BODS/BOA Survey of impact of COVID-19 on UK orthopaedic practice and implications on restoration of elective services - Part 2
By Bhanu Mishra1, BODS Collaborators and Bibhas Roy2
1Post CCT Shoulder Fellow, Manchester University Foundation Trust
2Consultant Orthopaedic Surgeon, Manchester University Foundation Trust
We acknowledge the input of all BODS and BOA members who helped design the survey and then participated in it.
The coronavirus disease 2019 (COVID-19) outbreak has emerged as the biggest global health threat which has infected over 60 million people and claimed more than 1.5 million lives around the world. It has put significant strain on the global healthcare systems including the UK. Trauma and orthopaedic (T&O) surgery was one of the most severely affected specialties as all non-emergency surgical cases were cancelled, outpatient consultations were reconfigured, inpatient admissions minimised, and staff redeployed to medical and intensive care specialties to help treat COVID-19 patients1. Guidelines were produced by the WHO, NHS, and British Orthopaedic Association (BOA) for the treatment of orthopaedic patients during the COVID-19 pandemic2-4.
By the end of August 2020 an estimated 86,000 elective joint replacement surgery had been cancelled in the UK. Joint replacement operations are some of the most successful life-improving procedures and significant delay can lead to deterioration of physical, mental and social health5-7. When questioned, 56.8% of patients preferred to continue with planned surgical care upon resumption of elective orthopaedic services in spite of additional risks posed by COVID-198.
As we moved into phase three of the NHS response to the pandemic, NHSE provided guidance, recommendations and targets to facilitate the NHS priorities from August 2020, which included accelerating the return of non-COVID health services9. The targets in relation to recovering the maximum elective activity possible between now and winter, included an aim to achieve at least 80% of last year’s overnight electives and outpatient/day-case procedures in September, and 90% in October 20207. The targets for first outpatient appointments and follow ups, are that Trusts should be operating at 90% of usual activity in August and 100% for rest of the year. In phase three, NHSE also advised that “every patient whose planned care has been disrupted by COVID-19 receives clear communication about how they will be looked after, and who to contact in the event that their clinical circumstances change”9. NHSE outlined (1st October) the need for clinical validation of surgical waiting lists; although outlining that if this has already been undertaken during the pandemic then it does not need to be repeated10.
This paper is aimed to assess current practice against these targets, and also to evaluate the change in practice as compared to the initial evaluation which was done following the first wave (August 2020). We also address the key implications of survey findings on the restoration of elective services in future.
A second online survey of Orthopaedic Clinical Directors was conducted (First survey in August 2020), with a range of multiple choice, numerical answer, and free text questions. The form was sent to all the clinical directors via mobile and email communication on 11th November 2020 and left open for five days.
Questions addressed four broad categories:
- Current and highest work achieved since restart for elective orthopaedic practice, including day cases, joint replacement and outpatient clinics.
- Proportion of elective activity in independent sector.
- Effect of second wave on service delivery, in consideration with NHSE targets.
- Training opportunities.
These questions were considered vital to get an overall assessment of the effect of second wave on the restart, while making future predictions based on current trends.
Responses were anonymised and aggregate data analysed for each question. Due to the poor response rate from a few regions and the uncertainty as to whether these responses were representative, we have excluded them from data analysis where necessary.
The authors were satisfied that the geographical spread of responses was likely to represent the national picture in elective orthopaedic care. The regions with poor response rates have provided valuable insight into their practice even when their results are very different from the national picture and they are highlighted later in the report.
The response rate was 57% (84 of 151 Trusts). Although representatives of all four home countries (England, Wales, Scotland and Northern Ireland) were surveyed, we received only a single response from both Scotland and Northern Ireland.
Full survey results are presented below by category:
1. Current Elective Orthopaedic Work (EOW - Day Case and Elective Joint Replacement)
Table 1 and Figures 2 and 3 summarise the current EOW.
|
|
Mean (Average) |
Median |
Mode |
|
Current Day Case Rates as a % of Pre-COVID levels |
60.7% |
60 |
50 |
|
Current EJR rates as % of Pre-COVID levels |
50.4% |
55 |
0 |
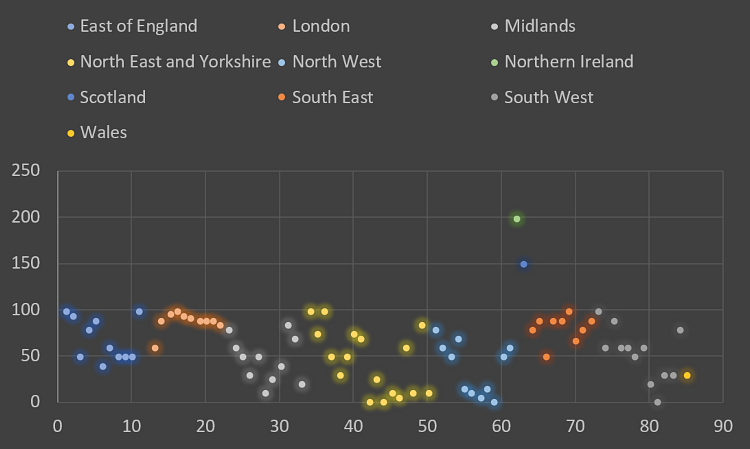
Figure 1 – Percentage of Pre-COVID day case currently being achieved.
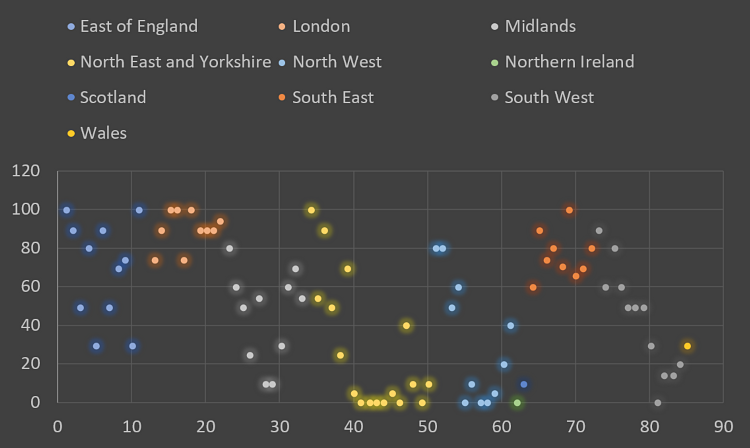
Figure 2 – Percentage of pre-COVID EJR currently being achieved.
2. Current EOW (both Day-Cases and EJR) grouped by region
The London region has the highest numbers: Day case rates are 88% and EJR rates are at 89% of Pre-COVID levels. Northern Ireland (200%) and Scotland (150%) show very high numbers for day case procedures but are unlikely to be representative as there is only one response per country (please refer to Figure 3 and 4).
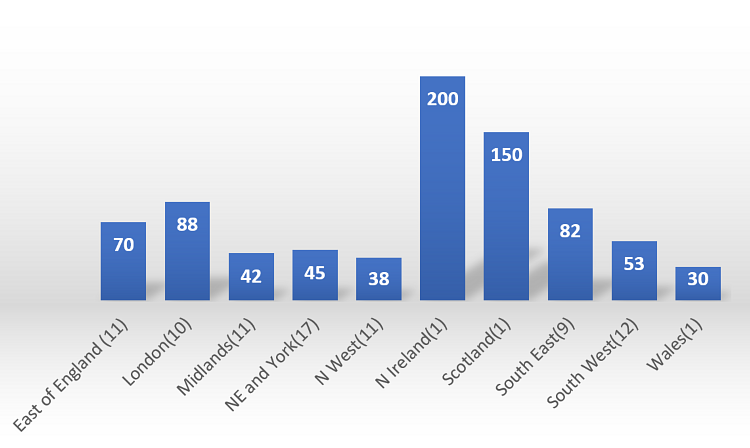
Figure 3 – Percentage of pre-COVID day case currently being achieved.
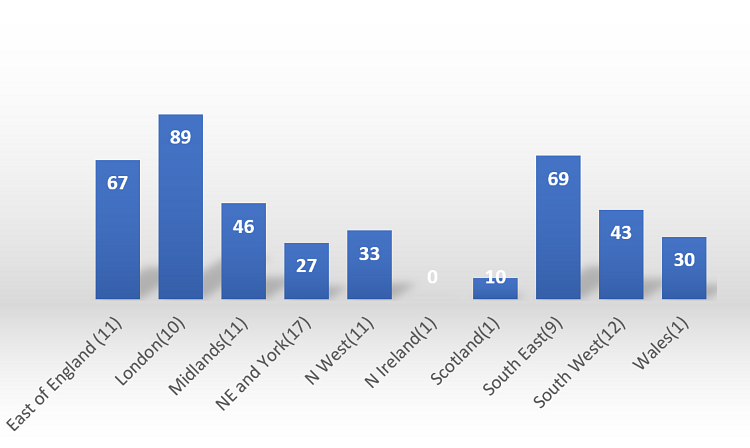
Figure 4 – Percentage of pre-COVID EJR currently being achieved (Grouped by Region).
3. Highest percentage of EOW achieved since restart (i.e., both Day-Cases and EJR)
Table 2 and Figures 5 and 6 summarises the highest percentage of EOW achieved since restart.
|
|
Mean (Average) |
Median |
Mode |
|
Highest Pre-COVID Day case |
78.7% |
80 |
100 |
|
Highest Pre-COVID EJR |
72.8% |
70 |
100 |
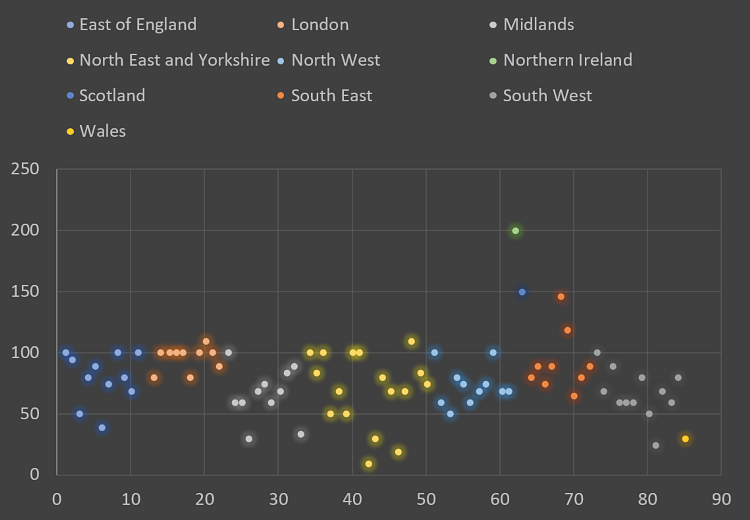
Figure 5 – Highest percentage of pre-COVID day case work achieved since restart.
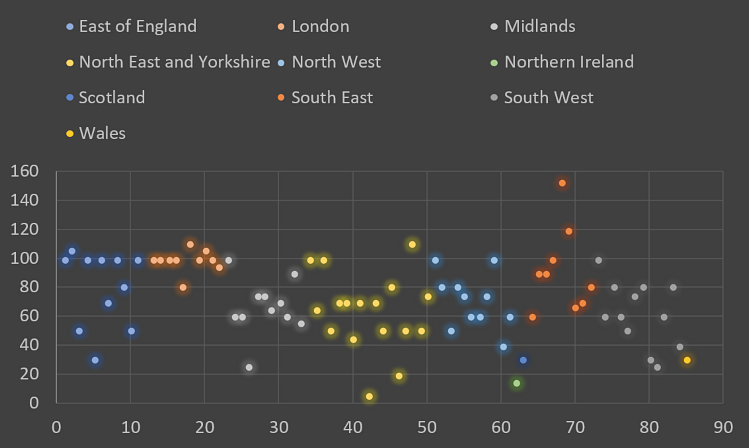
Figure 6 – Highest percentage of elective joint replacement (EJR) work achieved since restart.
4. Highest percentage of EOW (both Day-Cases and EJR) grouped by region
London again shows the highest numbers achieving 93% of pre-COVID day case numbers and 92% of pre-COVID EJR cases. Northern Ireland (200%) and Scotland (150%) again show high day case numbers but are excluded as they represent single unit numbers only. (Please refer to Figures 7 and 8).
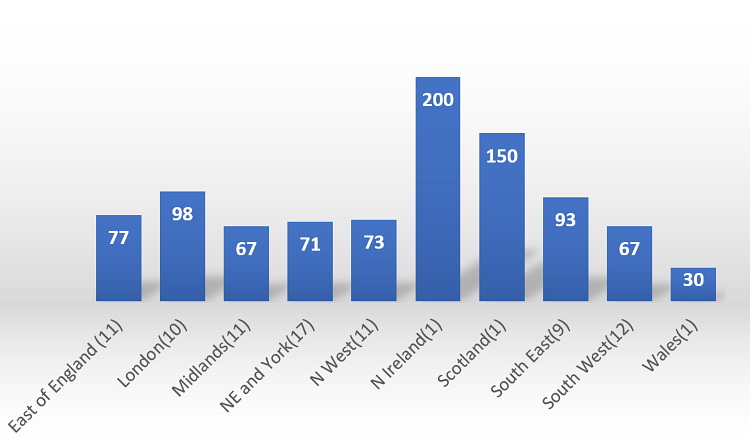
Figure 7 – Highest percentage of day case achieved since restart; grouped by region.
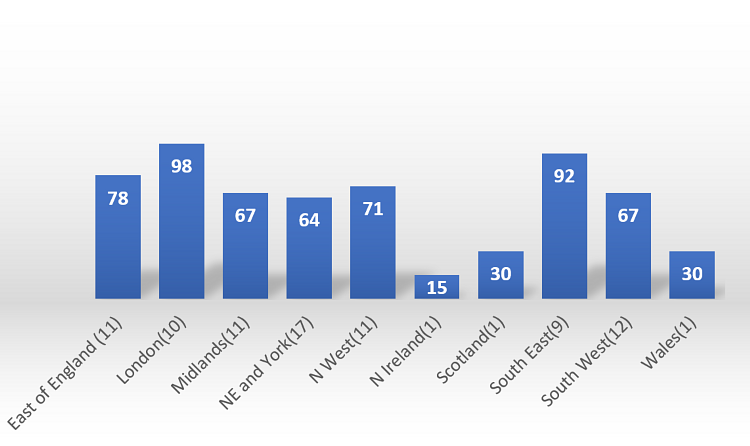
Figure 8 – Highest percentage of EJR work achieved; grouped by region.
London, South-East and East of England are the best performing regions while Wales is the only region where the current joint replacement rate albeit small, is same as the highest rate achieved. Comparison of highest vs. current percentage of EJR workloads grouped by region is shown in Figure 9.
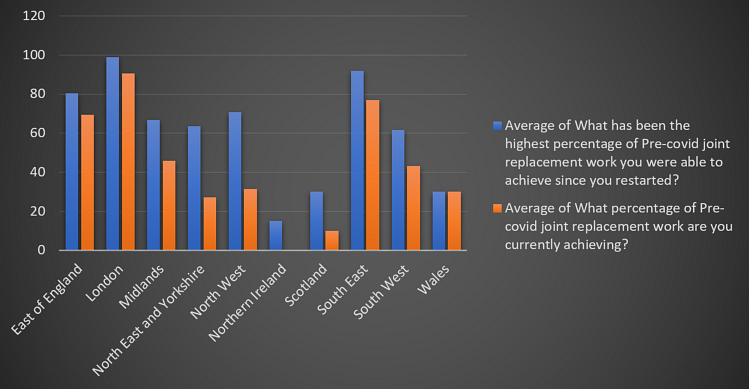
Figure 9 – Comparison of highest vs. current percentage of pre-COVID joint replacement work grouped by region.
5. Correlation of green site availability in previous survey to the rate of surgery (current EOW and highest percentage of EOW achieved since restart) measured in the current survey.
41 hospitals responded to both surveys: 12 hospitals were in Group 1 (No access to green site), 11 hospitals were in Group 2 (Plan to have access to green corridor in near future) and 18 hospital in Group 3 (Had access to green site). As noted in the graph below, the hospitals in Group 3 were among the best performing hospitals especially in terms of EJR procedures. Therefore, the ability to perform EJR is disproportionally dependent on availability of green site (please refer to Figure 10).
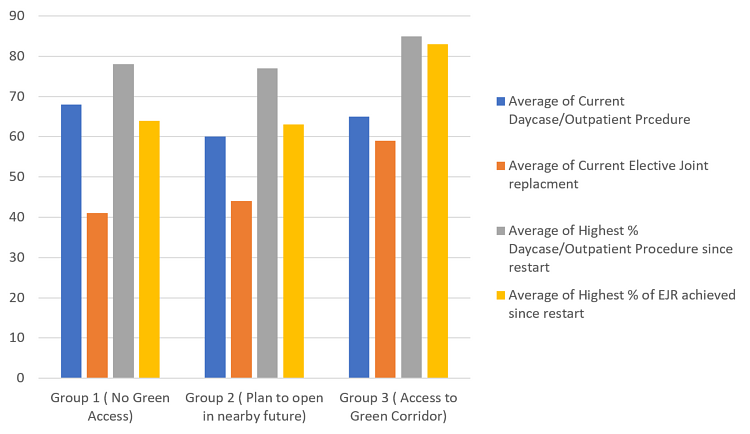
Figure 10.
6. Role of independent sector in increasing elective activity
At the national level, a mean 23% of elective activity is undertaken in the independent sector (median 15%, mode 0%). Around 36% of responders think that increased use of independent sector activity will allow increased elective activity (Figures 11 and 12).
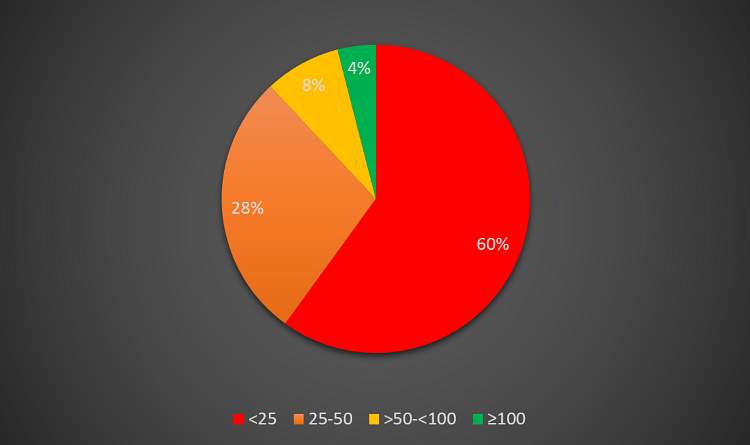
Figure 11 – Percentage of elective activity in the independent sector.
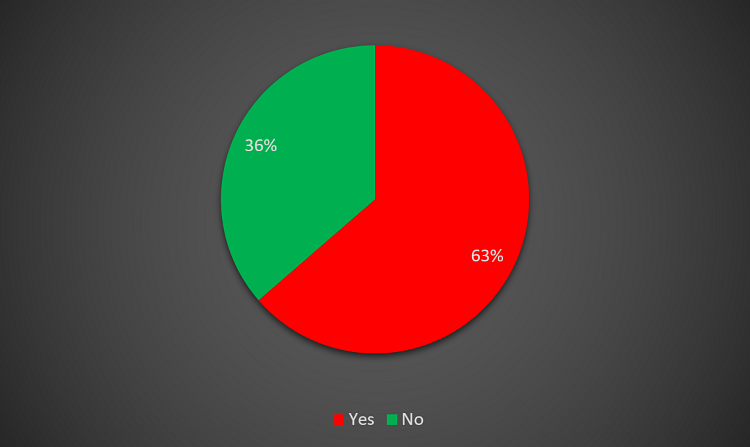
Figure 12 – Would increased use of independent sector allow increased elective activity?
7. Proportion of Elective activity in the Independent Sector
South-East region (38%) has the highest, while London (8%) has the lowest proportion of independent sector activity. Northern Ireland, Scotland and Wales are excluded from the assessment due to single centre responses (Figure 13).
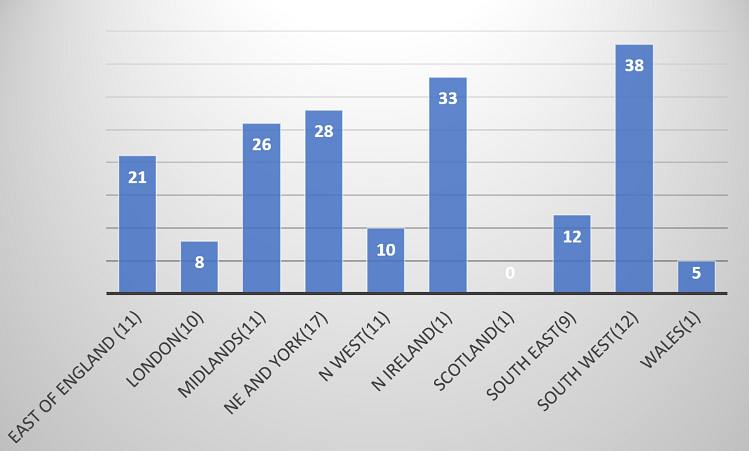
Figure 13 – Proportion of elective activity in independent sector.
8. Effect on the services due to second COVID-19 wave
58% of the responders have been affected due to second COVID-19 wave. Among these, 26% are the Trusts where all non-urgent operations have been suspended, while in 13% non-urgent operations have been reduced. 19% of Trusts stated that the planned expansion over time has stopped so that the restart targets have not been achieved (Figure 14).
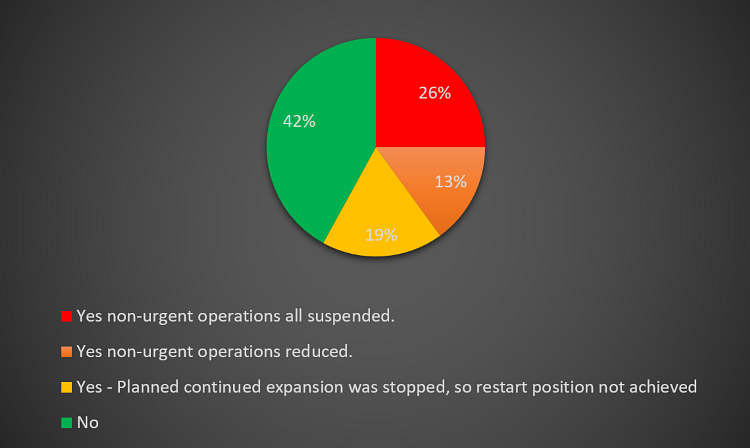
Figure 14 – Effect on services due to second COVID-19 wave.
9. NHSE Targets for Elective operations and Clinics
Only 23% of responders achieved targets for EOW and 20% of responders achieved targets for elective clinics (Figures 15 and 16).
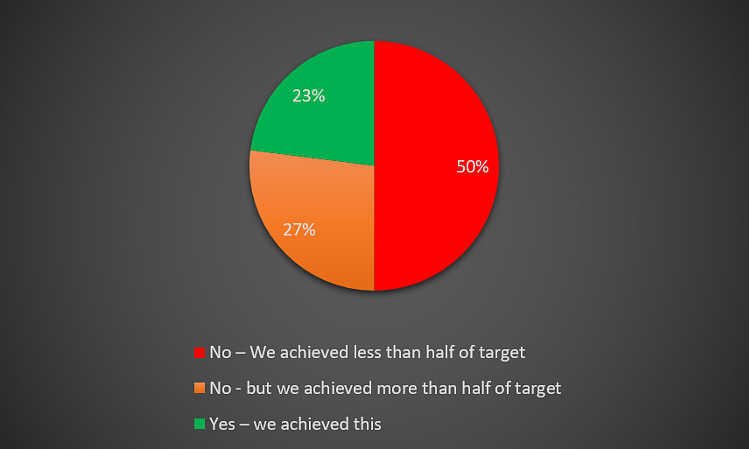
Figure 15 – NHS England targets for elective operations.
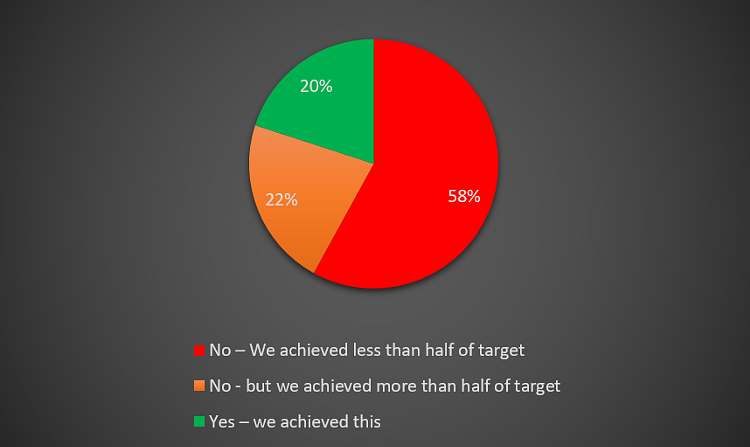
Figure 16 – NHS England targets for elective clinics.
10. Patient communication regarding planned care disruptions
43% of patients have now been contacted as opposed to 38% in the August 2020 survey. Now only 2% of have patients have received no contact as compared to 8% previously (Figures 17 and 18).
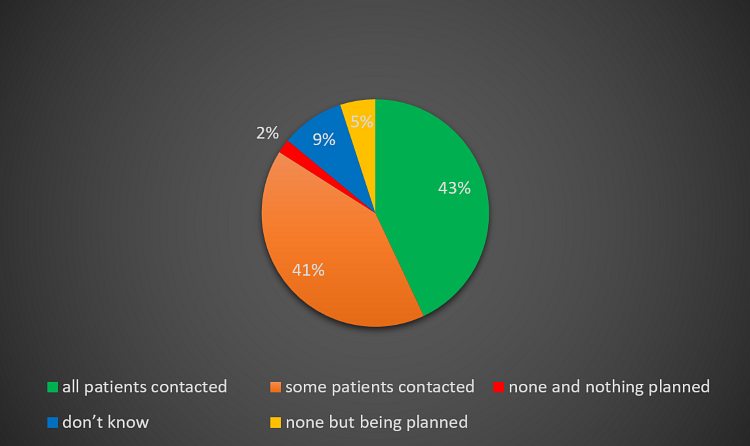
Figure 17 – Patient communication for planned care disruptions (November 2020).
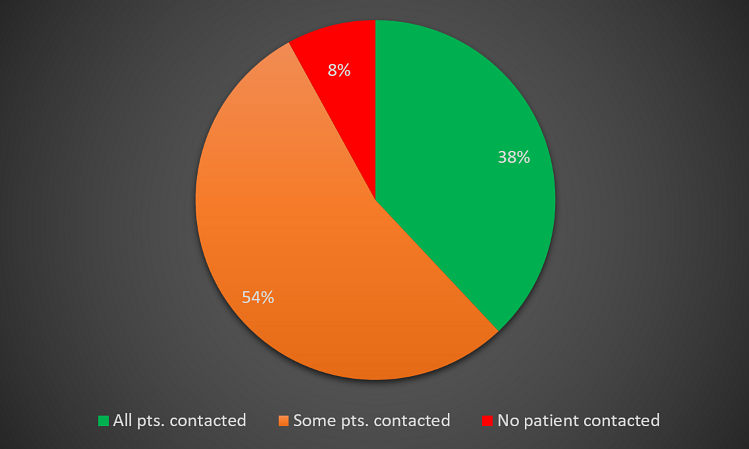
Figure 18 – Patient communication for planned care disruption (August 2020).
11. Clinical validation of waiting list
Following NHS England 1st October 2020 guidelines for clinical validation of waiting list; 48% of hospitals are fully and 43% partially validated. 9% of hospitals have not been able to validate their waiting lists.
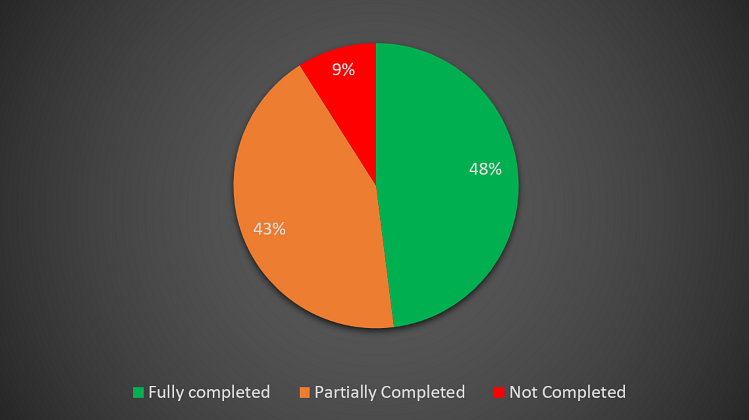
Figure 19 – Clinical validation of waiting list (percentage of total).
12. Training opportunities for junior doctors
31% of Trusts are now providing sufficient training opportunities to the juniors for EJR surgery compared to 20% in August 2020. 14% of Trusts are not able to provide any training opportunities to the juniors opposed to 18% in August 2020 (Please refer to Figures 20 and 21).
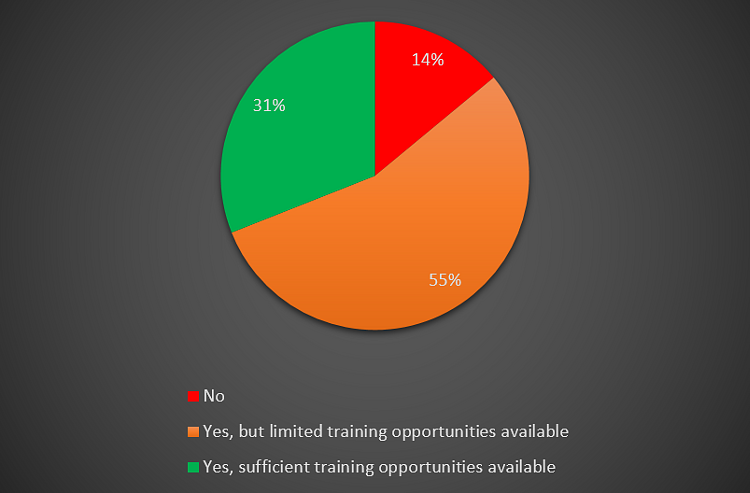
Figure 20 – Training opportunities for elective joint replacement (November 2020).
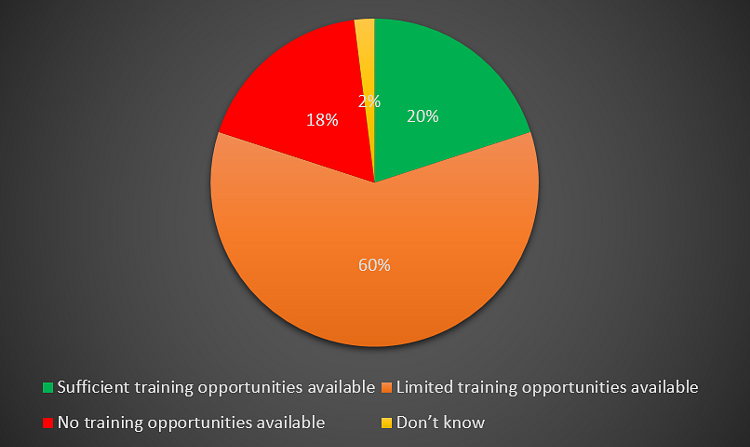
Figure 21 – Training opportunities for elective joint replacement (August 2020).
Discussion
The findings of the present survey highlight key implications of the second wave on EOW and the level of success attained by different trusts in the restart of orthopaedic practice. In our last survey we focused solely on EJR surgery as a surrogate metric to assess elective orthopaedic activity, however the present survey is more comprehensive. We obtained a better response rate of 57% this time around as compared to 37% in our previous survey. However, we received only single centre response from Scotland and Northern Ireland so the data should be used with caution if creating models of care for the entire UK.
A survey response rate of 50% or higher is considered excellent in most circumstances and is driven by high levels of motivation to complete the survey, or a strong personal relationship between business and customer11.
There is evidence in the literature regarding speed of response and survey period. The following was found in an analysis of random sample of 500,000 individual respondents12.
- 41% of responses are collected within 1 day
- 66% of responses are collected within 3 days
- 80% of responses are collected within 7 days12
In our survey we obtained 71% response on the first day and 84% within the first 24 hours, which compares well to the evidence.
The response speed and rate of the present survey implies that the survey is valid as well as representative.
The third phase of NHS response following NHS England guidance focused on accelerating the return of non-COVID-19 health services, making full use of capacity available in the window of opportunity between August and winter. The target was to reach at least 80% of their last year’s activity for both overnight electives and outpatient/day case procedures rising to 90% in October9. The majority of responders were not even close to these targets; only 23% achieved targets for elective operations and 20% for elective clinics. This correlated with our previous survey findings, where 75% of responders thought that NHSE targets were unlikely to be achieved. Even when we asked about the highest percentage of EOW achieved following the first wave, the results varied widely among centres from 0-200%. It is very difficult to explain such a varied result unless we try to look into individual hospitals for more detailed answers but one likely reason can be local lockdown imposed in the area.
The other interesting finding was that few centres have totally stopped doing inpatient elective work and have instead shifted their resources to day-case and outpatient work where they are working 1.5-2.0 times of their normal.
NHSE guidelines surrounding COVID-19 recommend that “every patient whose planned care has been disrupted by COVID-19 receives clear communication about how they will be looked after, and who to contact in the event their clinical circumstances change”9. Our current survey showed that only 43% of patients have been contacted. This shows marginal improvement as compared to previous survey where it was 38%. We believe that all trusts should now undertake measures to ensure all patients receive communication including an indication as to when their planned care will take place.
According to NHSE guidance in July 2020, “a modified national contract will be in place giving access to most independent hospital capacity until March 2021”, which was done with the view that increased use of independent sector will allow increased EOW.9 Though our survey show that 23% of the elective orthopaedic activity is in the independent sector, only 36% of the responders think that increased use of independent sector will allow increased activity. What is also interesting to note that London region which has least proportion of their elective activity in the independent sector (8%), is the region which has performed the best in terms of current elective work and the highest work attained since the restart following the first phase.
The data presents poor compliance with the NHSE guidelines. 58% respondents stated that the second wave was responsible for this failure to achieve targets. The lack of access to green sites and independent sector facilities are also important factors.
Furthermore, NHS England outlined on 1st October 202010 the requirement for all the trusts to undertake clinical validation of their waiting lists. The validation includes:
- Checking on patient’s condition and establishing any additional risk factors
- Establishing the patient’s wishes regarding treatment
- Providing good communication with patient and carer and GP
- Introducing the P5 and P6 categories that allows patients to postpone surgery but remain on the waiting lists
Utilising appropriate technology to facilitate this can help in the recovery of planned care procedures, by allowing close management and efficient coordination of waiting list, providing appropriate communication and information to patients remotely and undertaking COVID-19 risk assessment and harm reviews for patients. In our survey, 48% of hospitals fully validated, 43% partially and 9% of hospitals were not able to validate their waiting lists.
COVID-19 pandemic has affected surgical training significantly due to suspension of EOW. NHS England, Health Education England and independent sector agreed to ensure provisions and adequate indemnities were in place to enable trainees to access opportunities in independent sector10. Despite this our surveys show that this is not sufficient as only 31% of Trusts are providing sufficient training opportunities for EJR surgery which is slightly better than in our previous survey (20%).
Projected Scenario Modelling:
In order to estimate the full impact of the second wave on elective orthopaedic procedures, we modelled the most likely scenarios for the coming four months, based on 2019 elective arthroplasty NJR data12 and the current state of pandemic in the UK. In particular, we attempt to project the required levels of practice, as a percentage of 2019 practice, in order to clear the additional arthroplasty caseload generated during the pandemic. We then compared the results to our previous scenario modelling done based on our August 2020 study, to further verify our projections.
In order to do this, the following assumptions were made:
- 2019 NJR data recorded 200,434 arthroplasty cases (excluding trauma cases) – averaging 16,703 cases nationwide per month10.
- This monthly figure is used for projecting 'normal' arthroplasty practice.
- 50% of normal joint replacement work was performed in March 2020.
- No joint replacement work was performed from April-July 2020.
- 35% of normal joint replacement work was performed in August 2020 (based on estimates from previous survey).
- 72% of normal joint replacement work was performed in September 2020 (based on estimates from present survey).
- 50% of normal joint replacement work was performed each in October and November 2020 (based on estimates from present survey).
- 20% of normal joint replacement work in 2019 (1st January 2019 – 31st December 2019) was performed through waiting list initiative or extra theatre session (3rd session of the day) lists.
Scenario 1: Maximum practice from now on (1st December 2020), with no further COVID-19 related reduction in activity.
This is a rather over optimistic scenario, and is very unlikely to happen. The purpose of this scenario is to understand the pending workload which we have currently in terms of elective joint replacement which is 107,400 cases. If we operate with maximum practice from 1st December 2020 (i.e., from now on) for next 12 months then we need to operate at 154% of our pre-COVID practice to clear all the cases.
Scenario 2: Assuming the impact of second lockdown till 31st March 2020. Assumed operative caseload of 50% from Decemeber - March 2021.
This is probably the most realistic projection, based on current situation. In this scenario, an additional 140,806 cases will require arthroplasty surgery by the time normal practice is resumed in April 2021. We would therefore need to operate at 170% of pre-COVID practice for a year from April 2021 to clear all the cases.
This scenario very closely correlated with our prediction from previous survey where our calculation suggested 168% pre-COVID practice from 1st April 2021 to clear additional caseload.
Scenario 3: Same recovery as per scenario 2, but with increasing utilisation of theatre capacity by increasing to:
1. Three session list 12 hours instead of nine, on Mondays to Fridays across all facilities and adding a further two-session list on a weekend (Saturday/Sunday) (nine hours).
In this case, and with the assumption that 20% of cases had been performed on extra session lists previously, the total operative capacity could be increased by a further 27.7% from 54 to 69 hours per week. If this could be achieved, we would have to practice at 133% of 'normal' pre-COVID levels for a year from April 2021 to clear the additional caseload generated during the pandemic.
2. Three session list 12 hours instead of nine, on Mondays to Fridays across all facilities with no further increase in two session list on weekend than what was available in 2019.
Again, with the assumption that 20% of cases had been performed on extra session lists previously, the total operative capacity could be increased by further 11.1% from 54 to 60 hours per week. If this could be achieved, we would have to practice at 153% of 'normal' pre-COVID levels for a year from April 2021 to clear the additional caseload generated during pandemic.
In all modelled scenarios, the rate of practice is only to clear additional caseload generated during the pandemic and return to pre-COVID waiting list levels. However, pre-COVID levels of arthroplasty practice was not meeting demand, as demonstrated by rising waiting lists. As these models demonstrate, the NHS faces a mammoth task to deal with the increased workload generated during these unprecedented times.
This has significant social and economic implications, with joint replacements being some of the most successful life-improving procedures, allowing often otherwise healthy patients to continue working where appropriate and/or also continuing their social responsibilities, such as caring for friends and family. Beyond joint replacement surgery, it is likely that the same implications apply for other orthopaedic and non- orthopaedic planned care.
Conclusions and recommendations
We obtained a significantly better response rate in this second survey but even so we believe our data should be used with caution to create models for the entire UK orthopaedic practice. With current and pre-COVID models of care, it is difficult to expect the existing and additional new caseload of EJR surgery to be operated on in a timely fashion. NHSE targets were thought to be very demanding right from the start and have not been achieved by around 80% of the trusts. Additional resources are required to facilitate recovery. Recommendations include an increase in ring-fenced 'green' pathway elective orthopaedic facilities, regional or network collaborative models of care to facilitate maximal efficiency, and continued utilisation of independent sector facilities. Additionally, the use of cloud-based technology to facilitate care pathways and workflows across geographical boundaries will ensure, care continues to be delivered safely and independent of individual Trust-restricted systems. Realistic target-setting is essential as is honest communication with patients to set realistic expectations.
References
- Graichen H. The role of an orthopaedic surgeon in the time of Covid-19 Pandemic–a German perspective. J Orthop. 2020;19:A1–A3.
- NHS 2020. Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic. Available at: https://abcd.care/sites/abcd.care/files/site_uploads/Images/Specialty%20guide_Orthopaedic%20trauma%20and%20coronavirus_V1_16%20March.pdf. [Date last accessed 9 July 2020].
- British Orthopaedic Association (2020). Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf. [Date last accessed 9 July 2020].
- World Health Organization (2020). Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected. interim guidance. Available at: https://apps.who.int/iris/bitstream/handle/10665/330893/WHO-nCoV-Clinical-2020.3-eng.pdf?sequence=1&isAllowed=y [Date last accessed 9 July 2020].
- Zhang L, Lix LM, Ayilara O, Sawatzky R, Bohm ER. The effect of multimorbidity on changes in health-related quality of life following hip and knee arthroplasty. Bone Joint J. 2018;100-B(9):1168-74.
- Thewlis D, Bahl JS, Fraysse F, Curness K, Arnold JB, Taylor M, et al. Objectively measured 24-hour activity profiles before and after total hip arthroplasty. Bone Joint J. 2019;101-B(4):415-25.
- Scott CEH, Turnbull GS, Powell-Bowns MFR, MacDonald DJ, Breusch SJ. Activity levels and return to work after revision total hip and knee arthroplasty in patients under 65 years of age. Bone Joint J. 2018;100-B(8):1043-53.
- Chang J, Wignadasan W, Kontoghiorghe C, Kayani B, Singh S, Plastow R, et al. Restarting elective orthopaedic services during the COVID-19 pandemic. Bone & Joint Open. 2020;1(6):267-71.
- NHS England (2020). THIRD PHASE OF NHS RESPONSE TO COVID-19. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/07/20200731-Phase-3-letter-final-1.pdf.
- NHS England (2020). Clinical validation of surgical waiting lists: framework and support tools. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/10/C0760-Clinical-validation-of-surgical-waiting-lists-1-2.pdf.
- Customer Thermometer (2020). Average Survey Response Rate – What You Need to Know. Available at: https://www.customerthermometer.com/customer-surveys/average-survey-response-rate/.
- SurveyMonkey.com (2020). How many days does it take for respondents to respond to your survey?https://www.surveymonkey.com/curiosity/time-to-respond.
- NHS England (2020). Agreed principles and guidance around training in the Independent Sector for organisations working under the COVID 19 National Contract. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/09/C0730-NHSEI-and-HEE-Joint-Clinical-Trainee-Letter.pdf.
- National Joint Registry (2020). Summary of key facts about joint replacement during the 2019 calendar year. Available at: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20AR%20Summary%20key%20facts%202019.pdf.
