Orthopaedic department staff stress in relation to COVID-19
By Katrina Bell, Niall Donaldson, Katherine Coyle and Amit Putti
Department of Trauma and Orthopaedic Surgery, Forth Valley Royal Hospital, Larbert, UK
Corresponding author e-mail: [email protected]
Published 27 August 2020
Introduction
The UK-wide ‘lockdown’ began on 23rd March 2020 and COVID-19 was the talk of the corridors and staffrooms in hospitals up and down the country. Particularly in the initial stages, there was a lot of uncertainty and misinformation, complicating matters further. There was no doubt that it was a source of stress and anxiety amongst staff, although there seemed to be great variation in the extent to which individuals were concerned. Experiencing or witnessing a stressful event is key to the development of post-traumatic stress disorder (PTSD)1. Also crucial to the diagnosis are re-experiencing the event such as nightmares (intrusion symptoms), avoiding reminders (avoidance symptoms) and hyperarousal symptoms, including problems with concentration or sleep1. The Adult Psychiatry Morbidity Survey in 2014 found that a third of adults had experienced a traumatic event and 4.4% of adults screened positive for PTSD in the past month2.
The aims of this project were to quantify staff stress levels using the Impact of Event Scale-Revised (IES-R) and to determine if any particular group experienced higher stress levels than others so that staff support resources could be appropriately allocated.
Methods
Orthopaedic staff at a district-general hospital, were surveyed between April and July 2020. Data including age, gender, occupation, the Impact of Event Scale-Revised (IES-R) and whether or not the individual worked with COVID-19 positive patients was collected. Participation was voluntary and anonymous.
The IES-R is a standardised self-reporting questionnaire to gain a subjective response to a specific traumatic event in a time frame of seven days. The Impact of Event Scale was first described by Horowitz et al. in 19793 as a scale of subjective stress related to a specific life event. It mainly assessed avoidance and intrusion symptoms. This was subsequently revised to the Impact of Event Scale-Revised (IES-R) to include hyperarousal4. The IES-R features 22 questions and is scored from 0 to 88. Scores ≥ 24 suggest a clinical concern of PTSD and scores ≥ 33 a probable diagnosis of PTSD5.
Data was analysed using descriptive and inferential statistics (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp, 2016), with p < 0.05 considered significant.
Results
60 respondents completed the questionnaire with a mean age of 35 (range 22 to 59). 48 individuals identified as female. Participants were categorised into three groups: 16 doctors; 34 nursing staff; and ten ‘other’, including allied health professionals (AHP), pharmacists and administrative staff.
Males had a mean IES-R score of 6.3 (range 0 to 24, SD 6.9). Females had a higher mean score of 19.9 (range 0 to 58, SD 15).
Occupation
The mean score for all the individuals sampled was 17.2 (range 0 to 58). Doctors, ranging from Foundation interim Year 1 (FiY1) to consultants, had a mean score of 8 (range 0 to 24, SD 7.8). Nursing staff included student nurses, healthcare support workers, staff nurses, charge nurses and nurse practitioners and had a mean score of 18.9 (range 0 to 54). The ‘other’ group had the highest mean score of 25.9 (range 0 to 58).
20 of 60 staff members had scores ≥ 24 suggesting a clinical concern of PTSD, and 10 had scores ≥ 33, indicating a probable diagnosis of PTSD. Only two of the 16 doctors had a score from 24-32, and none had a score ≥ 33. Five nurses scored from 24-32 in the clinical concern category and seven in the probable diagnosis category. The scores in the ‘other’ group were fairly equally distributed across the score categories with four in the <24 category and three in each of the 24-32 and ≥ 33 categories, (see Figure 1).
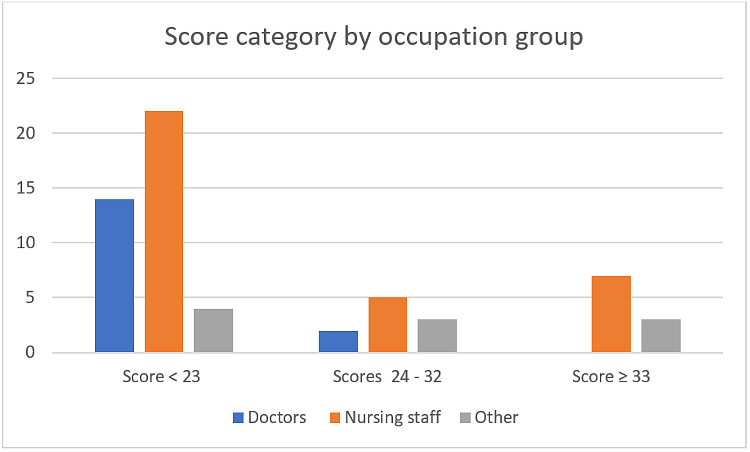
Figure 1: Score category by occupation group
Working with COVID-19 positive patients
46 of those surveyed worked with COVID-19 positive patients, with a mean score of 17.2 compared to 13.6 for the 13 who did not work with positive patients. One individual was ‘unsure’. Although those who worked with positive patients had a higher mean score, this did not reach statistical significance (p = 0.654).
Discussion
The purpose of this study was to quantify staff stress levels using the Impact of Event Scale-Revised (IES-R) and to determine if any particular group experiences higher stress levels.
This study found that those who identified as female had a higher mean score, as did nursing staff when compared to doctors. This is supported by the findings of Lai et al. Lai et al. surveyed 1,257 healthcare workers treating COVID-19-positive patients in China during January and February 20206. They used the Chinese versions of the 9-item Patient Health Questionnaire, the 7-item Generalized Anxiety Disorder scale, the 7-item Insomnia Severity Index, and the 22-item Impact of Event Scale–Revised. They found that women had higher scores than men (p < 0.01), and nurses had higher scores than physicians (p = 0.01). They did not survey staff members other than nurses or physicians.
Chew et al. surveyed 906 healthcare staff between February and April 2020 in tertiary centres in Singapore and India7. They used both the Depression Anxiety Stress Scales (DASS-21) and the Impact of Events Scale-Revised (IES-R) as well as asking about physical symptoms. The mean IES-R score was 8.29, which is lower than that of 17.2 in this study. They surveyed physicians, nurses, AHPs, technicians, clerical staff, administrators and maintenance workers but did not record whether or not they worked with COVID-19-positive patients. 20.6% of their respondents worked in roles that would not be considered to be patient facing (technicians, clerical staff, administrators and maintenance workers), something which may explain the lower mean score than in our study.
The main limitation of this study is the small sample size. Particularly in the ‘other’ category, small respondent numbers limit the interpretation and generalisability of the results.
The project has identified that a third of staff members surveyed are at risk of developing PTSD. In order to maximise participation, survey completion was anonymous. However, given that a surprisingly high number of individuals were so severely affected, it would have been useful to be able to direct affected staff to the hospital’s staff wellbeing resources.
This study quantified staff stress levels in relation to COVID-19 in our centre. However, it is difficult to draw reliable inferences on the most affected staff groups, although doctors were the least affected. Should we experience a second wave of COVID-19 the IES-R could be used to help identify staff experiencing higher levels of stress to allocate staff wellbeing resources appropriately.
References
- Sareen J. Posttraumatic Stress Disorder in Adults: Impact, Comorbidity, Risk Factors, and Treatment. Can J Psychiatry. 2014;59(9):460–7.
- Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N Engl J Med. 2017;376(25):2459–69.
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: A measure of subjective stress. Psychosom Med. 1979;41(3):209–18.
- Weiss D, Marmar C. The Impact of Event Scale—Revised. In: Wilson J, Keane T, editors. Assessing psychological trauma and PTSD. The Guilford Press; 1997. p. 399–411.
- Asukai N, Kato H, Kawamura N, Kim Y, Yamamoto K, Kishimoto J, et al. Reliability and validity of the Japanese-language version of the Impact of Event Scale-Revised (IES-R-J): Four studies of different traumatic events. J Nerv Ment Dis. 2002;190(3):175–82.
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3(3):e203976.
- Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–65.
