Orthopaedics in the developing world: ADAPTING to a new reality within the COVID-19 pandemic
By Cameron Anley, Marilize Burger, Nando Ferreira, Edward Fuzy, Rudolph G Venter and Jacques du Toit
Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, Stellenbosch University, Tygerberg Hospital, South Africa
Corresponding author email: [email protected]
Published 04 June 2020
Adaptation is the process of changing to become accustomed to a new environment. In evolutionary terms, this process occurs over many generations and millions of years. The COVID-19 pandemic has come as a Cretaceous-Paleogene extinction event, thus threatening the way in which we, as orthopaedic surgeons, have traditionally gone about our work. As an orthopaedic department within an academic hospital, we had to define our role in this crisis while maintaining a high level of patient care, continuing with pre-and post-graduate education and, most importantly, achieving a new homeostasis with regards to life and work. Apart from maintaining our orthopaedic productivity we also had to ADAPT; we had to Assist with the COVID-19 patients, play a role in Developing PPE, be Aware of our colleagues and the stressors arising from the pandemic, remain Productive with regards to research and maintain our Teaching and training program.
As South Africa is still in the process of heading towards the envisioned 60-90 day peak of the COVID-19 crisis, we have some important decisions to make. Do we merely survive and allow this to be a 'Crisis Wasted' or do we seize the 'Opportunities within the Crisis' and assist for the greater good?
Assist
In a health care system that is understaffed and overworked, it became evident that our physicians would not be able to deal with COVID-19 patients alone. Initially, orthopaedic priorities were focused on freeing up hospital bed space. This entailed the cancellation of all elective cases which were not time sensitive, more aggressively resorting to conservative treatment options and ensuring optimal theatre efficiency to minimize length of stay for individuals requiring urgent and emergency orthopaedic surgical care. As the pandemic rages and the orthopaedic patient burden has eased (partly thanks to the national lockdown that was imposed in South Africa), orthopaedic staff are increasingly being deployed to the front line: screening patients, managing COVID-19 patients in the wards, and orthopaedic residents with previous experience in Critical Care Units are being deployed to the non-COVID-19 critical care environments to optimise critical care staff availability for the COVID-19 areas.
Develop
The Stellenbosch University, Division of Orthopaedic surgery has established close collaboration with the faculty of engineering and developed an in-house additive manufacturing laboratory. The laboratory is mainly used for 3D print models of patient imaging for pre-op planning and rehearsal of surgical procedures. With the advent of the pandemic we repurposed the lab to assist with the production of important safety equipment required for the COVID-19 response.
- Prusa Visor Project
Combining an open source design for a face shield headband, designed by Joseph Prusa and made available under the Creative Commons (CC) license, with clear sheets of plastic and elastic straps, our laboratory has facilitated the '#WeFightBackCovid' in creating high quality face shields. These were distributed to healthcare workers at Tygerberg Hospital, local secondary hospitals, clinics, screening facilities and the private sector at no cost to the receiver. To date, more than 750 face shields have been distributed with production continuing until normal supply chains can catch up with the demand.
- Hands-free door openers
By adapting designs from the engineering firm Materialise NV (Leuven, Belgium), also made available under the Creative Commons (CC) license, we have produced hands-free door openers for Tygerberg Hospital high risk areas.
- Peri Intubation Containment Chamber (PICC)
Intubation has been identified as a high-risk period for clinicians in contracting COVID-19. Although intubation boxes have previously been designed, they are cumbersome and of little clinical significance in preventing airborne transmission and have thus not widely been adopted. From simple designs of portable splash screens, the idea developed to focus more on containment, and extraction of aerosols, in a simple, cost-effective solution, that utilises as much existing equipment as possible. If we achieve our goal, intubation of patients with respiratory illnesses that spread via aerosolisation will be greatly diminished and lessen the risk to everyone within the immediate environment.
Awareness
The awareness that a crisis like this is linked to many stressors goes without saying. Depending on each individual’s circumstances, these may be financial, academic, medical and/or psychological. Cognisance of these stressors is essential to create strategies that enable all members of the department, both medical and ancillary staff, from the interns to the senior consultants, to cope during this stressful time.
Never has leadership been more important. Knowing that our staff are requested to engage in high risk activities requires a structured and fair deployment plan as well as acknowledgement of individual fears and anxieties. Identifying and protecting those at increased physiological and/or physical risk goes a long way to support the orthopaedic health care worker, now armed with a stethoscope instead of the much-preferred scalpel and hammer. In addition, having mentors showing support to the staff and creating teams has been invaluable in achieving this goal in our department.
Productivity
We have experienced a significant decrease in service delivery load due to elective work being cancelled, and the national lockdown decreasing our 'bread and butter' burden of disease responsibilities, i.e. trauma and emergencies. This gave us the unique opportunity to not only aid with the COVID-19 patients but also to strengthen the other aspects of our daily responsibilities e.g. research and academic activities. To ensure that individual productivity was not lost during periods of isolation, the orthopaedic division’s research unit established a digital collaboration network, providing impetus and support for ongoing research. Most of our residents have made tremendous progress with their dedicated research assignments, required as part of the specialisation process, during this time and most will probably be able to complete this part of their training much sooner than anticipated. The orthopaedic division developed a 'Team Based' approach, which allowed residents isolation time to ensure that a mass outbreak would not incapacitate the entire department, and at the same time provide dedicated time for research and studying activities.
At the onset of the South African COVID-19 epidemic, our residents were divided into three teams, with each team consisting of a combination of junior and senior members. These teams rotate on a weekly basis between 1) being on-site, 2) being on-site and on-call for COVID-19 duties and 3) being in isolation.
- Residents on-site are responsible for the day to day activities happening as part of the normal service within the Division of Orthopaedic Surgery.
- Residents on-site and on-call for COVID-19 activities aid in the screening tents, the persons under investigation (PUI) and in the critical care areas.
- The team in isolation remain at home and avoid external contact, as part of the nationwide lockdown procedures. This not only allows for social distancing but also ensures that there is still adequate staff should a member of a team contract COVID-19 and other team members need to self-isolate. These residents each have a dedicated number and if the need arises, they can be called upon to go back to the hospital to fulfil required duties. This team’s primary responsibility in their week of isolation is to work on their research projects, whilst getting direct and timeous feedback from their supervisors, thus enabling them to make rapid progress. Secondary benefits of isolation include family time and support, and mental preparation for the inevitable tsunami of COVID-19.
Teaching
Although we find ourselves in unprecedented times, our primary aim and that of our institution, remains to continue to remain productive and to continue teaching and providing learning opportunities for both under- and postgraduate students. Academic activities had to continue but understandably had to change. Teaching activities were forced onto a digital teaching platform, firstly to keep the divisional staff in the loop whilst in isolation, and secondly to continue high quality academic teaching and a sense of normality. The division embraced Microsoft Teams and currently all our departmental academic activities including our morning handover meetings, formal weekly academic meetings, and individual tutorials are live streamed and recorded. The division also extensively make use of educational webinars, both internationally and with our local sister academic units. The orthopaedic industry contributed significantly by sponsoring numerous of these webinars, whilst mostly achieving the ultimate goal of not advertising their own products. Many of these educational modalities have shown to have added value and will be incorporated into our curriculum even after the COVID-19 pandemic has passed.
Our national examination body, the College of Medicine of South Africa (CMSA), in collaboration with university heads of departments, have changed the format of registrar exit exams to enable the final candidates to qualify in 2020 or early in 2021. Regional exams, incorporating digital platforms, case-based scenarios etc. has enabled a continuously high level of evaluation of residents.
Adaptation
Although adhering to a novel but structured approach, we are all aware that we need to be extremely fluid and adaptable in our approach. Each morning we take stock of the divisional priorities of the day via our online meeting to enable adaptation and to make sure that we can cover our duties and beyond. Ongoing communication is key to ensure consistency of high-quality orthopaedic care.
Finally, to ensure continuity of care within an ever changing Orthopaedic workforce, the division introduced a digital 'Jimmy' book (ListRunner) that captures every admitted patient in the department and allows for real time communication of management plans.
Conclusion
An important theme commonly highlighted about any crisis is looking for 'silver linings'. The COVID-19 pandemic has reiterated the importance of adaptability, collaboration, constant innovation and that ‘less can be more’. Staff cohesion has reached even greater heights and we are all reminded of why we signed up for this noble profession of serving for the greater good. The developing world is constantly understaffed and overburdened, but perhaps this pandemic has taught us to work smarter, rather than harder. Importantly, we have managed to ADAPT in order to play our role during this crisis.
When you are asked if you can do a job, tell 'em, 'Certainly I can!' Then get busy and find out how to do it. - Theodore Roosevelt
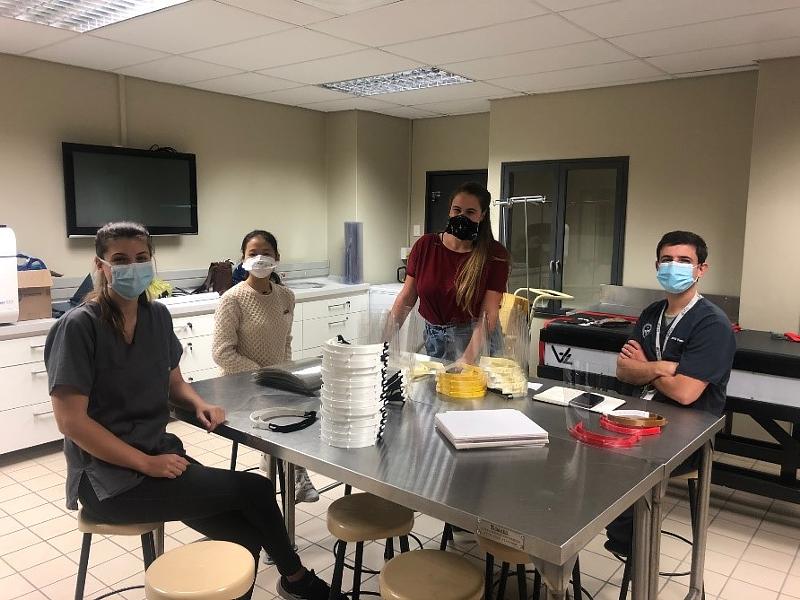
Student volunteer group '#WeFightBackCovid' with Dr Venter
