Changing perceptions during the COVID-19 pandemic peak in the UK
By Thomas Collins and Anand Pillai
Trauma & Orthopaedics, Wythenshawe Hospital, Manchester, UK
Corresponding author e-mail: [email protected]
Published 28 July 2020
Introduction
The emergence of the COVID-19 pandemic has had a significant impact on the daily life of people throughout the UK and indeed the world. The crisis is constantly evolving, with advice from the government adapting in response in an attempt to minimise its spread and prevent the NHS from being overwhelmed.
To facilitate this, there is a need for us to work using innovative methods to maintain high standards of patient care whilst complying with government guidance to socially distance and reduce hospital footfall. As is often the case with new practices, there can be a transition period during which time staff and patient apprehension can be prevalent. The fact that these new methods of patient care have developed and adapted so quickly to the threat from COVID-19, only lends credence to this point. The BMA have recently conducted a survey looking at the impact of COVID-19 on doctors1, however, to our knowledge a similar study has not been performed with patients.
The aim of this study was to assess patients’ concerns regarding COVID-19 and how they changed over time in response to changes put in place by the Trauma and Orthopaedics Outpatient Department (OPD) on a background of fluctuating infection and death rates (Figure 6) and reactive government announcements (Figure 7).
Method
We performed a prospective, cohort study of OPD attendees. Patients were asked to complete a questionnaire following their outpatient clinic appointments. Data collection took place between the 6th and 28th May and was prospective. Responses were collated and analysed for trends.
Patients were asked:
1. If they were worried about COVID-19.
2. If they felt at risk of contracting COVID-19 from their hospital visit.
3. If staff wore personal protective equipment (PPE) during their appointment.
4. What their preference was between a telephone, video or face-to-face consultation.
Results
153 questionnaires were completed. The percentage of patients worried about COVID-19 reduced throughout the 23-day collection period, (Figures 1a and 1b).
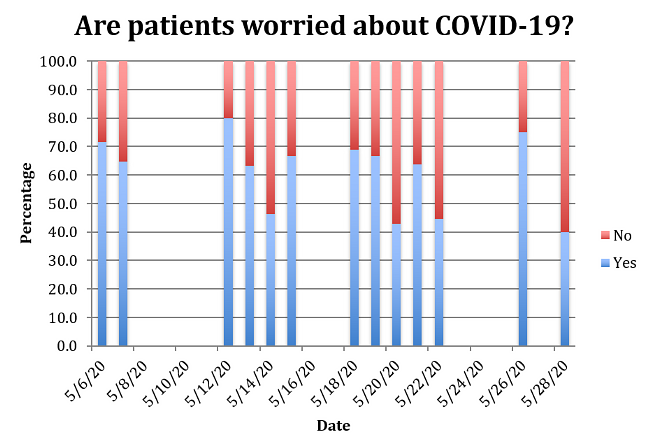
Figure 1a
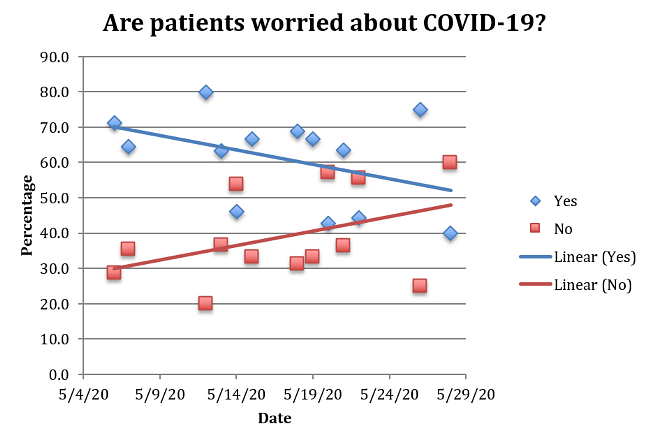
Figure 1b
The percentage of patients who believed they were able to comply with social distancing measures (>2 metres) in all areas of the outpatient department increased throughout the 23-day collection period. The percentage of patients who believed they were unable to comply with social distancing measures in one or all areas reduced throughout the same period. These findings can be seen in Figures 2a and 2b.
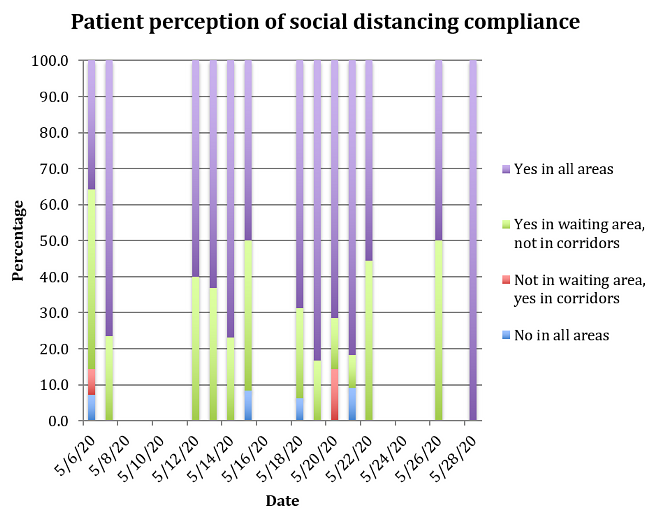
Figure 2a
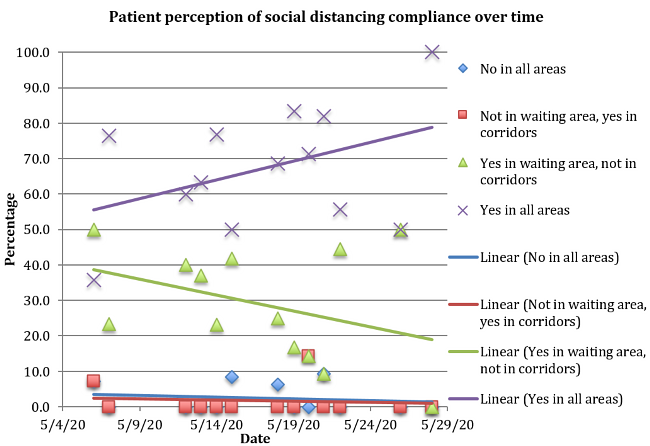
Figure 2b
The percentage of patients who perceived most staff in the outpatient area to be wearing PPE increased over time. The percentage of patients who perceived no staff, some staff or all staff to be wearing PPE reduced over time (Figures 3a and 3b).
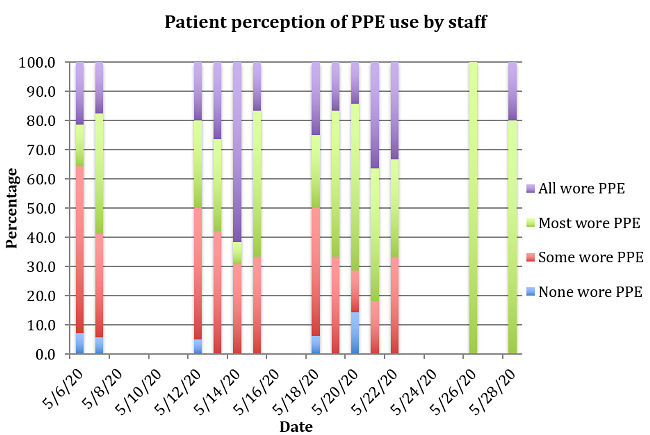
Figure 3a
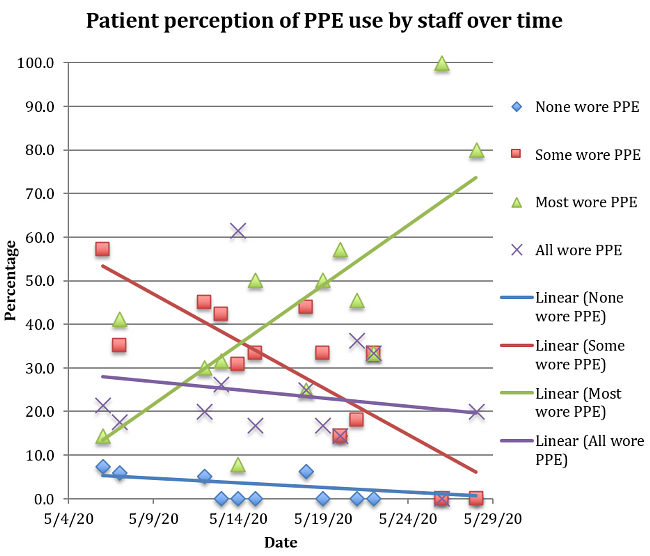
Figure 3b
The percentage of patients who felt there was no risk to them of contracting COVID-19 from their outpatient appointment increased over time. The percentage of patients who felt they were very at risk from COVID-19 also increased with time, however, this increase was marginal as can be seen by the trend line on Figure 4b. The percentage of patients who felt they were at little of moderate risk from COVID-19 reduced with time, (Figures 4a and 4b).
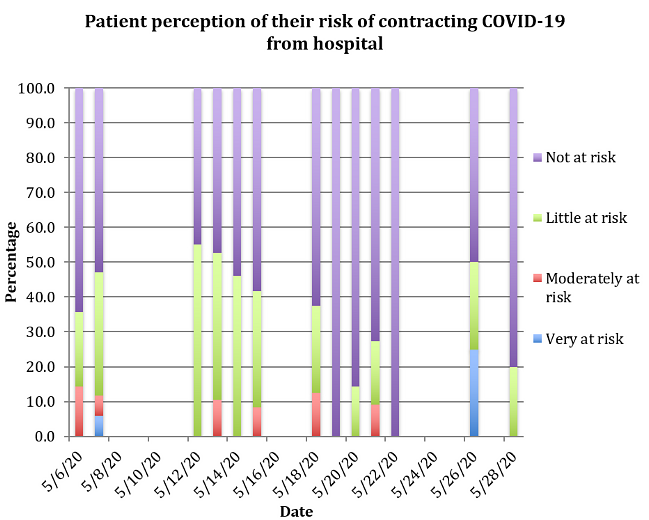
Figure 4a
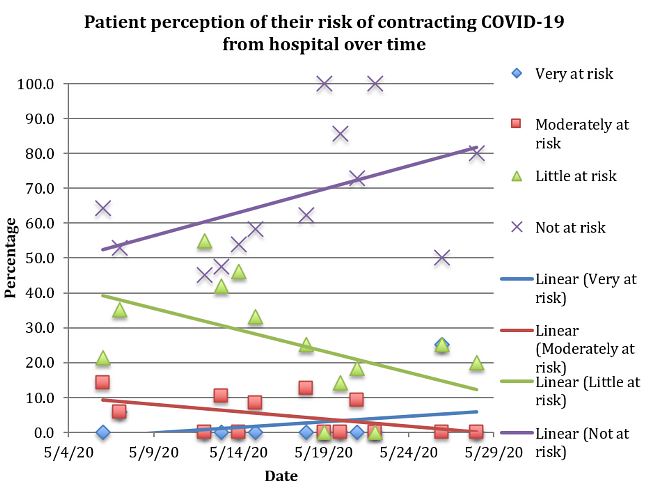
Figure 4b
Throughout the 23-day collection period patients consistently reported that given the choice they would prefer a face-to-face appointment to a video or telephone consultation, (Figure 5).
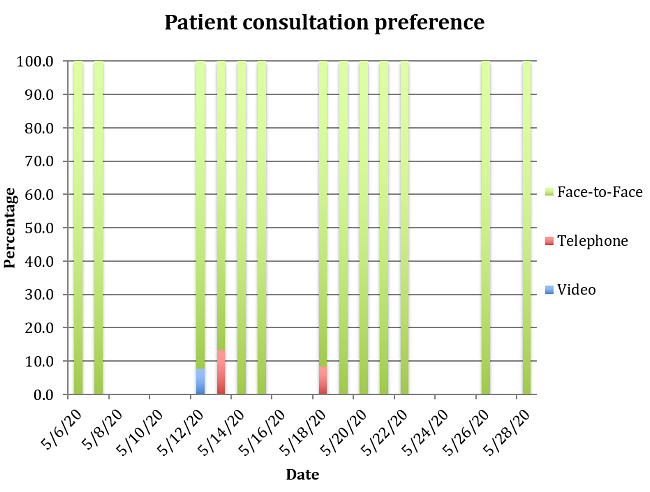
Figure 5
Discussion
There were two factors OPD staff had the power to change that could influence a patients’ perception of risk from COVID-19, namely, adherence to PPE and measures to ensure social distancing compliance by patients.
Mandatory use of surgical masks within all hospital areas was not declared by the government until 15th June, after the data collection period of this study ended, (Figure 7). However, staff were encouraged and advised to wear PPE from the beginning of the pandemic.
During our data collection the waiting area layout was changed on 18th May from patients being allowed to sit in every third seat on skipped rows, to replacement of the rows with individual chairs placed with a two metre radius from each other. Following this change the percentage of patients who felt they were able to comply with social distancing in all areas increased, (Figures 2a and 2b). This suggests that this change contributed to patients being able to maintain social distancing within the OPD.
62.07% of hospital doctors would like there to be more delivery of patient care remotely, while 42.37% would like there to be more limitation on capacity in clinical areas1. These are the same changes we made to our OPD. The results from our study show that as patients’ perception of staff PPE compliance and their own ability to comply with social distancing measures improved through time, their perception of risk of contracting COVID-19 decreased. It is our contention that the combination of the social distancing measures and PPE use led to reduction of patients’ perception of risk from COVID-19.
It is interesting to compare the feelings of risk from COVID-19 between staff (from the BMA survey in mid-June1) and patients in our study. 39.73% of hospital staff felt 'fully' protected from COVID-19, while 62.1% of our patients felt no risk (across the whole 23-day study). Our lowest percentage of patients who felt no risk was 45.0% (on 12th May), which is still higher than the staff figure. Reasons for this are debatable, however, it is reasonable to assume that increased staff awareness of potential COVID-19 outcomes is a significant factor.
Interestingly, despite general worry and feelings of risk from COVID-19, especially earlier in the data collection period (as seen in Figures 1a, 1b, 4a and 4b), patients almost unanimously preferred face-to-face consultations to video or telephone appointments (Figure 5). This suggests that either patients were willing to accept the risks of contracting COVID-19 to ensure appropriate treatment, or to receive a preferred ‘traditional’ appointment, or that patients were not aware of the potential seriousness of COVID-19. It is important to note that there were some patients who were not suitable to video or telephone consultation. For example, requiring removal of cast or K wires, needing examination, or decisions on surgery. Patients in these categories may have been aware of this and therefore recorded face-to-face appointment as their preference.
Throughout this study there were background events that may have influenced the responses to our questionnaires, particularly the patients’ perception of personal risk of contracting COVID-19 from their appointment. These events are media reports of new cases and deaths from COVID-19 and recommendations put in place by the government off the back of these figures. A summary of new daily cases and deaths from COVID-19 can be seen in Figure 6, while a timeline of the government’s management of the crisis can be seen in Figure 7.
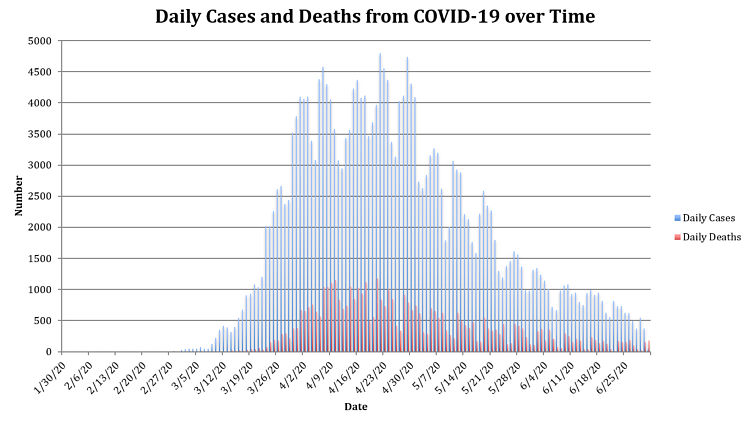
Figure 6: Bar chart showing the daily numbers of new cases and deaths from COVID-192
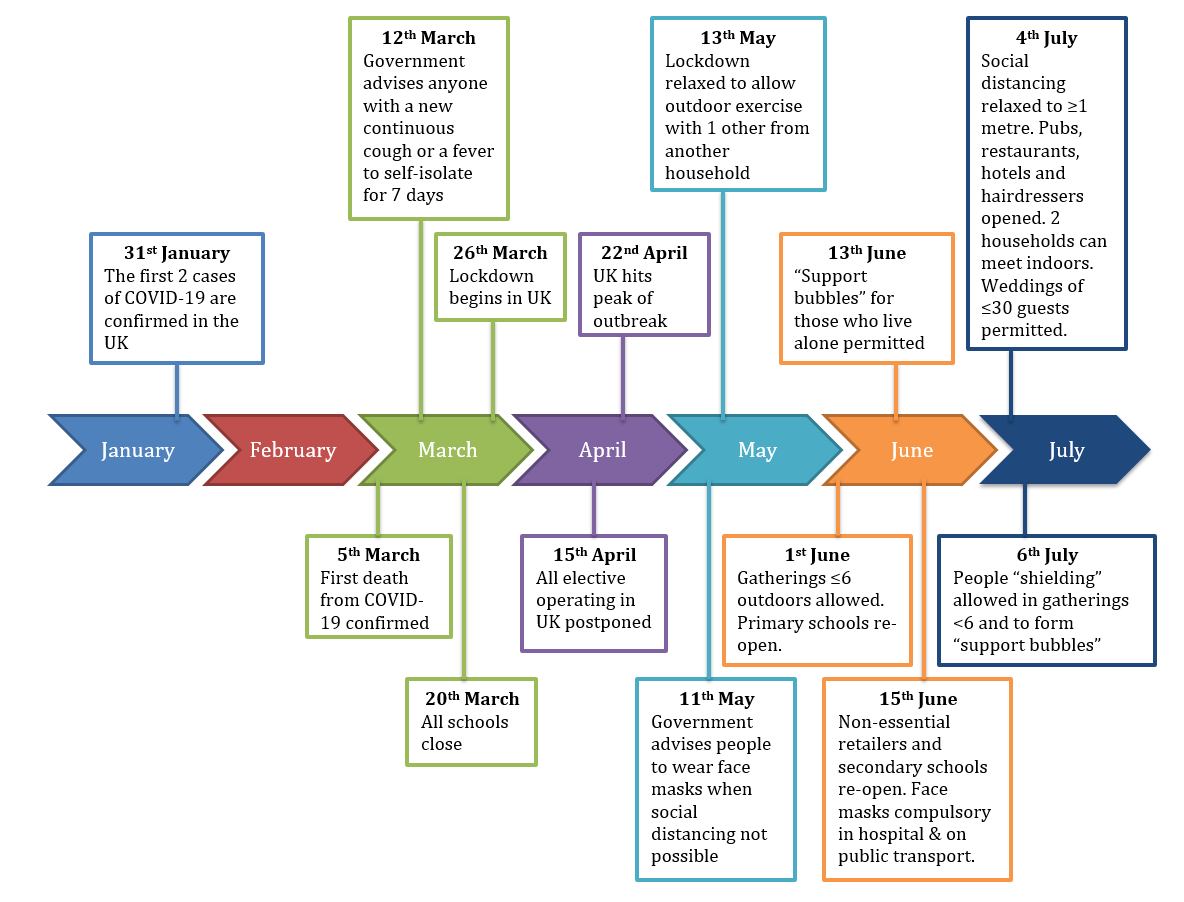
Figure 7: Timeline of Government management of COVID-193
Conclusion
Over time, patients’ general perception of risk of contracting COVID-19 during their outpatient appointment reduced. This may have been in part to the efforts made by OPD staff to facilitate social distancing and comply with PPE use. Patients overwhelmingly preferred face-to-face consultations over video or telephone consultations.
It is the hope of the authors that this study can be used as evidence that implementation of social distancing measures and PPE usage amongst all staff is beneficial in reducing the concerns of patients. This study can also be used in argument for immediate implementation of social distancing and mandatory PPE usage should a 'second wave' occur. Finally, countries in the earlier stages of the COVID-19 outbreak can use this study to inform their own OPD/hospital policies.
Following on from this study, the next decisions will be whether these new methods of delivering patient care will continue, for how long, and if this will be in conjunction with or replaced by traditional OPD practices. Figures from the BMA survey into the impact of COVID-19 on hospital doctors show that 40.35% plan to work 'more flexibly/from home more' following the pandemic1, indicating there is certainly appetite to continue remote consultation where appropriate. The determining factors will likely be whichever combination facilitates the largest number of appointments per week. Especially as the number of elective patients waiting for appointments will have been steadily increasing.
It is imperative that the efforts made during the first wave are studied so that lessons can be learnt. Differences between better performing areas and the rest of the country need to be analysed to find out why, so similar changes can be employed in worse affected areas, thereby unifying successful protocols across the NHS. Failing this we will see further instances of localised 'second waves' (such as Leicester4), and perhaps even national waves. This would truly be disastrous to the NHS, bringing it to a standstill and leading to further collateral losses.
Further to this, there must be a campaign towards promoting shared responsibility between healthcare staff and the public regarding long-term changes in healthcare delivery and infection prevention methods. There should be public education on the need for this change, as our study shows patients are still greatly in favour of face-to-face consultations. We will otherwise be unsuccessful in influencing and altering current behaviours that risk repeated outbreaks of COVID-19.
References
- BMA (2020). COVID-19: analysing the impact of coronavirus on doctors. Available at: https://www.bma.org.uk/advice-and-support/covid-19/what-the-bma-is-doing/covid-19-analysing-the-impact-of-coronavirus-on-doctors.
- GOV.UK (2020). Coronavirus (COVID-19) in the UK. Available at: https://coronavirus.data.gov.uk/#category=nations&map=case.
- Wikipedia (2020). Timeline of the COVID-19 pandemic in the United Kingdom. Available at: https://en.wikipedia.org/wiki/Timeline_of_the_COVID-19_pandemic_in_the_United_Kingdom.
- BBC News (2020). Leicester lockdown tightened as coronavirus cases rise. Available at: https://www.bbc.co.uk/news/uk-england-leicestershire-53229371.
