COVID-19: The Impact and Changes to Trauma Services in Cardiff
By KSS Dayananda, T Yasin, P Jemmett and RW TrickettCardiff and Vale University Health Board
Corresponding author email: [email protected]
Published 15 May 2020
Introduction
The Coronavirus (COVID-19) pandemic has necessitated radical changes to health and social care. Stringent measures have been put in-place and enforced by government policy. Social isolation and distancing, plus halting of all non-essential activity and travel have become essential. This was formally introduced across the UK by the British Government on 23rd March 2020. The effects of these measures and unprecedented times on trauma across Cardiff, Wales, and the UK are yet to be fully understood. How things will evolve as the country returns to its pre-lockdown state is also entirely unknown.
The management of trauma has required adjustment in light of the need to prioritise our patient’s health needs. These have been supported by updated guidelines from the BOA1. The need to adapt in order to manage this pandemic has presented challenges, and will have numerous repercussions in the management of non-COVID-19 pathology. The full impact of this will only be known retrospectively.
We discuss how the tertiary referral trauma unit and dedicated elective unit in Cardiff and Vale University Health Board (CAVUHB) made adaptations to the Trauma Services in line with recommended national guidelines.
We aim to:
- Outline the changes to our services.
- Understand the demographic of trauma during the first 4-weeks of enforced national social isolation, ‘lockdown’.
- Consider the implications on halting all elective operating and re-introduction of standard services.
Background
Cardiff and Vale University Health Board (CAVUHB) has three hospital sites: University Hospital Wales (UHW), University Hospital Llandough (UHL) and the Children’s Hospital for Wales (CHfW).
UHW is the tertiary referral trauma centre and due to imminently become the Major Trauma Centre for Wales. There is a full complement of specialties, excluding plastic surgery. A newly opened Trauma Ambulatory Care Unit (TACU) allows the treatment of ambulant trauma and co-ordination of urgent scheduled day-case trauma patients. Geographically, the UHW site also houses the stand-alone CHfW. UHL encompasses the Cardiff and Vale Orthopaedic Centre (CAVOC), a dedicated ring-fenced elective orthopaedic unit and the Day Surgery Unit (DSU) shared by all surgical specialties.
Service adjustments
In preparation for the predicted surge of COVID-19 activity, we modelled a reduction in major trauma secondary to the social isolation and distancing measures. The incidence of non-major, ambulant trauma and fragility fractures was difficult to predict. A potential increase in certain injury types, for example those following DIY or gardening endeavours, and cycling was considered. The need for maintained theatre capacity to manage these injuries whilst protecting patients and staff from cross contamination of COVID-19 would necessitate increased theatre time.
With pressing need to maintain a safe Trauma Service our local department team has swiftly reconfigured the entirety of CAVUHB Trauma Services. All elective activity was stopped on 13th March 2020. Planned elective activity (i.e. those patients with upcoming surgical or out-patient appointments) was re-triaged by the respective consultants and an assessment on urgency made. Whilst this predated subsequent advice from the Royal College of Surgeons and British Orthopaedic Association2, the method of triaging followed a similar rationale.
The trauma service has been divided across the two geographical sites: UHW/CHfW and UHL. Polytrauma and spinal injuries continue to be managed within UHW. Paediatric trauma has relocated entirely to the CHfW. All remaining trauma cases are considered for either in-patient transfer (for non-ambulant trauma) or planned day-surgery (for ambulant trauma) treatment at UHL. UHW has three dedicated COVID-19 theatres, used solely for the management of patients who have tested positive. Thus, patients with confirmed COVID-19 positive status or high suspicion of infection on clinical grounds, are managed in UHW. The long-standing dedicated trauma theatre at UHW has been kept free from COVID-19. Asymptomatic or confirmed COVID-19 negative patients are managed in UHL. This allowed a degree of segregation regarding viral status.
The novel trauma unit is based in the Day Surgery Unit in UHL. It comprises established Day Surgery functionality, along with access to in-patient dedicated trauma beds and TACU. It is segregated from the main hospital allowing for the single point of access for in-patients, and has a separate hospital entrance for ambulant patients. The TACU (previously located in UHW) has been relocated to UHL. The unit complements the day surgery unit, allowing management of ambulant trauma problems and administration of intravenous antibiotics as required.
A dual site general trauma consultant on-call rota has been made possible by the reintegration of all orthopaedic trauma consultants into the rota, providing resident, frontline senior decision making. There is a separate spinal and hand surgery on-call rota. In line with the COVID-19 workforce, all orthopaedic surgical grades have witnessed significant rota changes running a resident three day on, three day off pattern with redundancy to allow for staff sickness or self-isolation. The less experienced surgical workforce (foundation and core trainee doctors) have been redeployed to the COVID-19 workforce. Dedicated orthogeriatric consultant support is provided seven days per week in UHL, where the majority of the hip fractures are managed.
Fracture clinic services usually located in UHW have been relocated to UHL in the CAVOC Outpatients department. Patients are screened prior to admittance for symptoms and fever. This has dual purpose; it allows segregation of fracture clinic patients requiring face-to-face review to protect them, and additionally provides ED with increased capacity to allow compliance of social distancing in waiting areas and separation of suspected infected cases.
The Virtual Fracture Clinic (VFC) had been established in UHW prior to the COVID-19 pandemic. However, the pandemic has emphasised its critically important role.
Methods and materials
Analysis of our prospectively collected electronic surgical database (Bluespier) permits capture of all cases undergoing surgical intervention. Data was extracted for the first four-weeks of ‘lockdown’ from 23rd March 2020 to 19th April 2020. Retrospective review of this same database allows evaluation of trauma and orthopaedic surgery activity prior to COVID-19 with comparison to the same four-week period in 2019 (25th March 2019 to 21st April 2019).
Data concerning all patients undergoing treatment through the TACU are routinely prospectively recorded.
Retrospective review of all fracture clinic appointments allows quantification of the number of patient’s reviewed face-to-face or via the Virtual Fracture Clinic (VFC) with comparison of both time periods.
Results
Trauma surgery
Since the start of national ‘lockdown’ there has been a 48% reduction in trauma surgery compared to the same period in 2019, (see Figure 1).
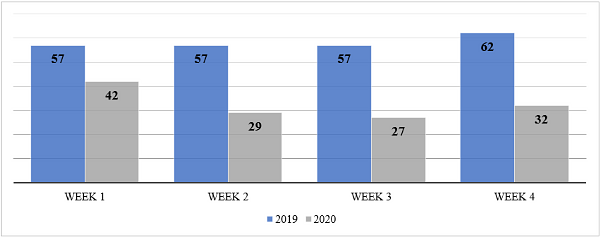
Figure 1: Number of trauma operations performed in the same 4-week period comparing 2019 and 2020.
Between 23rd March 2020 and 19th April 2020 there were 130 surgical cases for trauma performed across the CAVUHB, compared to 233 cases during the same four-week period in 2019. The mean age was 46 years (5 months to 99 years), with a male to female ratio of 1:1.28 (57 males to 73 females).
After an initial peak in surgical numbers performed during the first week, the surgical numbers have stabilised with the establishment of ‘lockdown’, (see Figure 2). This peak was secondary to a small number of urgent non-acute cases (adult n=9, paediatric n=7) who were stratified for risk by their treating consultant as unable to wait until a post-COVID service was re-established, (see Figure 3).
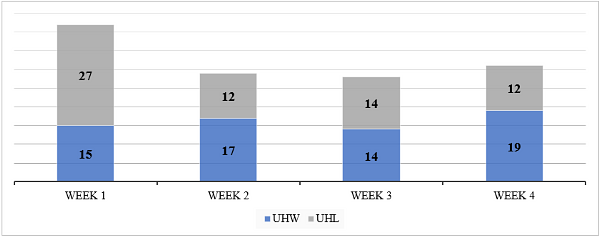
Figure 2: Surgical burden and hospital distribution by week during the first 4 weeks of ‘lockdown’.
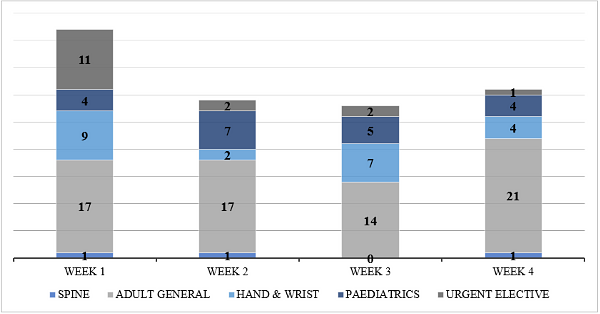
Figure 3: Trauma surgical sub-specialty distribution over the first 4-weeks of ‘lockdown’.
Injury severity was compared by classifying trauma procedures according to Table 1. The overall number of cases of major trauma has decreased, as well as the proportion relative to the overall total during ‘lockdown’ when compared with the same four-week period in 2019. However, the number / proportion of polytrauma, soft tissue injuries and NOF fractures have increased marginally, (see Figure 4).
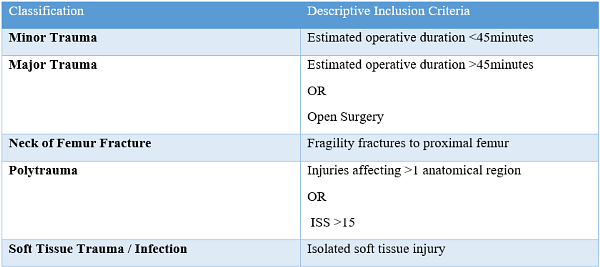
Table 1: Descriptive parameters to allow interpretation of trauma severity.
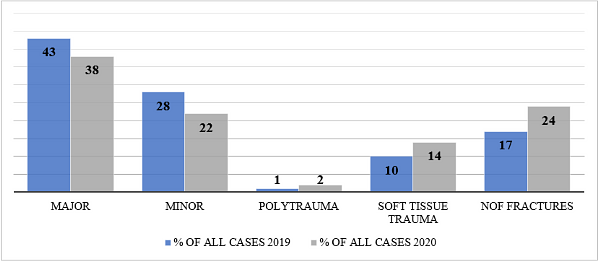
Figure 4: Comparative severity of trauma cases during ‘lockdown’ and the same month in 2019.
Day-case surgery has comprised 40% of all surgical cases and 27% have less than one week stay. Across all injury categories, the mean length of in-patient stay has been five days.
Neck of femur (NOF) fragility fractures
Hip fractures were the most common injury seen, comprising nearly a quarter of all operated cases during the first four-weeks of ‘lockdown’. Comparatively, NOF fractures accounted for a fifth of all operated trauma cases during the same four-week period in 2019. Demonstrating the expected decrease in sporting and industrial injuries, but a persistence in fragility fractures during ‘lockdown’, (see Figure 5).
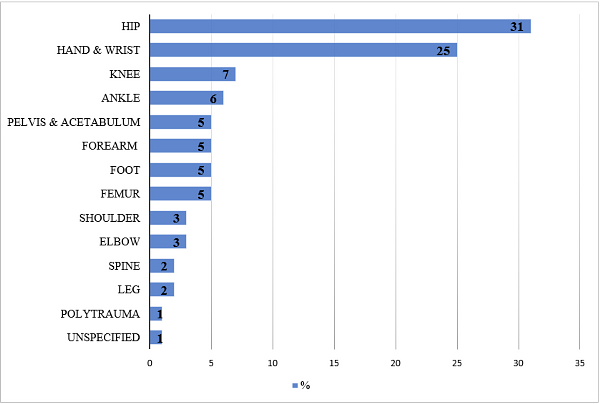
Figure 5: Trauma caseload by anatomic region during the first 4 weeks of COVID-19 ‘lockdown’.
Thirty-one patients sustained a NOF fracture during the first four-weeks ‘lockdown’, with an average age of 80 (50-99). Sixty-five percent (n=20) received their surgery at UHL, and prior to 2nd April 2020 all surgeries for NOF fractures were performed at UHL, (see Figure 6).
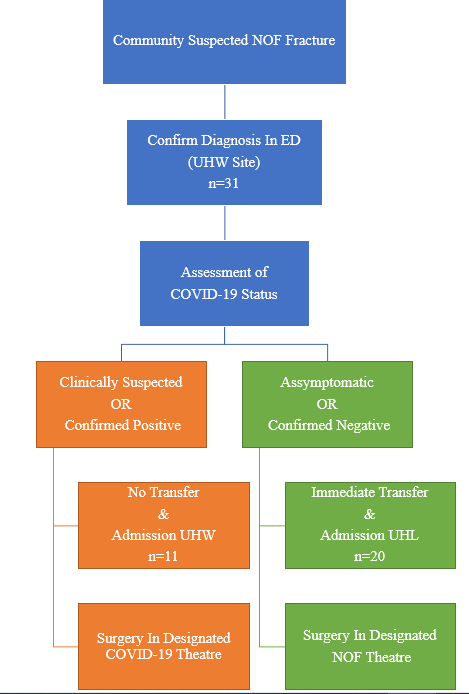
Figure 6: NOF pathway during ‘lockdown’.
Thirty-five percent (n=11) of NOF fracture patients were swabbed at some stage during their admission, of which only two returned a positive result. On average there were eight days between date of admission and the date of swab testing. Two patients were tested on the day of admission. One patient tested positive, was operated on in a COVID-19 designated theatre (UHW site) and transferred immediately to a COVID-19 designated medical ward post-operatively. The other tested negative and was operated in the usual trauma theatre and was nursed post-operatively on the trauma ward.
The average length of stay among this category of patients was 12 days (range 2-33 days), and is as expected higher than the overall average. A median number of one day was recorded between admission and surgery, maintaining compliance with NICE and BOAST guidelines4,5. Nearly 30% (n=9) received their surgery on the day of admission. Ten percent (n=3) of patients died during admission. Twenty-two percent (n=7) are currently awaiting discharge.
COVID-19 status
During the first four-weeks of ‘lockdown’ 48 patients undergoing trauma surgery were tested for COVID-19. Fourteen (29%) were performed on admission due to clinical presentation. Seven cases (5%) have subsequently returned positive swabs to date. Only two patients were positive on arrival. Five patients underwent surgery at UHW on the basis of clinical suspicion of COVID-19, whilst the remaining two developed symptoms and were tested post-operatively. Three patients have been discharged, two remain in-patient and two died during their admission.
Elective surgery
Elective orthopaedic activity was suspended on the 13th March 2020. Comparative data from 2019 shows 469 elective procedures were performed over 175 theatre sessions, (see Figure 6). Extrapolating these data suggests an elective backlog of almost 1,000 cases with two months of lost activity and 1,400 after three months. These numbers account for annual leave, cancelled sessions due to bank holidays and for departmental audit.
Trauma Ambulatory Care Unit (TACU)
There have been 48 patients treated through the TACU. All avoided the need for an in-patient admission. The majority have been for intra-venous antibiotics for superficial infections. There have been 18 minor surgical procedures through the TACU facilities, often utilising a Wide Awake, Local Anaesthetic No Tourniquet (WALANT) technique6.
Fracture clinic
The overall number of fracture clinic attendance during ‘lockdown’ has reduced by over 70% compared to the same four-week period in 2019 (2,746 in 2019, 801 in 2020).
Virtual fracture clinic (VFC) has facilitated a further reduction in face-to-face fracture clinic contacts. However, the service was not implemented in 2019, being newly introduced only a few months prior to ‘lockdown’, thus, comparative data is unavailable. During the ‘lockdown’ period, 117 patients (15%) were reviewed via VFC. The most common mechanism recorded was a non-descriptive fall (50%) followed by cycling related activities (16%). Hospital attendance for the initial consultation were avoided in 42% (n=49) by telephone discussion and directly discharging patients with a safety net contact number and remote physiotherapy where required. The most common injuries to be discharged directly were un-displaced radial head / neck fractures, (see Table 2). Forty percent of these specific injuries were sustained during cycling accidents. Distal radius fractures were the most common injury requiring a face-to-face consultation due to the need for completion of plasters and subsequent radiological monitoring of fracture position.
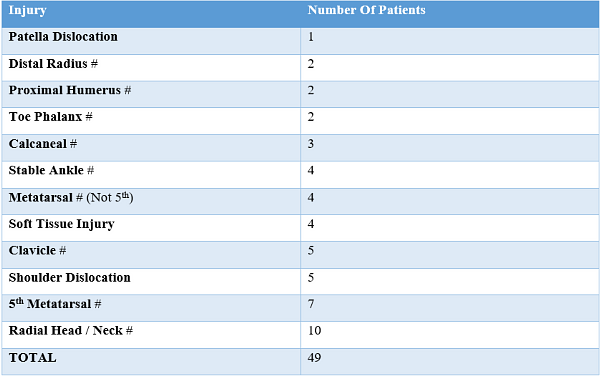
Table 2: Injuries of patients directly discharged from VFC during the first month of ‘lockdown’.
Discussion
The swift implementation of a split site trauma service at CAVUHB allowed segregation of confirmed or suspected COVID-19 cases and protection for those at highest risk of suffering serious consequences of COVID-19, namely the geriatric population with proximal femoral fractures. Containment of all paediatric cases to the CHfW (fracture clinic review and surgery) has improved the patient journey for our paediatric patients and their parents, and may also have minimised risk by segregating those considered to be ‘asymptomatic carriers’ – although this remains unknown.
Front-line trauma consultant decision making in the Emergency Department (ED) has ensured that patients spend less time within the confines of hospital and has contributed to reduced need for fracture clinic follow-up. Overall clinic attendances have reduced by >70%. Whilst this is unlikely to be sustainable in the longer term, it has demonstrated how patient contact episodes can be streamlined.
Expanding the utilisation of VFC, which has shown in various units to safe and efficient, has made a significant contribution to keeping patients safe, as well as improving efficiency7,8. Fifteen percent were reviewed via VFC and 6% of all fracture clinic patients directly discharged. Had a similar service been utilised in 2019 clinic attendances could have been reduced by over 400 patients for the considered four-week period.
The TACU has treated comparatively fewer patients during the ‘lockdown’ period compared to pre-COVID-19. This is likely a product of the reduced overall number of traumatic injuries requiring treatment. However, it remains an essential component of our service, reducing the need for in-patient admission and improving the patient experience. It has also been integral to the increased reliance on Day Surgery operating. Patients are now routinely admitted and discharged through the TACU, negating the need for even a Day Surgery trolley.
Amendments to rotas and job descriptions early on were essential for the implemented changes. The staff across the department have demonstrated flexibility and willingness throughout. Early release of the junior tiers (Foundation and Core trainees) for redeployment to the medical COVID-19 workforce strengthened CAVUHBs response to the pandemic.
Furthermore, the impact of social distancing and stringent government advice to stay at home, avoiding unnecessary activity appears to have been followed when considering the marked reduction in traumatic injuries observed during the ‘lockdown’ period.
It is difficult to predict the impact of the nation exiting ‘lockdown’. A potential surge in traumatic events as the public participate in previously restricted activities may be accompanied by a surge in COVID-19 burden. At a time where re-introduction of non-urgent activity is being discussed, it is important that the service remains flexible and able to revert to a 'war footing' at short notice.
Even if the COVID-19 pandemic allowed a swift return to non-urgent activity, there will be a significant impact on our patients. The inevitable increase in waiting times will have 3-fold implications: Prolongation of symptoms, potential progression of disease requiring more extensive or complex surgery or loss of preserving surgeries in favour of salvage only. Coupled with this, there will likely be a prolonged period of additional precautions concerning COVID-19 transmission, having a detrimental effect on out-patient and theatre efficiencies. The overall impact is impossible to predict at this stage.
A potential positive may arise from the increased non-surgical management of many injuries. Reporting the outcomes of the COVID-19 cohort may allow a better understanding of our surgical decision making. Additional service level changes – such as remote consultations and therapy services – seem likely to become the norm in the future.
Summary
Managing trauma services during these unprecedented times forces reflection and appraisal of practice. Learning and evaluating longer-term outcomes will be vital to driving change in the delivery of services to ensure improvements to hospital efficiency and patient care moving forward to a post-COVID-19 era, as well as being adequately prepared should a similar situation occur in the future.
References
- BOA (2020). Standard for Trauma and Orthopaedic (BOASTs): Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html. Accessed on: 22/04/2020
- RCS England (2020): COVID-19: Good Practice for Surgeons and Surgical Teams. April 2020. Available at: https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/covid-19-good-practice-for-surgeons-and-surgical-teams/. Accessed on: 04/05/2020.
- Benger JR, Noble SM, Coast J, Kendall JM. The Safety and Effectiveness of Minor Injuries Telemedicine. Emerg Med J. 2004;21(4):438-45.
- BOA (2019). Standard for Trauma and Orthopaedic (BOASTs): The Care of the Older or Frail Orthopaedic Trauma Patient. Available at: https://www.boa.ac.uk/resources/boast-frailty.html. Accessed on: 05/05/2020.
- NICE (2017). Hip fracture management. Clinical Guideline [CG124]. Available at: https://www.nice.org.uk/guidance/cg124.https://www.nice.org.uk/guidance/cg124/chapter/Recommendations#timing-of-surgery. Accessed on: 05/05/2020.
- Lalonde DH. Conceptual Origins, Current Practice, and Views of Wide Awake Hand Surgery. J Hand Surg Eur Vol. 2017;42(9):886-95.
- Holgate J, Kirmani S, Anand B. Virtual Fracture Clinic Delivers British Orthopaedic Association Compliance. Ann R Coll Surg Engl. 2017;99(1):51-4.
- Jenkins PJ, Gilmore A, Murray O et al. The Glasgow Fracture Pathway: a virtual clinic. BJJ News. 2014;(2):22–24. Available at: http://www.fractureclinicredesign.org/wpcontent/uploads/2013/09/BJJ-Article.pdf. Accessed on: 04/05/2020.
