 and redeployment to other specialities during COVID-1913. For some, the cancellation of career progressive exams like FRCS has made it more difficult to progress to consultancy1. Combined, these issues have led to an anticipated shortage of senior staff in the future14.
To address burnout, training programs should be implemented to help staff recognize early signs of burnout15. On-site mental health support teams would also be highly beneficial, as would fostering a more open culture within surgery when it comes to discussing burnout.
The complex economic situation of the UK means that changes to the 2016 pension-cutting tax system will be difficult to lobby. Making all medical professionals exempt from the 2016/2017 tax changes would certainly increase retention and push back the average age of retirement, as pensions would be more protected. Having more consultants would provide an irreplaceable pool of knowledge and expertise from which both trainees and patients can benefit immensely.
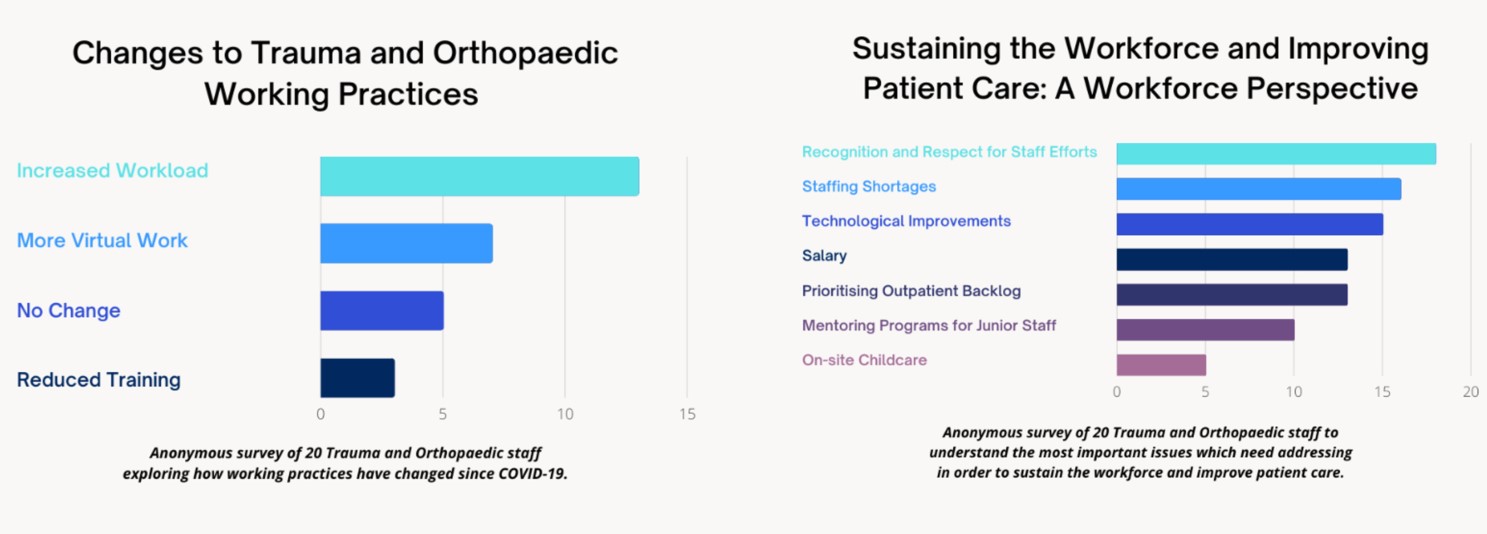
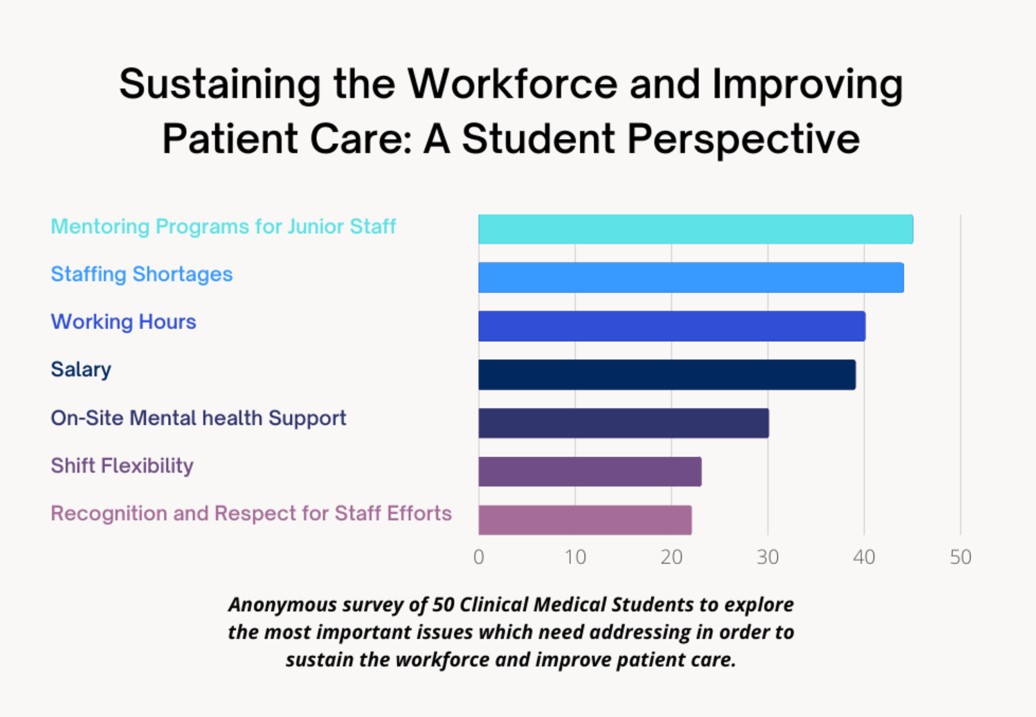
To further my understanding of the challenges practitioners face, I conducted an anonymous survey of 20 orthopaedic staff (Figure 1). The majority reported increased workload post-pandemic, but none stated working hours as an issue which needs addressing. Instead, increased recognition and respect for staff achievements was the number one issue which staff felt needed improvement. This was closely followed by staffing shortages and technological advancements to improve efficiency.
To improve recognition and respect for staff achievements, an internal NHS rewards system could be created, with financial rewards or career opportunities such as funded electives as potential incentives. More efforts should be made to improve MDT comradery, allowing members to foster a deeper understanding of their peers' difficulties and encouraging increased internal respect and recognition between all members of the team. Dedicated time within large meetings to publicly applaud the efforts of staff would certainly not go amiss.
Challenges around technology have been echoed across the country, with many staff stating that IT-related issues are holding back the full potential of hybrid MDT systems16. Utilising rapidly evolving artificial intelligence systems to diagnose and suggest solutions for IT issues faced during MDTs, and mandatory IT training for MDT staff to know how to fix commonly occurring problems could be potential solutions.
Whilst current T&O staff challenges will be at the focal point of improvements, it is equally important to look after our future staff. To investigate their views, I conducted an anonymous survey of 50 clinical medical students (Figure 2). Respondents cited mentoring programs to support junior staff, salary, working hours, and staff shortages as the most important issues to address. Seeing active change and improvement within T&O in areas expressed by staff and students will encourage medical students to join the speciality, combating the staffing shortage and improving current retention.
Conclusion
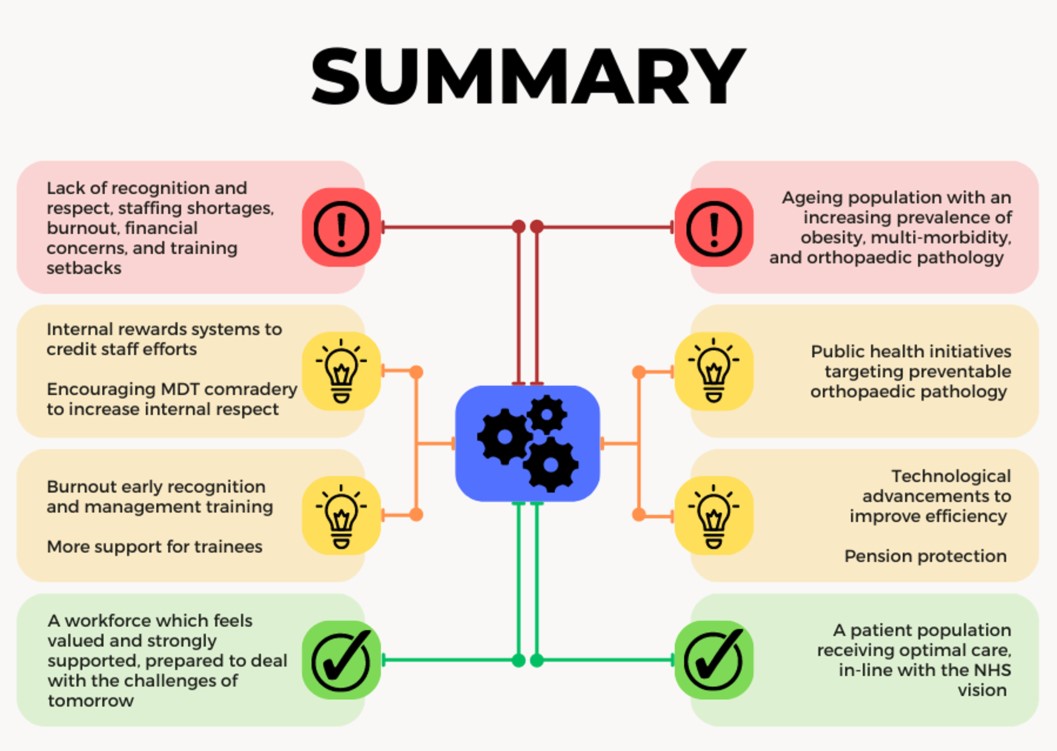
A comprehensive approach is vital to support the workforce and patients. The importance of open communication and active engagement between staff, management, and patients cannot be overstated. It is imperative that everyone's concerns are heard and addressed. While some of the challenges can only be resolved through improved funding, there are many operational changes that can have a significant impact. Prioritizing initiatives that target patient care will not only improve standards of care but also enhance staff well-being and satisfaction, resulting in better outcomes. It is crucial to ensure consistent and equitable improvements in all areas so that the workforce of today is prepared for the challenges of tomorrow. With this multi-faceted approach (Figure 3), we can sustain and improve the workforce, ultimately providing the best possible care for patients.
References
- Khan H, Williamson M, Trompeter A. The impact of the COVID-19 pandemic on orthopaedic services and training in the UK. Eur J Orthop Surg Traumatol. 2021;31(1):105-9.
- Weyman A, Glendinning R, O'hara R, Coster J, Roy D, Nolan P. Should I stay or should I go? NHS staff retention in the post COVID-19 world: Challenges and prospects. IPR Report [Internet]. 2023 [cited 2023 Feb 26]. Available from: www.bath.ac.uk/publications/should-i-stay-or-should-i-go-nhs-staff-retention-in-the-post-covid-19-world/attachments/NHS-staff-retention-IPR-report.pdf.
- Imison C, Bohmer R. Perspectives NHS and social care workforce: meeting our needs now and in the future? [Internet]. Available from: www.kingsfund.org.uk/sites/default/files/field/field_publication_file/perspectives-nhs-social-care-workforce-jul13.pdf.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37-43.
- ONS. Overview of the UK population - Office for National Statistics [Internet]. Office for National Statistics; 2021. Available from: www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021.
- Kingston A, Robinson L, Booth H, Knapp M, Jagger C. Projections of multi-morbidity in the older population in England to 2035: estimates from the Population Ageing and Care Simulation (PACSim) model. Age Ageing. 2018;47(3):374-80.
- NIHR. NIHR Evidence - Multi-morbidity predicted to increase in the UK over the next 20 years - Informative and accessible health and care research [Internet]. 2018. Available from: https://evidence.nihr.ac.uk/alert/multi-morbidity-predicted-to-increase-in-the-uk-over-the-next-20-years.
- Kehoe A, Smith JE, Edwards A, Yates D, Lecky F. The changing face of major trauma in the UK. Emerg Med J. 2015;32(12):911-5.
- NHS Eengland. Statistical Press Notice NHS referral to treatment (RTT) waiting times data March 2022 [Internet]. May 2022 [cited 2023 Feb 24]. Available from: www.england.nhs.uk/statistics/wp-content/uploads/sites/2/2022/05/Mar22-RTT-SPN-publication-version.pdf.
- BOA. Workforce Surveys [Internet]. [cited 2023 Feb 26]. Available from: www.boa.ac.uk/policy-engagement/workforce-surveys.html#:~:text=Retirement%20Intentions&text=This%20is%20most%20pronounced%20in.
- BOA. BOA Burnout and Wellbeing Survey Infographic and Results: time for a culture change? [Internet]. www.boa.ac.uk. [cited 2023 Feb 26]. Available from: www.boa.ac.uk/resources/boa-burnout-and-wellbeing-survey-infographic-and-results-time-for-a-culture-change.html.
- Bodansky D, Thornton L, Sargazi N, Philpott M, Davies R, Banks J. Impact of COVID-19 on UK orthopaedic training. The Bulletin of the Royal College of Surgeons of England. 2021;103(1):38-42.
- Dattani R, Morgan C, Li L, Bennett-Brown K, Wharton RMH. The impact of COVID-19 on the future of orthopaedic training in the UK. Acta Orthop. 2020;91(6):627-32.
- Written evidence submitted by The British Orthopaedic Association (CBP0008) [Internet]. 2021 [cited 2023 Feb 24]. Available from: https://committees.parliament.uk/writtenevidence/38332/pdf/.
- Winter G. How other professions cope with burnout. The Bulletin of the Royal College of Surgeons of England. 2020;102(6):252-5.
- Soukup T, Winters D, Chua K, Rowland P, Moneke J, Skolarus TA, et al. Evaluation of changes to work patterns in multidisciplinary cancer team meetings due to the COVID ‐19 pandemic: A national mixed‐method survey study. Cancer Med. 2023;12(7):8729-41.
