Congress 2025 E-Poster Abstracts

Every year the BOA Annual Congress receives a wide range of abstract submissions covering all the sub-specialty in Trauma and Orthopaedics. This year is no different with over 600+ submissions. Below is the list of selected E-Poster abstracts for this year's Annual Congress in Liverpool.
Categories
Foot & Ankle
114 - Comparison of patient reported outcomes using the Manchester-Oxford Foot Questionnaire and surgical complications following total ankle replacement in rheumatoid arthritis versus osteoarthritis
Robert Kay, Chryssa Neo, Jun Leow, John McKinley, Hisham Shalaby
Edinburgh Orthopaedics, Edinburgh, United Kingdom
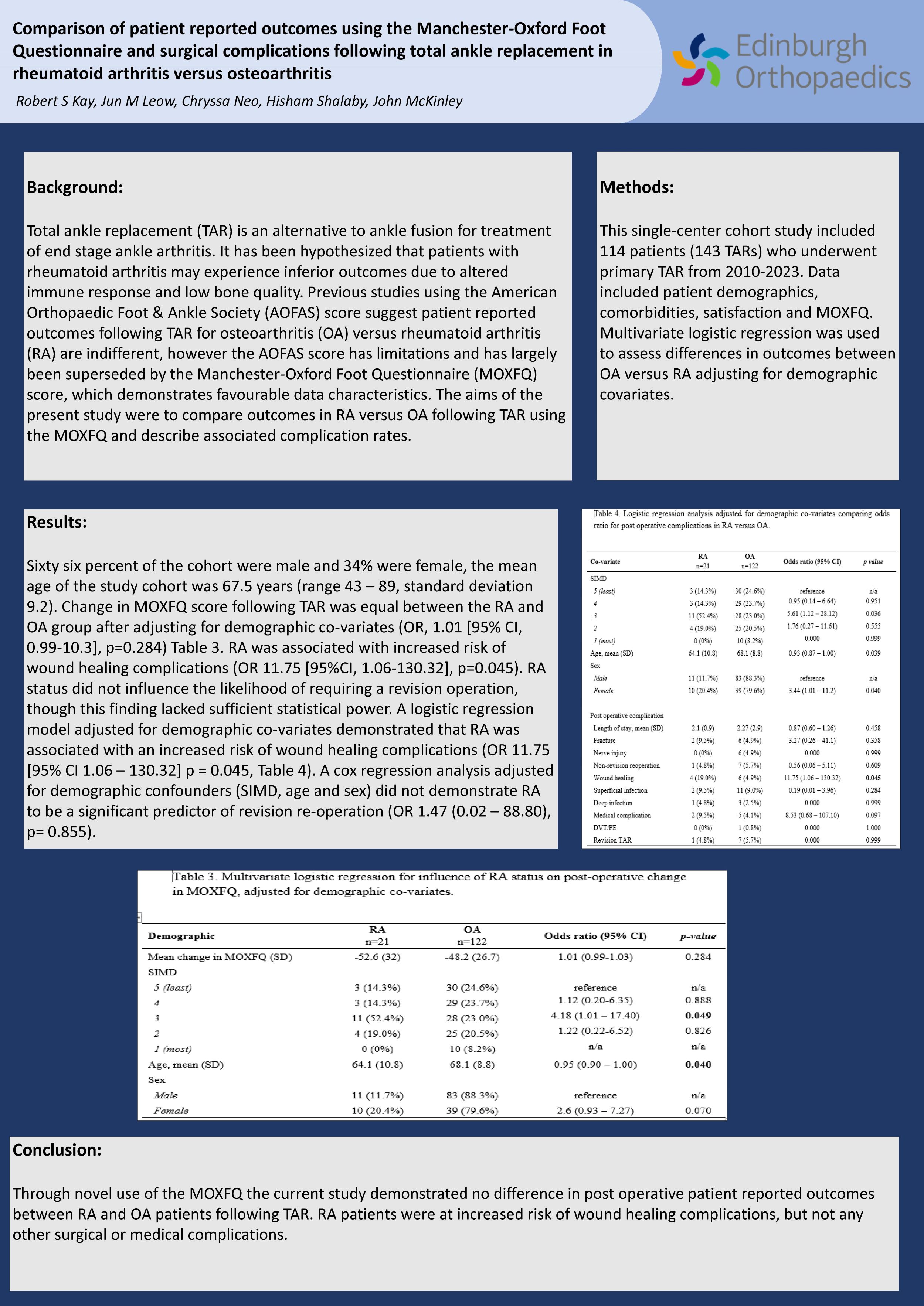
Background: Total ankle replacement (TAR) is an alternative to ankle fusion for treatment of end stage ankle arthritis. It has been hypothesised that patients with rheumatoid arthritis may experience inferior outcomes due to altered immune response and low bone quality. Previous studies using the American Orthopaedic Foot & Ankle Society (AOFAS) score suggest patient reported outcomes following TAR for osteoarthritis (OA) versus rheumatoid arthritis (RA) are indifferent, however the AOFAS score has limitations and has largely been superseded by the Manchester-Oxford Foot Questionnaire (MOXFQ) score, which demonstrates favourable data characteristics. The aims of the present study were to compare outcomes in RA versus OA following TAR using the MOXFQ and describe associated complication rates.
Methods: This single-center cohort study included 114 patients (143 TARs) who underwent primary TAR from 2010-2023. Data included patient demographics, comorbidities, satisfaction and MOXFQ. Multivariate logistic regression was used to assess differences in outcomes between OA versus RA adjusting for demographic covariates.
Results: Change in MOXFQ score following TAR was equal between the RA and OA group after adjusting for demographic co-variates (OR, 1.01 [95% CI, 0.99-10.3], p=0.284). RA was associated with increased risk of wound healing complications (OR 11.75 [95%CI, 1.06-130.32], p=0.045). RA status did not influence the likelihood of requiring a revision operation, though this finding lacked sufficient statistical power.
Conclusion: RA status was not demonstrated to significantly affect change in MOXFQ score following TAR. Wound healing complications were higher in RA patients, while other surgical and medical complications rates were equivalent.
184 - Comparison of Intra-articular Haematoma Block and Procedural Sedation for the Manipulation of Closed Ankle Fracture Dislocations: A Cross-Sectional Study
Mahmoud Elmesalmi
St George's University Hospitals NHS Foundation Trust, London, United Kingdom
Background: Ankle fracture dislocations are commonly reduced in the emergency setting under procedural sedation (PS), which requires trained clinicians and monitoring. This study aimed to evaluate the patient-reported efficacy of intra-articular haematoma block (IAHB) as an analgesic alternative to PS for the closed reduction of ankle fracture dislocations.
Methods: Data from patients with displaced ankle fractures requiring manipulation between October 2020 and April 2021 were analysed. Patients who received IAHB were compared to those who received PS. IAHB involved the injection of 10 mL of 1% lignocaine into the joint space.
Results: Twenty-eight patients received PS, and 25 received IAHB. There were no statistically significant differences in visual analogue scale (VAS) scores before, during, or after treatment (p > 0.05). First-attempt reductions were successful in 76% of IAHB patients compared to 82.1% of PS patients. IAHB was associated with lower medication costs and a shorter time to manipulation.
Conclusion: IAHB is a cost-effective and safe alternative to PS for managing ankle fracture dislocations.
437 - A Retrospective study comparing conservative treatment methods for proximal 5th metatarsal (zone 2) fractures from a Major Trauma Centre

Chiraag Pandya1, Sam Newman1, Carolyn Chadwick1, Howard Davies1, Christopher Stride2, Bobby Siddiqui1, Donatas Chlebinskas1
1Northern General Hospital, Sheffield Teaching Hospitals, Sheffield, United Kingdom. 2University of Sheffield, Sheffield, United Kingdom
Introduction: Proximal fractures of the 5th metatarsal are a common injury seen in orthopaedic fracture clinic. Zone 2 'Jones' injury have a higher risk of non-union due to the watershed area of blood supply with non-union rates documented as high as 50% with some advocating treatment with immobilisation in cast. The aim of this study was to retrospectively review all zone 2 fractures from a Major Trauma Centre and assess the difference in discharge time from clinic depending on their mode of treatment and to describe the symptomatic delayed/non-union rates seen in this cohort.
Methods: We retrospectively looked at x-rays of 5th metatarsal fractures reports as ‘base of fifth, Zone 2 or Jones fracture’ sustained between 2009 and 2022 and included those that showed a zone 2 as per the Lawrence and Bottes Classification. Online patient records were reviewed to assess mode of treatment and categorised into 4 treatment methods: cast, removable boot, foot orthosis or nothing. Weight bearing status and pertinent co-morbidities for non-union such as diabetes, smoking and steroid use were also collected.
Results: 221 zone 2 fractures were identified. Symptomatic non-union rates were 4.1% for zone 2 fractures . Cox regression survival analysis showed that no immobilisation had significantly quicker times to discharge when compared to other treatment options (Ave time to discharge 21 days, p=0.048). Diabetes increased time to discharge (p=0.048), weight bearing status had no effect on time to discharge (p=0.202)
Discussion: These results show lower non-union rates than seen in the literature however, previous literature used radiographic non-union as their end point. It is safe to treat these patient without immobilisation.
Disclosure: No conflicts to declare
Implications: This data may facilitate earlier discharge from triage clinic reducing burden on acute fracture clinic appointments.
604 - Classification of First Metatarsal Osteotomy Healing Following Minimally Invasive Hallux Valgus Surgery
Sanjana Mehrotra1, Thomas Lewis2, Jonathan Kaplan3, Tyler Gonzalez4, Sergio Morales5, Thomas Goff6, Vikramman Vignaraja7, Ayla Newton8, Robbie Ray8, Peter Lam2
1Sheffield Medical School, University of Sheffield, Sheffield, United Kingdom. 2Orthopaedics and Arthritis Specialist Centre, Sydney, Australia. 3Duke University Orthopedics, Durham, USA. 4University of South Carolina, School of Medicine, Columbia, USA. 5Orthopedic Surgery Department, Pontificia Universidad Católica de Chile, Santiago, Chile. 6Mid Yorkshire Hospitals NHS Trust, Wakefield, United Kingdom. 7King’s Foot and Ankle Unit, King’s College NHS Foundation Trust, London, United Kingdom. 8King’s Foot and Ankle Unit, King’s College Hospital NHS Foundation Trust, London, United Kingdom
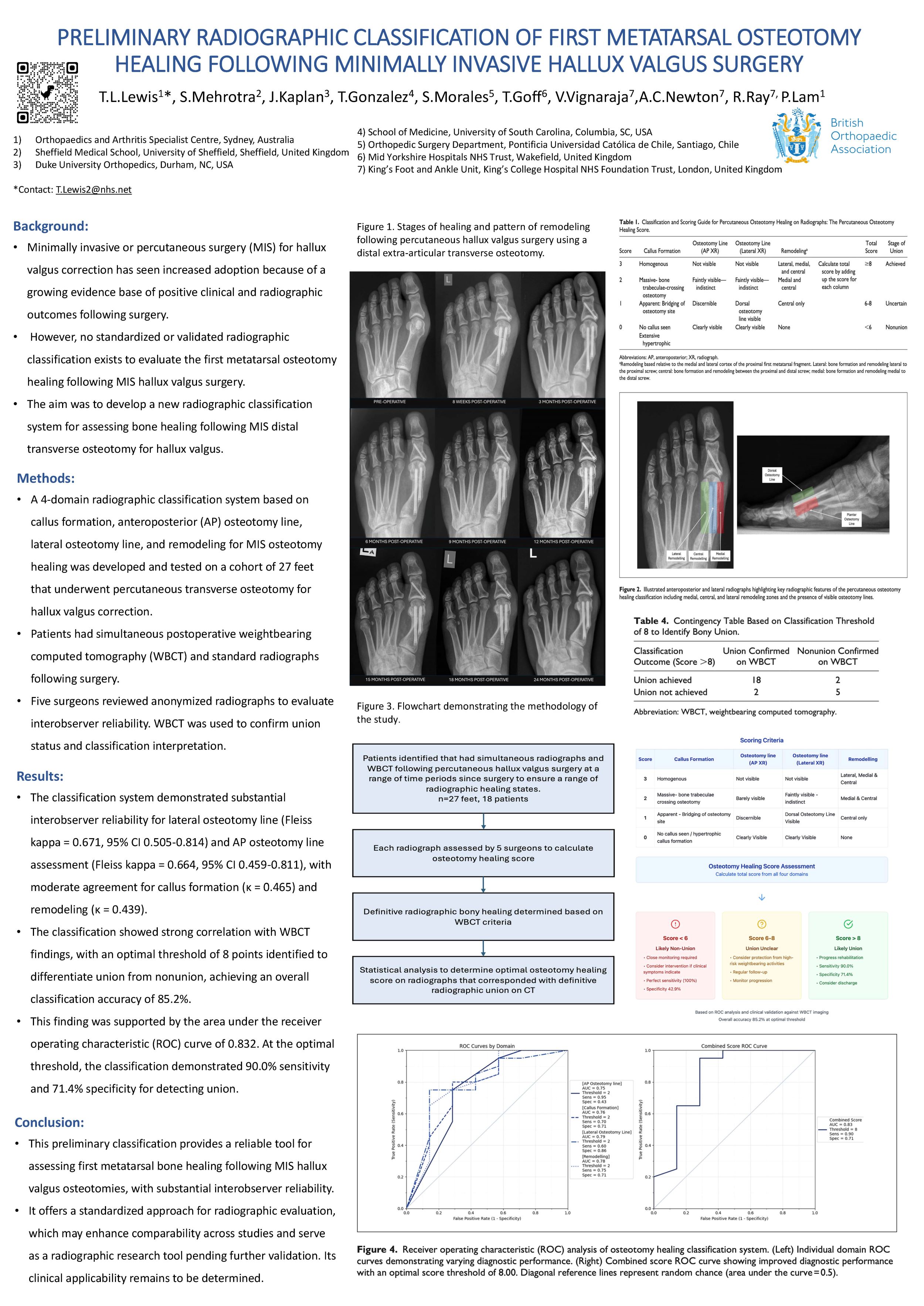
Background: Minimally invasive or percutaneous surgery (MIS) for hallux valgus correction has seen increased adoption due to a growing evidence base of positive clinical and radiographic outcomes following surgery. However, no standardised or validated radiographic classification exists to evaluate the first metatarsal osteotomy healing following MIS hallux valgus surgery. The aim was to develop a new radiographic classification system for assessing bone healing following MIS distal transverse osteotomy for hallux valgus.
Methods: A four-domain radiographic classification system based on callus formation, AP osteotomy line, lateral osteotomy line, and remodelling for MIS osteotomy healing was developed and tested on a cohort of 27 feet who underwent percutaneous transverse osteotomy for hallux valgus correction. Patients had simultaneous postoperative WBCT and standard radiographs following surgery. Five surgeons reviewed anonymized radiographs to evaluate interobserver reliability. WBCT was used to confirm union status and classification interpretation.
Results: The classification system demonstrated substantial interobserver reliability for lateral osteotomy line (Fleiss kappa = 0.671, 95% CI: 0.505-0.814) and AP osteotomy line assessment (Fleiss kappa = 0.664, 95% CI: 0.459-0.811), with moderate agreement for callus formation (κ = 0.465) and remodelling (κ = 0.439). The classification showed strong correlation with WBCT findings, with an optimal threshold of 8 points identified to differentiate union from non-union, achieving an overall classification accuracy of 85.2%. Receiver operating characteristic analysis indicated an area under the curve of 0.832. At the optimal threshold, the classification demonstrated 90.0% sensitivity and 71.4% specificity for detecting union.
Conclusion: This new classification provides a reliable tool for assessing first metatarsal bone healing following MIS hallux valgus osteotomies, with substantial interobserver reliability. It offers a standardised approach for radiographic evaluation, supporting clinical decision-making and enhancing comparability across studies.
Disclosure: No disclosures.
607 - Endoscopic Flexor Hallucis Longus Transfer With Interference Screw and Additional Tension Slide Cortical Button for Chronic Achilles Tendon Rupture
Ayla Claire Newton1, Samuel Franklin1, Thomas L Lewis1, Sanjana Mehrotra2, Vikramman Vignaraja1, Robbie Ray1
1King’s Foot and Ankle Unit, King’s College Hospital NHS Foundation Trust, London, United Kingdom. 2Sheffield Medical School, University of Sheffield, Sheffield, United Kingdom
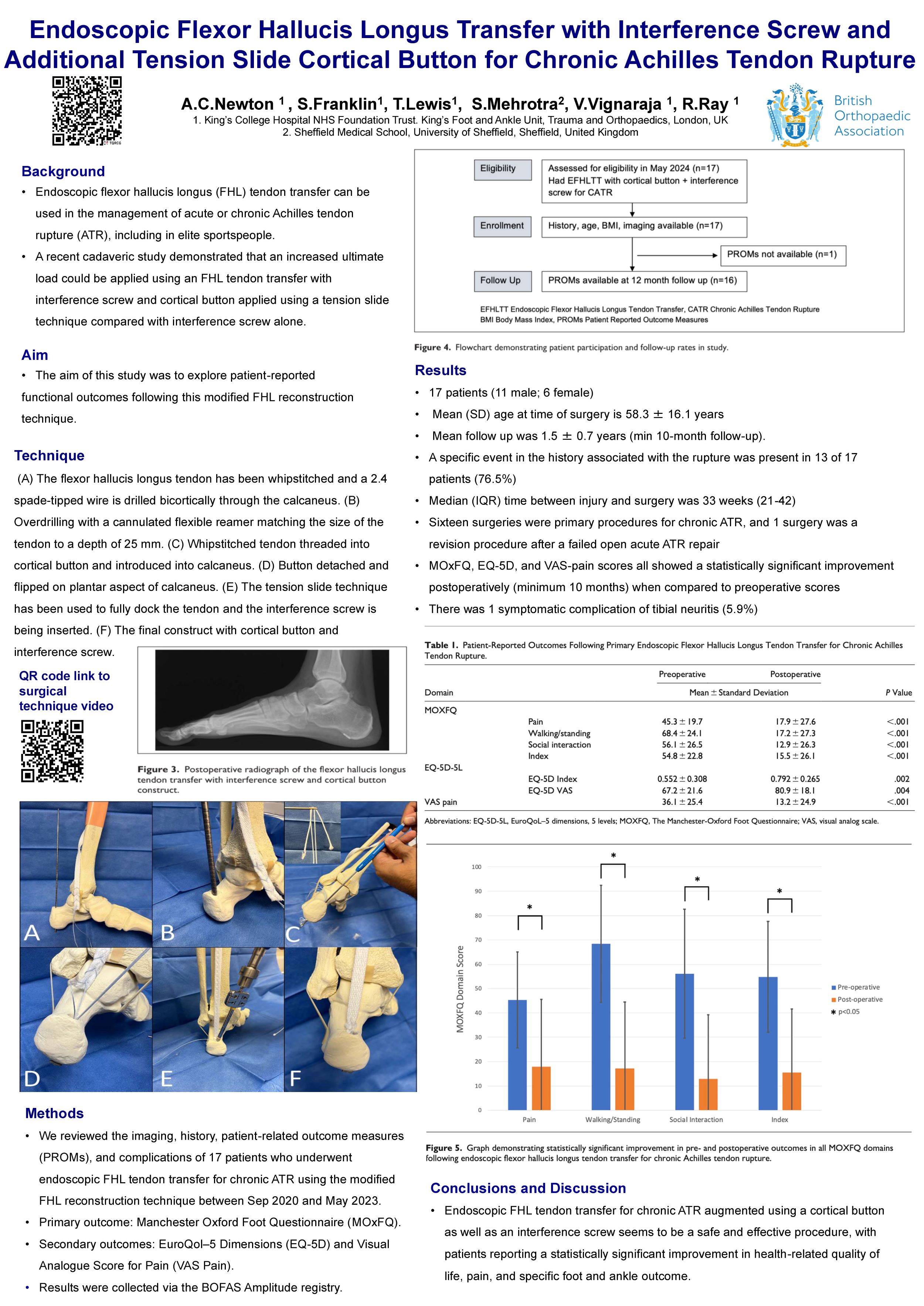
Background: Endoscopic flexor hallucis longus (FHL) tendon transfer can be used in the management of acute or chronic Achilles tendon rupture (ATR), including in elite sportspeople. A recent cadaveric study demonstrated an increased ultimate load could be applied using an FHL tendon transfer with interference screw and cortical button applied using a tension slide technique compared with interference screw alone. The aim of this study was to explore patient-related outcome measures (PROMs) following modification to this operation.
Methods: We reviewed the imaging, history, PROMs and complications of 17 patients who underwent endoscopic FHL tendon transfer for chronic ATR using the modified FHL reconstruction technique. The primary outcome was the Manchester-Oxford Foot Questionnaire (MOxFQ), EuroQol–5 Dimensions (EQ-5D), and visual analog score for pain (VAS-Pain) with a mean follow up of 1.5 years.
Results: Seventeen patients (11 male, 6 female) underwent endoscopic FHL tendon transfer between September 2020 and May 2023. Mean (SD) age at the time of surgery was 58.3 (16.1) years, and mean (SD) BMI was 27.6 (4.8). A specific event in the history associated with the rupture was present in 13 of 17 patients (76.5%); the median (IQR) time between injury and surgery was 33 weeks (21-42). Sixteen surgeries were primary procedures for chronic ATR, and 1 surgery was a revision procedure after a failed open acute ATR repair. MOxFQ, EQ-5D, and VAS-pain scores all showed a statistically significant improvement postoperatively (minimum 10months) when compared to preoperative scores. There was 1 symptomatic complication of tibial neuritis (5.9%).
Conclusion: Endoscopic FHL tendon transfer for chronic ATR augmented using a cortical button as well as an interference screw seems to be a safe and effective procedure, with patients reporting a statistically significant improvement in health- related quality of life, pain, and specific foot and ankle outcome function.
Disclosure: No disclosures
631 - Osteochondral lesions of the talus treated with open Autologous Matrix Induced Chondrogenesis (AMIC): Medium term results
Mohammad Salim, Mohit Sethi, Rajiv Limaye
University Hospital of North Tees, Stockton-on-Tees, United Kingdom
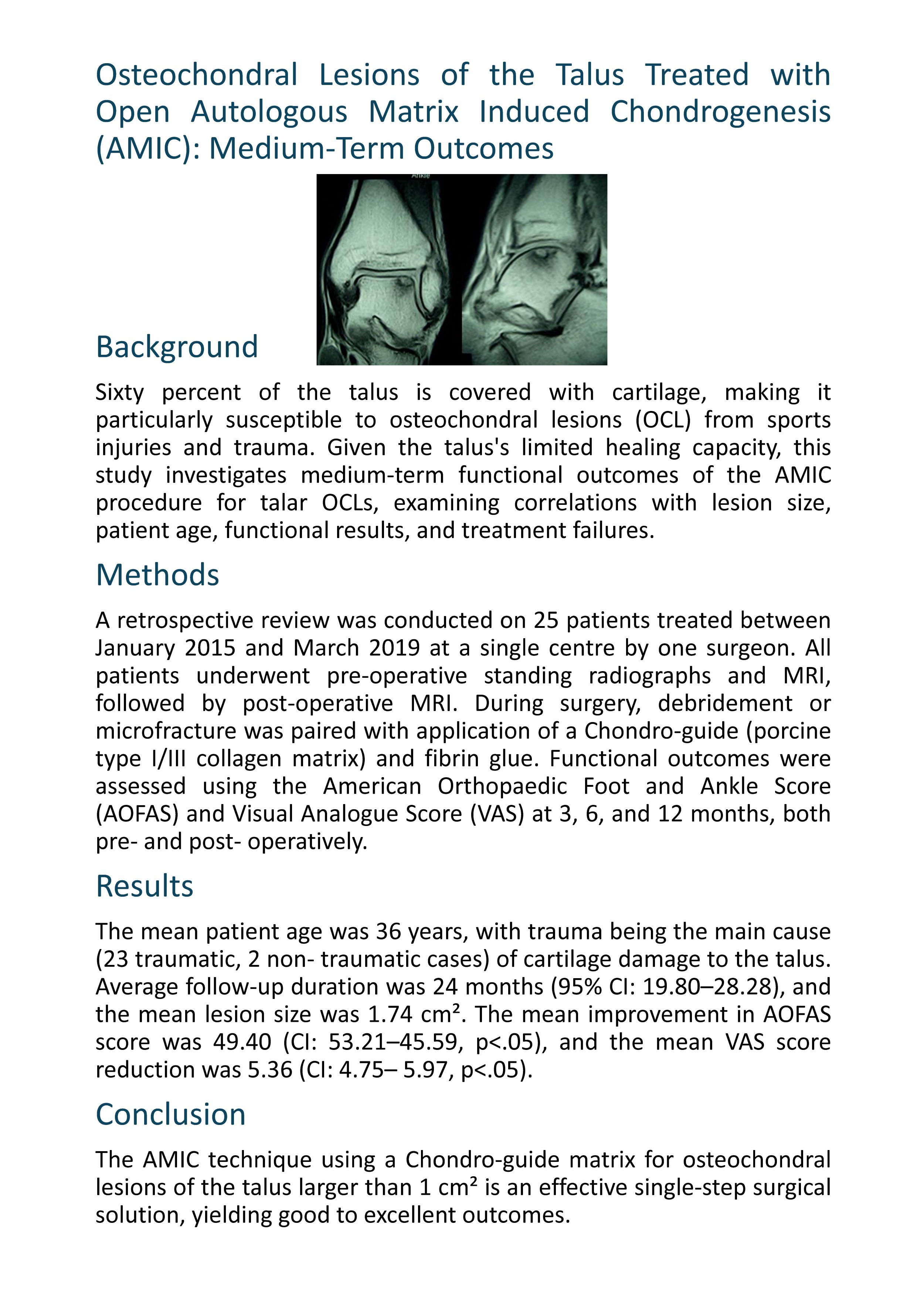
Background: 60% of the talus is covered by cartilage. Sports injuries and trauma can lead to osteochondral lesions (OCL) of the talus, which inherently has poor regenerative capacity. This study aims to evaluate medium term functional outcome of AMIC procedure for OCL of the talus and correlate them with the size of lesion, patient age, functional outcome and failures.
Methods: This was a 25 patient retrospective, single centre, single surgeon study from Jan 2015 to March 2019. All patients had pre-operative standing radiographs and MRI followed by post-op MRI. Intraoperative debridement/ microfracture was combined with Chondro-guide (type I/III porcine collagen matrix) application with fibrin glue. Pre-op and Post-op American Orthopaedic Foot and Ankle Score (AOFAS) and Visual Analogue score (VAS) were done at 3, 6 and 12 months
Results: The mean patient age was 36 years. Main aetiology was trauma (23 patients ; 2 non- traumatic) Mean follow up was 24months (95% CI-19.80-28.28), Mean size of the osteochondral lesion was 1.74 cm2 Mean difference between preoperative and post operative AOFAS score was 49.40 (CI 53.21-45.59) (p<.05) and VAS score was 5.36 (CI 4.75-5.97) (p<.05)
Conclusion: AMIC with Chondro-guide matrix procedure for >1 cm2 osteochondral lesions of talus is a one-step surgical technique with excellent to good results.
691 - Comparative cohort study of Immediate cast vs Immediate Boot in the Functional Non-operative management of Achilles Tendon Ruptures

Milosz Kostusiak, Hasan Altahoo, David Townshend
North Tyneside General District Hospital, North Shields, United Kingdom
Introduction: Achilles tendon rupture is a common injury of lower limbs in adults. Conservative management using Accelerated Rehabilitation is a mainstream treatment for these injuries, resulting in comparable outcomes to surgical intervention. This study aims to compare initial moonboot with wedges (MBW) vs initial equinus cast (EC) immobilisation on outcomes of Achilles tendon ruptures.
Methodology: Retrospective cohort study of patients with acute Achilles tendon rupture between January 2018 and December 2022. Review of emergency department notes, clinic letters and radiology reports. Follow up period of one year. Primary outcome was re-rupture within the first 12 months. Secondary outcomes were conversion to surgical management due to failed conservative treatment, patient reported outcome measures using Achilles Tendon Rupture Score (ATRS), and time to return to work and sport activities.
Results: 343 patients were identified with acute Achilles tendon rupture (0-14 days) with treatment documented in 340. Majority were male (77.2%), an average age of 52 (16-89). Most common mode of injury was contact sports (26.5%). Eighteen patients were managed with surgery during the treatment due to own choice or insertional tear. Thus, 271 patients (83.4 %) with EC and 55 patients (16%) were managed with initial MBW. The total re-rupture rate was 1.8% (n=5), all of which were treated with EC at initial orthopaedic review. No re-ruptures were reported in patients managed in initial MBW. Conversion to surgery was reported in 4 patients that was treated in MBW vs 6 patients treated in the EC due to persisting gap. ATRS scores and return to work/sporting activities were not statistically significant between both groups.
Conclusion: Patients with acute Achilles tendon ruptures managed initially in moonboot with wedges have comparable clinical outcomes to those managed in equinus cast. This study supports the use of either method of initial treatment of Achilles tendon ruptures.
711 - Mini open Achilles repair: Surgical outcomes and resource assessment in a consecutive 100 patient case series
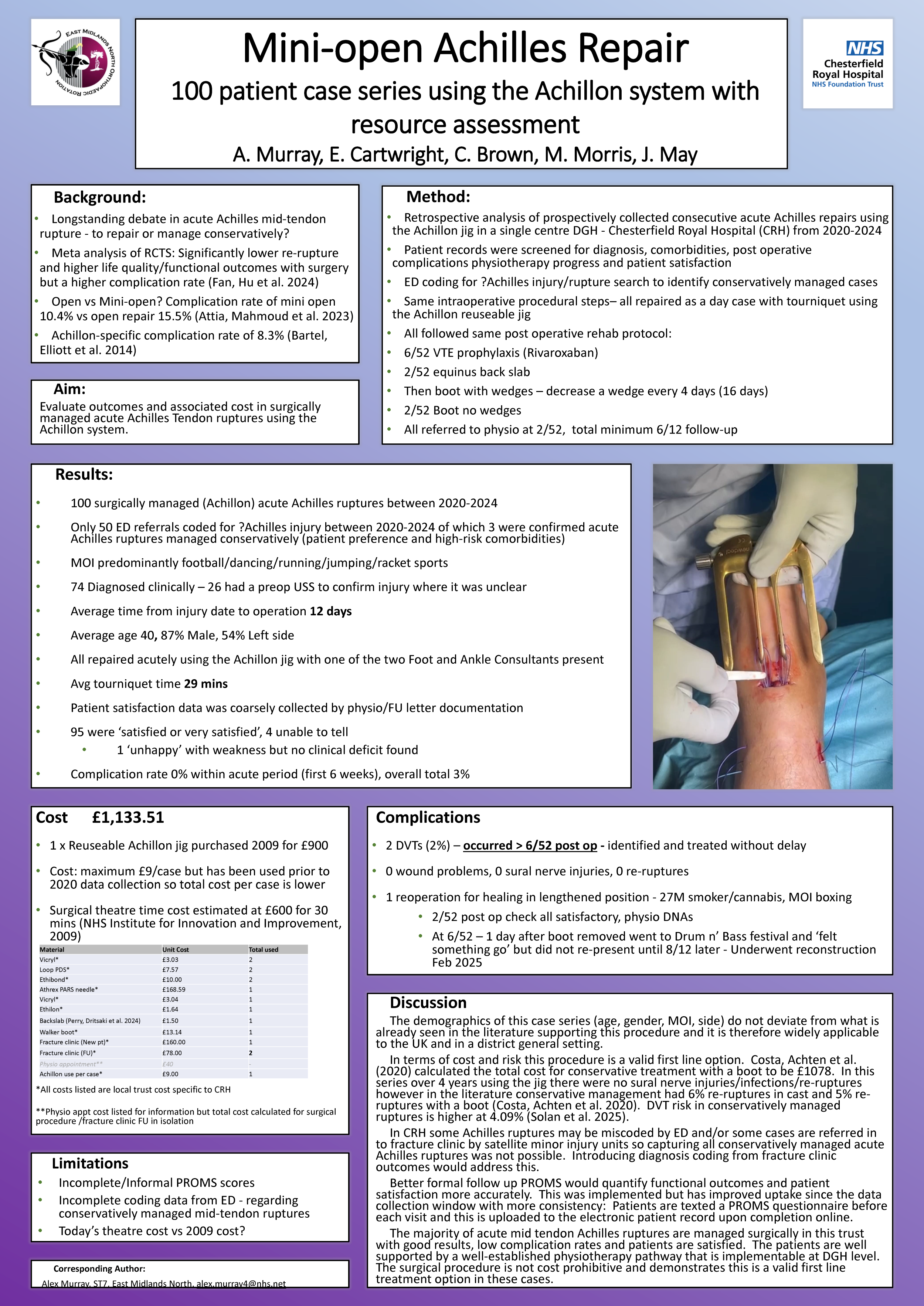
Alex Murray, Emily Cartwright, David Sprot, Matthew Morris, Jonathan May
Chesterfield Royal Hospital, Chesterfield, United Kingdom
Achillon is a minimally invasive system for Achilles tendon repair used in our trust for all acute repairs. A retrospective analysis was performed on prospectively collected data for 100 consecutive patients with minimum follow up of 6 months from 2019 to 2024 from a single district general hospital in England. All repairs were performed with a Foot and Ankle consultant present under tourniquet and all followed the same post operative rehabilitation protocol. Operative technique used is described.
Results: The demographic had an average age of 41, predominantly men and with an average tourniquet time of 29 minutes. There were no immediate or delayed sural nerve injuries. Our DVT rate was 2% and 1% healed in a lengthened position requiring re-operation (in a non-compliant individual). There were no re-ruptures and no superficial or deep infections. Successful rehabilitation was achieved in 99% of patients; they were either satisfied or very satisfied based on physiotherapy reports and clinic letters. One patient was unhappy with subjective weakness despite a good clinical outcome and appropriate progression with physiotherapy. Furthermore a basic cost and NHS resource assessment was carried out – examining the cost in terms of the purchase of the Achillon jigs, operative materials, theatre time, appointments and post operative footwear (boot with wedges).
This case series represents one of the largest reported and adds to the growing body of evidence currently published. It identifies resources needed to deliver an acute operative Achilles rupture treatment protocol with a low complication rate and a high success rate within an NHS district general hospital setting.
No disclosures.
762 - Anterior Malleolar Fractures: A Retrospective Review of Fixation Methods and Outcomes
Abdul-Rahman Gomaa1,2, Richard Huynh1, Hakim Ben Nusir1, Hayley Cullen1, Louise Jones1, Mohamed Abdellatif1, Gabrielle Jones1, Cameron Kennedy1, Ashka Moothoosamy1, Menahel Sajjad1, Rahul Mohan Kumar1, Lyndon Mason1,2
1Liverpool Orthopaedic & Trauma Service, Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom. 2School of Medicine, University of Liverpool, Liverpool, United Kingdom
Introduction: The anterior malleolus is an increasingly popular term which describes the anterior distal tibial or the Tillaux-Chaput tubercle. Fractures of which can lead to instability of the ATFL component of the syndesmosis, similar to posterior malleolar fractures. Anterior malleolar fractures (AMFs) have recently been classified by Rammelt et al. based on pathoanatomy and a treatment algorithm was proposed. The aim of this study is to compare the complications of the various fixation methods undertaken locally.
Methods: A retrospective review of all operatively treated ankle fractures between August 2022 and March 2024 was undertaken. Comorbidities, injury details, fracture morphology, operative details, clinical and radiographic follow-up were recorded. Complications were classified in line with the modified Clavien-Dindo grading for foot and ankle surgery.
Results: 427 operatively treated ankle fractures were identified, of which; 22 (5.15%) had a surgically treated AMFs. 12 (54.55%) were treated using a buttress plate, 7 (31.82%) were treated using a combination of plate and screw and 3 (13.64%) were treated using a screw. Of the 12 treated with a plate, 7 (58.33%) patients developed postoperative complications (Grade 1A: 1, Grade 2A: 2, Grade 2B: 1, Grade 3A: 1, Grade 3B: 2); all of which were associated with plate fixation.
Conclusions: AMFs are relatively uncommon injuries. Whilst plate fixation is a commonly used method for treating AMFs, it is associated with a higher rate of postoperative complications compared to other fixation methods like screws or a combination of plate and screw. This finding needs further investigation to further understand the injury and the treatment of these fractures.
763 - Accessing the Posterior Malleolus: The posterolateral or medial posteromedial approach?
Abdul-Rahman Gomaa1,2, Richard Huynh1, Hakim Ben Nusir1, Hayley Cullen1, Louise Jones1, Mohamed Abdellatif1, Gabrielle Jones1, Cameron Kennedy1, Ashka Moothoosamy1, Menahel Sajjad1, Rahul Mohan Kumar1, Lyndon Mason1,2
1Liverpool Orthopaedic & Trauma Service, Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom. 2School of Medicine, University of Liverpool, Liverpool, United Kingdom
Introduction: The posterolateral (PL) approach to the ankle remains to be commonly used for accessing the posterior malleolus (PM) despite its limitations which include inadequate exposure of the fracture as well as increased risk to peroneal artery. REF As such, the medial posteromedial (MPM) approach has been developed and described to address these two issues. REF The aim of this study is to compare the complications of the two approaches.
Methods: A historic cohort study all operatively treated ankle fractures between August 2022 and March 2024 was undertaken. Comorbidities, injury details, fracture morphology, operative details, clinical and radiographic follow-up were recorded. Complication were classification in line with the modified Clavien-Dindo grading for foot and ankle surgery.
Results: 427 operatively treated ankle fractures were screened, 92 (21.55%) involved surgically treated PMFs. Of these, the MPM approach was used in 68 cases (73.91%), while the PL approach was used in 12 cases (13.19%). Of the 68 MPM approaches, 10 (14.71%) patients developed postoperative complications (Grade 1A: 3, Grade 1B: 1, Grade 2A: 3, Grade 2B: 1, Grade 3A:1, Grade 3B:1). Of the 12 PL approaches, 8 (66.67%) patients developed postoperative complications (Grade 1B: 1, Grade 2A: 4, Grade 2B: 1, Grade 3A: 1, Grade 3B: 1).
Conclusions: In this study, the MPM approach to the ankle was associated with fewer and less severe postoperative complications compared to the PL approach. The MPM approach has greater utility in exposing the posterior tibia, and is possibly safer than the PL approach.
816 Superior mid-term outcomes with platelet-rich-plasma versus corticosteroid injections in plantar fasciitis. Results from a randomised controlled study
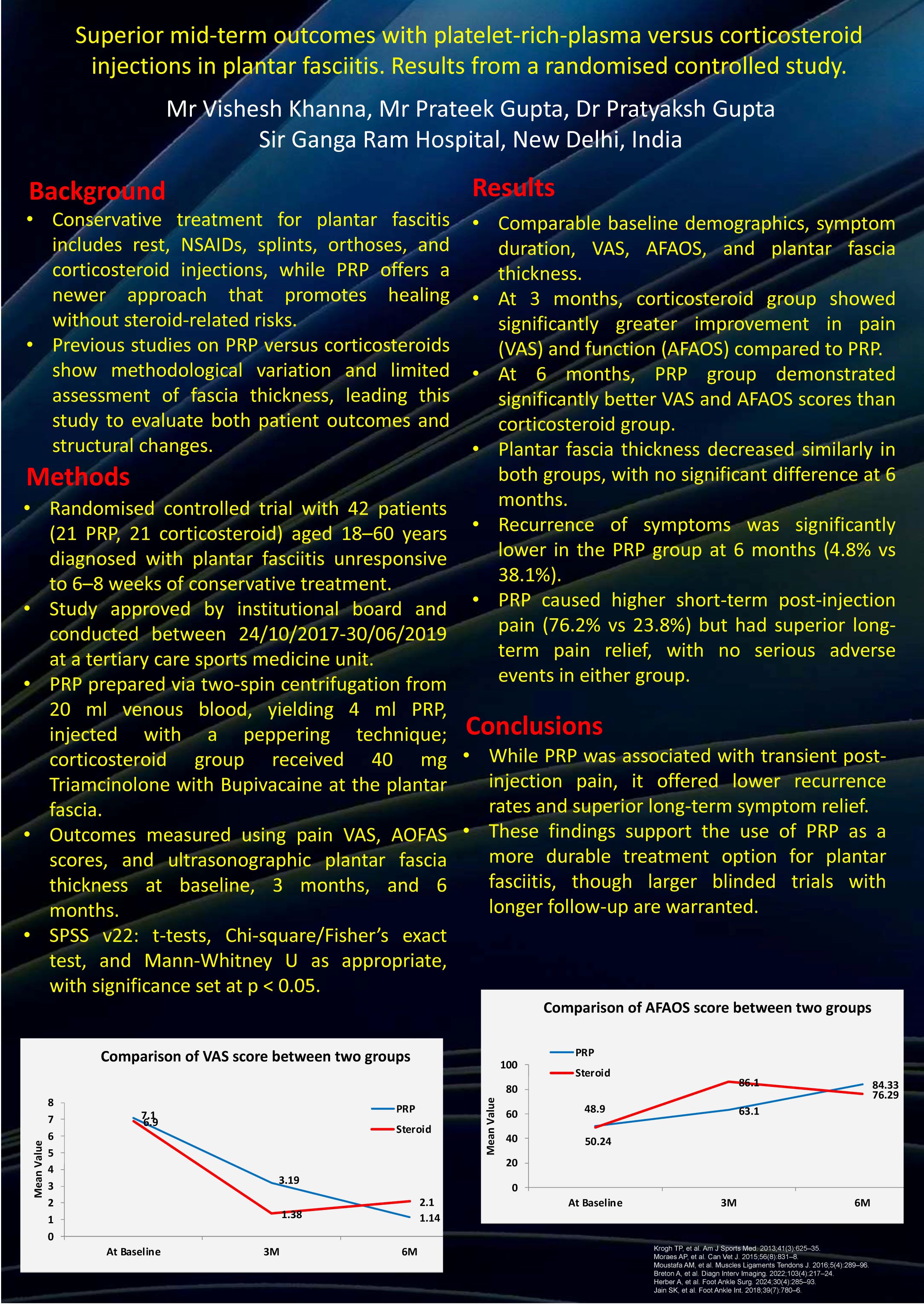
Vishesh Khanna, Prateek Gupta, Pratyaksh Gupta
Sir Ganga Ram Hospital, New Delhi, India
Background: Among methods for treating plantar fasciitis, conservative options including rest, nonsteroidal anti-inflammatories, splints, orthosis and corticosteroid injections have been promulgated. Whilst considering the latter in recalcitrant cases, the need for repeated injections and risks of rupture and fat pad atrophy serve as obvious limitations. In this context, platelet-rich plasma injections have found importance in recent times from its ability to enhance cellular chemotaxis, proliferation and differentiation, removal of debris, angiogenesis and laying down of extracellular matrix. This study was primarily aimed at evaluating the efficacy of PRP vis-a-vis corticosteroid injections in plantar fasciitis. Secondarily, we compared changes in plantar fascia thickness pre and post-injection with both modalities.
Methods: Over 18 months, 42 adults were prospectively randomised into receiving PRP (21) and corticosteroid plantar fascia injections (group B). Randomisation was done by sealed, opaque envelopes by computer-generated numbers. Demographic and clinical data, visual analogue pain scale and American Orthopaedic Foot & Ankle Society (AOFAS) scores were collected along with ultrasonographic data for plantar fascia thickness. Patients were followed up and 3 and 6 months.
Results: Mean pre-injection scores were 7.10±0.83 and 6.90 ± 0.70 in PRP and steroid groups (P=.427). Post-injection VAS scores similarly improved in both groups. Mean AFAOS scores between PRP and steroid groups at 3 months (63.1 vs 86.1, P<0.001) showed better results in the former. Likewise, 6-month scores were superior for PRP (84.3 vs 76.3, P=0.014). At 6 months, mean plantar fascia thickness was comparable across both groups (3.39 vs 3.4 mm, respectively, P=0.973).
Conclusions: PRP injections yield greater function at 3 and 6-month follow-ups in patients with recalcitrant plantar fasciitis. Among other evolving indications for PRP use, plantar fasciitis finds itself on a potential spectrum, when considering conservative options of management in recalcitrant cases. Our results highlight its utilitarian application when compared to corticosteroid injections.
872 - Vascular Considerations in Posterior Malleolus Fracture Surgery – The Prevalence of The Peroneal Artery Communicating Branch and Peroneal Artery Dominance
Shahjahan Aslam, Chiijoke Orji, Kosha Gala, Craig Wyatt, Zeeshan Akbar, Muhaned El-Gheryani, Mohamed Abdellatif, Lydon Mason
Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom
Background: The risk of vascular injury is a rare but significant concern in posterior malleolus fracture (PMF) surgery, especially with the commonly employed posterolateral approach. Anatomical variations of the peroneal artery have been blamed for serious vascular complications with the PL approach. The aim of this study is to investigate the prevalence of peroneal artery communicating branch (PACB) and peroneal artery dominant (PAD) lower limbs.
Methods: A historic cohort study was performed on 916 lower limb computed tomography angiographies (CTA). Patient data were stratified based on clinical indication for imaging, laterality, and the presence or absence of the communicating branch.
Results: A PACB was identified in 288 (31.4%) of the cases. The prevalence was significantly higher in patients with PVD (n = 226 (78.5%) compared to those imaged for trauma (n = 18), free fibula graft assessment (n = 16), or other vascular concerns (n = 28). Notably, in cases where the PACB was present, 40% had an atretic proximal posterior tibial artery thus making the lower limb PAD through the PACB. The PACB occurs approximately 4cm proximal to the joint, posing a substantial risk of arterial compromise if the posterolateral approach is used.
Conclusion: Our findings reinforce the existing anatomical literature regarding the variability of peroneal artery branching and underscore the potential hazards of a posterolateral approach in PMF fixation. Inadvertent ligation of the communicating branch may lead to ischemic complications. Given the high prevalence of this variation, particularly in patients with PVD, the posterolateral approach should be approached with caution.
Disclosure: The authors declare no conflict of interest
Hip
262 - The Association Between Preoperative Anaemia And Early Postoperative Outcomes After Primary Hip And Knee Arthroplasty Under An Enhanced Recovery Programme: An Observational Study
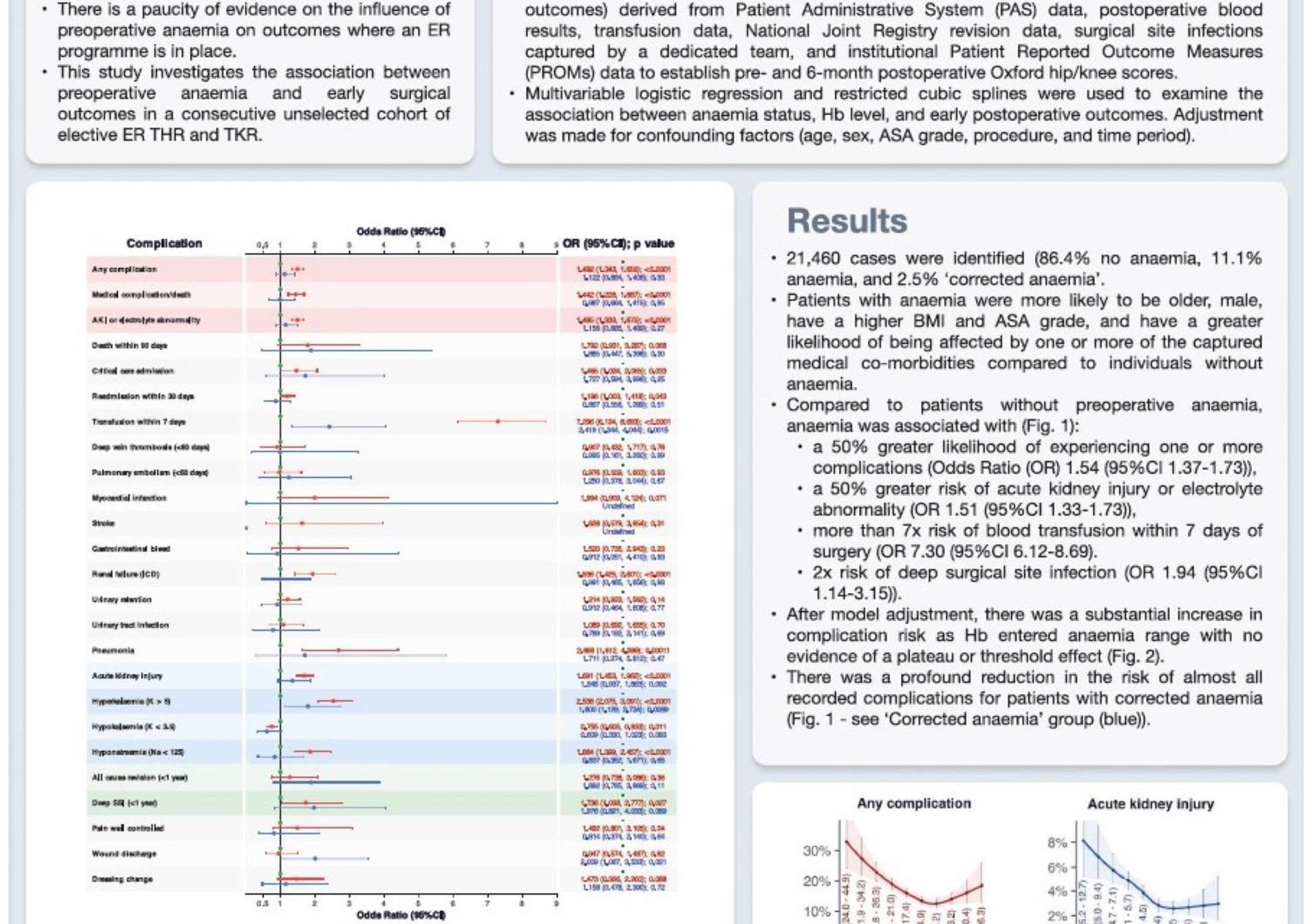
Richard Holleyman1,2, Sameer Khan2, Ashley Scrimshire2, Philip Stamp3, Mike Reed2
1Newcastle University, Newcastle Upon Tyne, United Kingdom. 2Northumbria Healthcare, Ashington, United Kingdom. 3Northumbria Healthcare, Cramlington, United Kingdom
Background: We investigated the effect of preoperative anaemia (PA) on early post-operative outcomes in patients undergoing elective primary hip or knee replacement (pTJA) under an enhanced recovery (ER) programme.
Methods: ER data including patient characteristics, comorbidities, preoperative blood indices and postoperative outcomes including transfusion, medical complications, surgical site infection and patient reported outcomes were analysed for a consecutive series of 21,460 pTJA performed at a single institution between 2008-2019.
Data for anaemic (2,375 episodes, 11.1%) and non-anaemic cohorts were compared. Additionally, patients who had their anaemia successfully corrected by the time of surgery were identified as a separate group. Multivariable logistic regression and restricted cubic splines were used to examine the association between anaemia, pre-operative haemoglobin and early postoperative outcomes.
Results: PA was associated with significantly increased risk of almost all studied complications including transfusion (Odds Ratio (OR)=7.1 [95%CI 6.0 -8.4]), critical care admission (OR=1.4 [1.0-2.0]) and suffering one or more of any captured complication (OR=1.5 [1.3-1.6]) but not venous thromboembolism or death. There was a substantial increase in complication risk as pre-operative haemoglobin entered anaemia range. There was a reduction in the risk of one or more complications for patients where previous anaemia was successfully corrected pre-operatively, although this did not reach statistical significance and numbers in this group were small (n=535). Preoperative and 6-months post-operative Oxford scores were significantly lower in the anaemic cohort, however the improvement in scores was not significantly different between cohorts.
Conclusion: Pre-operative anaemia is associated with detrimental postoperative outcomes, despite the stress-reducing and blood-conserving measures used in ER arthroplasty. Correcting anaemia may help to mitigate this risk.
353 - Complications and Functional Outcomes of Total Hip Arthroplasty after Pelvic Radiation: A Systematic Review and Meta-analysis
José María Lamo-Espinosa1, Gonzalo Mariscal2, Jorge Gómez-Álvarez3, Mikel San Julián3
1IMED Colón, Valencia, Spain. 2Valencia Catholic University, Valencia, Spain. 3University of Navarra Clinic, Navarra, Spain
Background: Total hip arthroplasty (THA) outcomes in patients with prior pelvic irradiation require careful evaluation due to the growing cancer survivor population and increased radiotherapy use. Radiation's adverse effects on bone may compromise prosthesis integration.
Methods: A systematic review following PRISMA guidelines was conducted across multiple databases examining THA complications in post-pelvic radiation patients. The analysis included cohort studies and clinical series, evaluated using MINORS criteria. Data pooling utilized Review Manager 5.4's generic inverse variance method, with sensitivity analyses for radiation dose, percentage of patients with osteoradionecrosis and radiation-to-THA timing.
Results: Analysis of twelve studies (2,876 patients) with follow-up ranging 24-120 months revealed: dislocation rate of 8.18%; aseptic loosening in 15.00%; septic loosening in 6.57%; radiolucency in 23.10%; revision surgeries in 13.89%; and intraoperative complications in 5.60%. Radiation dose did not influence outcomes, while longer radiation-to-THA intervals reduced complications. Harris Hip Score improved significantly (mean 37.36, 95% CI 26.97-47.74). Studies with higher percentage of patients with osteoradionecrosis presented higher rate of complications.
Conclusion: Total hip arthroplasty following pelvic radiation carries high complication risks specially in patients with osteoradionecrosis. Functional outcomes showed significant improvement at final follow-up.
420 - Comparative assessment of relaxed- and flexed-seated radiographs in evaluating spinopelvic parameters in Total Hip Arthroplasty
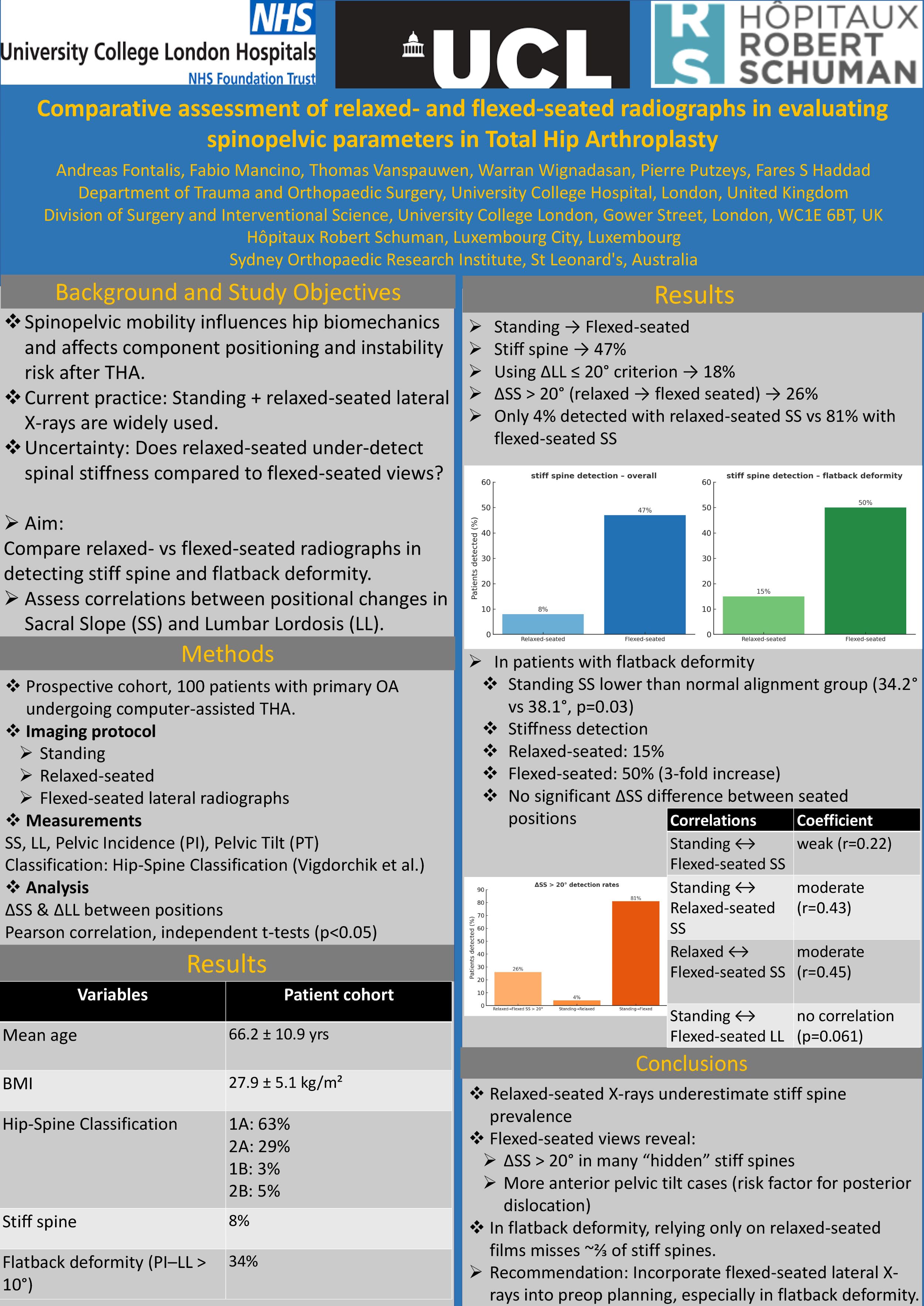
Andreas Fontalis1,2, Fabio Mancino3, Thomas Vanspauwen4, Warran Wignadasan1,2, Pierre Putzeys4, Fares S Haddad1,2
1Department of Trauma and Orthopaedic Surgery, University College Hospital, London, United Kingdom. 2Division of Surgery and Interventional Science, University College London, London, United Kingdom. 3Sydney Orthopaedic Research Institute, St Leonards, Australia. 4Hôpitaux Robert Schuman, Luxembourg City, Luxembourg
Background: This study evaluated the comparative value of relaxed- and flexed-seated lateral radiographs in assessing spinopelvic mobility in THA.
Methods: A prospective cohort of 100 patients undergoing THA for primary osteoarthritis underwent radiographic assessment in standing, relaxed-seated and flexed-seated positions. Measurements included sacral slope(SS), lumbar lordosis(LL), pelvic incidence(PI) and pelvic tilt(PT). Patients were also classified according to the Hip-Spine Classification.
Results: Mean age was 66.2 years and BMI 27.9. Based on standing to relaxed-seated change, 8% were classified as stiff (types 1B/2B) and 34% had flatback deformity(PI–LL>10°). Using standing to flexed-seated views, 47% met stiff spine criteria and 18% had ΔLL ≤ 20°. Among these, only 11% were identified using relaxed-seated SS, compared to 72% using flexed-seated SS.
Mean ΔSS between relaxed- and flexed-seated positions was 14.6 ± 12.1°,with 26% showing ΔSS > 20°. SS increased (anterior tilt) in 24% of patients from standing to flexed-seated and exceeded 10° in 7%. All such patients were classified as stiff. No association was found between ΔSS > 20° and BMI, PI, or native SS. In patients with flatback deformity, stiffness was identified in 15% using relaxed-seated SS vs 50% with flexed-seated. These patients also had lower standing SS (34.2° vs 38.1°,p=0.03), but similar ΔSS between seated positions.
Conclusion: Relaxed-seated radiographs may underestimate the prevalence of spinal stiffness. The lack of strong correlation between standing and flexed-seated parameters limits predictive value, making flexed-seated X-rays a useful tool in surgical planning. Patients with a stiff spine may show a ΔSS > 20° between relaxed- and flexed-seated views, making relaxed-seated imaging alone insufficient to identify them. Additionally, relaxed-seated X-rays may underdetect anterior pelvic tilt changes. In patients with flatback deformity, relying solely on relaxed-seated imaging may lead to a threefold underestimation of stiffness, supporting the use of flexed-seated radiographs in this group.
448 - Registry-Based Validation of 3D-Printed Titanium Acetabular Shells: a Comparative AJRR Analysis of Over 290,000 Cases
Dennis Nam1, Manoshi Stoker2, Ahmad faizan2, Michael Masini3, Sebastien Lustig4
1RUSH, Chicago, USA. 2Stryker, Mahwah, USA. 3Trinity Health, Ypsilanti, USA. 4Lyon Croix-Rousse University Hospital, Lyon, France
Background: 3D printed porous titanium acetabular shells have been introduced in the recent past with an intention to enhance biological fixation between the implant and underlying bone. The purpose of this work was to investigate midterm device survivorship and reasons for revision of a modern 3D printed porous acetabular shell as reported in the American Joint Replacement Registry (AJRR).
Methods: All primary THA cases in patients over 65 years of age from January 2016 – December 2023 submitted to AJRR as of December 2024 with Medicare data were queried in this 7-year analysis. Data was stratified into two treatment groups: aggregated cementless acetabular shells and a specific 3D printed acetabular shell design. This analysis included 233,182 aggregated cementless acetabular shells and 60,587 3D printed acetabular shells. Cumulative revision rate and reasons for failure, per ICD 9 and 10, were determined. AJRR data was linked to Medicare claims data through a unique identifier provided by the Research Data Assistance Center (ResDAC). A Cox regression model was run for both groups, controlling for age and sex. Descriptive statistics were used to determine significant differences between groups with alpha at 0.05.
Results: Both cohorts in this analysis had excellent survivorship at 7 years, : 97.3% (95% CI: 97.1% –97.4%) for 3D-printed shells and 97.2% (95% CI: 97.1% – 97.3%) for aggregate shells. The aggregated cementless acetabular shell and 3D printed acetabular shell groups had 2.17% and 1.75% all-cause revision rates respectively. Aseptic loosening presented 0.17% of 3D printed shells and 0.25% of aggregate shells (p<0.001).
Conclusion: Midterm results suggest excellent survivorship and good fixation with low rates of loosening for the acetabular shell design. National registries provide a source of real-world evidence which is indicative of product performance at a national level.
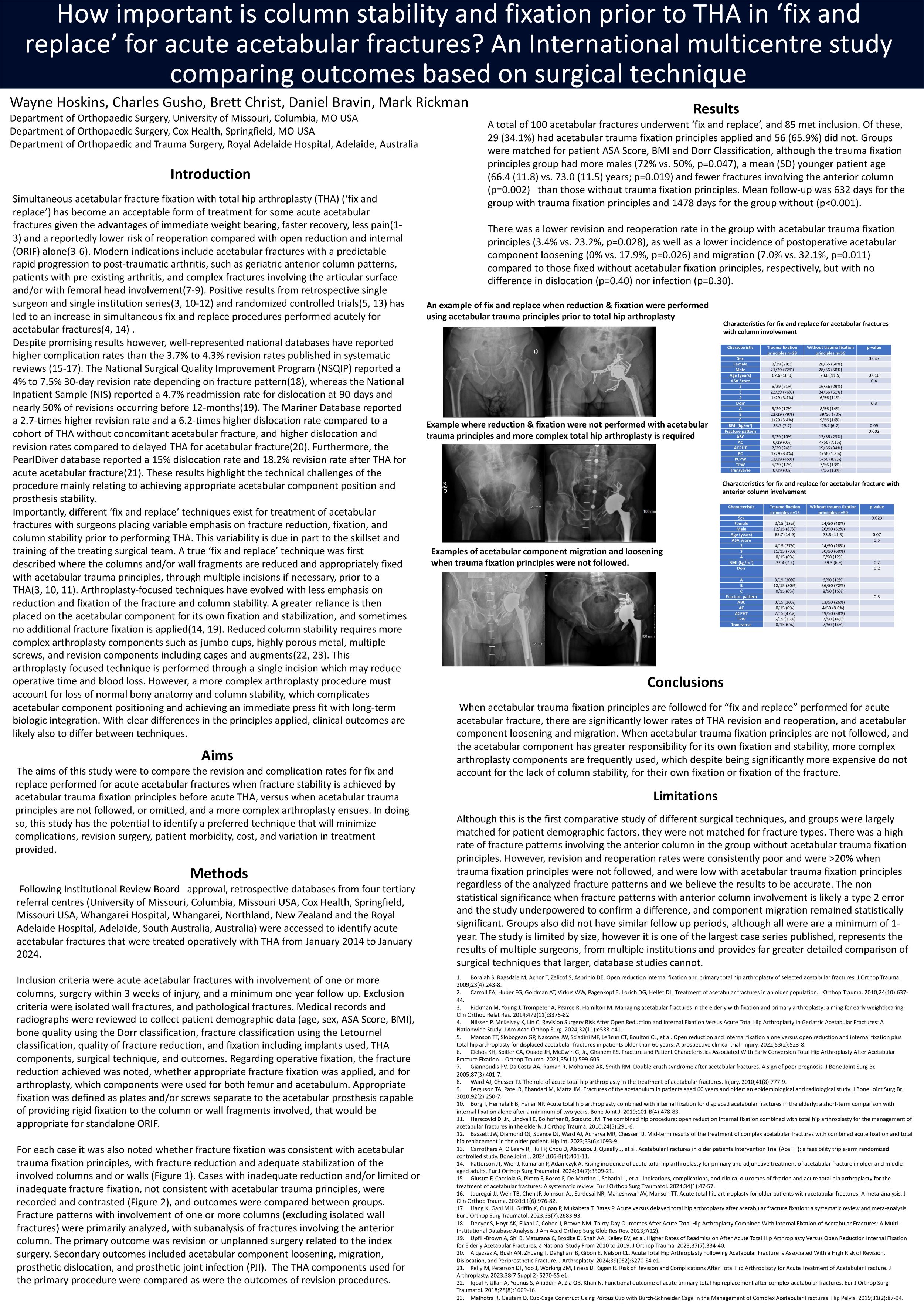
529 - How important is column stability and fixation prior to THA in ‘fix and replace’ for acute acetabular fractures An International multicentre study comparing outcomes based on surgical technique
Wayne Hoskins1, Charles Gusho1, Brett Christ1, Daniel Bravin2, Mark Rickman3
1University of Missouri, Columbia, USA. 2Cox Health, Springfield, USA. 3Royal Adelaide Hospital, Adelaide, Australia
Introduction: Combined acetabular fracture fixation with total hip arthroplasty (THA; ‘fix and replace’) for acute acetabular fracture treatment is increasing. However, failure rates are high and techniques vary widely. This study compared outcomes of ‘fix and replace’ when column stability is achieved with trauma fixation principles before THA, versus when THA is performed without either sufficient columnar stability or appropriate fracture fixation.
Methods: A retrospective cohort study among four tertiary centres was performed. Acutely treated (< 3 weeks) acetabular fractures involving one or more columns, fixed concurrently with THA and with one-year minimum follow-up were included. Patient demographics, fracture characteristics, reduction and fixation techniques, components and implants used, and outcomes were collected. It was noted whether fractures were reduced and fixed using trauma fixation principles before THA or whether limited and/or no fixation was applied, with or without appropriate fracture reduction. The primary outcome was revision or reoperation.
Secondary outcomes included component loosening, migration, dislocation, and infection.
Results: One-hundred cases of ‘fix and replace’ were identified, and 85 (85.0%) met inclusion. Of these, 29 (34.1%) had trauma fixation principles and 56 (65.9%) did not. Groups were matched for ASA and BMI, but the trauma fixation principles group had more males (72% vs. 50%, p=0.047), a younger mean age (SD) (66.4 (11.8) years vs. 73.0 (11.5), p=0.019), and fewer anterior column fractures (p=0.002).
There was a lower revision and reoperation rate for ‘fix and replace’ surgeries treated with trauma fixation principles (3.4% vs. 23.2%, p=0.028), along with less acetabular component loosening (0% vs. 17.9%, p=0.026) and migration (7.0% vs. 32.1%, p=0.011), though no difference in dislocation (p=0.4) nor infection (p=0.3).
Conclusion: When appropriate acetabular column reduction and fixation is not performed, there is an unacceptably high arthroplasty failure rate following a fix and replace strategy performed for acute acetabular fractures.
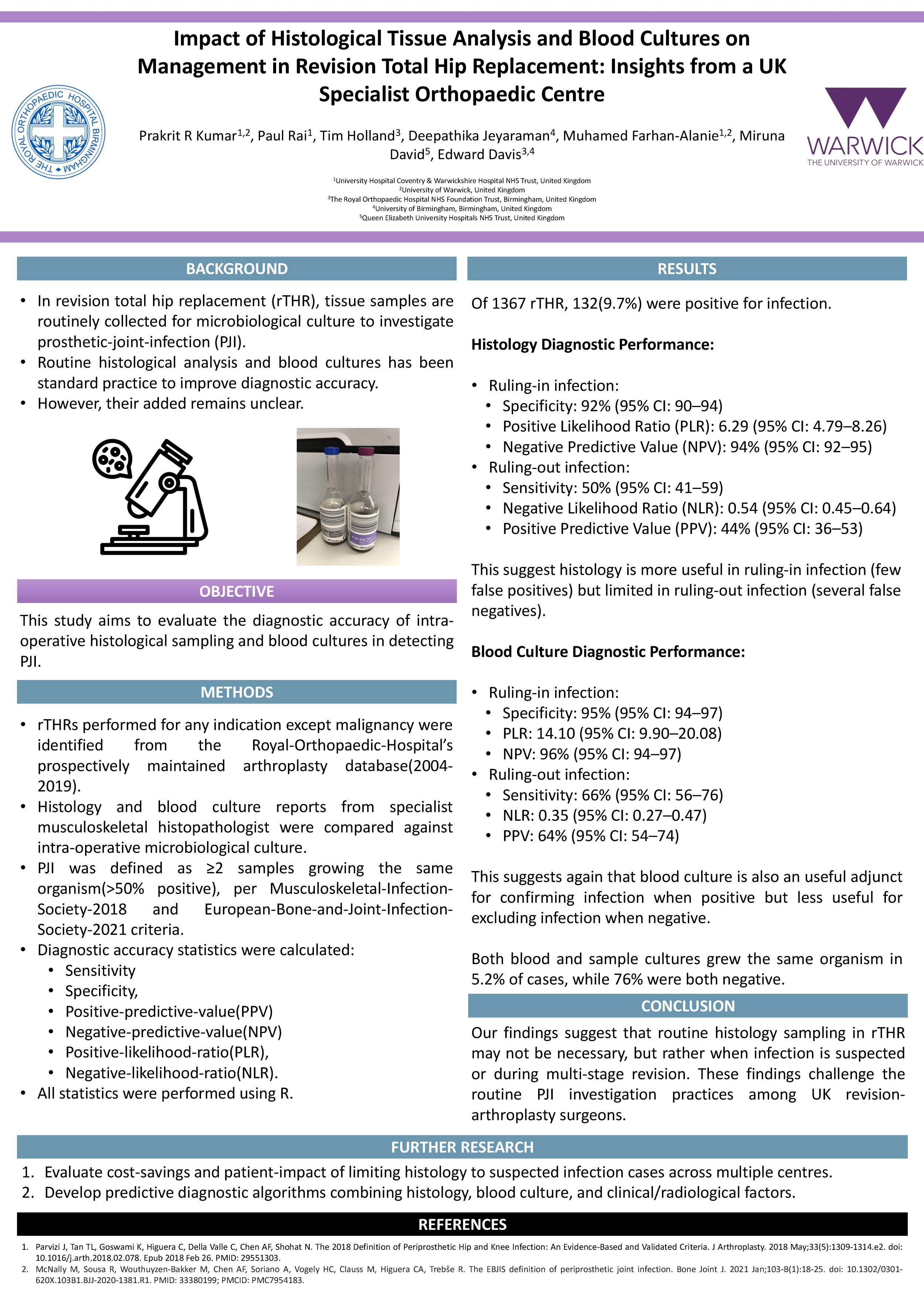
535 - Impact of Histological Tissue Analysis and Blood Cultures on Management in Revision Total Hip Replacement: Insights from a UK Specialist Orthopaedic Centre
Prakrit Kumar1,2, Paul Rai1,3, Tim Holland3, Muhamed Farhan-Alanie2,1, Miruna David4, Edward Davis3
1University Hospital Coventry & Warwickshire Hospital NHS Trust, Coventry, United Kingdom. 2University of Warwick, Warwick, United Kingdom. 3The Royal Orthopaedic Hospital NHS Foundation Trust, Birmingham, United Kingdom. 4University of Birmingham, Birmingham, United Kingdom
In revision total hip replacement (rTHR), tissue samples are routinely collected for microbiological culture to investigate prosthetic-joint-infection (PJI). Routine histological analysis and blood cultures has been standard practice to improve diagnostic accuracy. However, their added remains unclear. This study evaluates their diagnostic accuracy in detecting PJI. This study aims to evaluate the diagnostic accuracy of intra-operative histological sampling and blood cultures in detecting PJI.
rTHRs performed for any indication except malignancy were identified from the Royal-Orthopaedic-Hospital’s prospectively maintained arthroplasty database(2004-2019). Histology and blood culture reports from specialist musculoskeletal histopathologist were compared against intra-operative microbiological culture. PJI was defined as ≥2 samples growing the same organism(>50% positive), per Musculoskeletal-Infection-Society-2018 and European-Bone-and-Joint-Infection-Society-2021 criteria. Diagnostic accuracy, including sensitivity, specificity, positive-predictive-value(PPV), negative-predictive-value(NPV), positive-likelihood-ratio(PLR), and negative-likelihood-ratio(NLR), with 95% confidence-intervals(CIs), was calculated.
Of 1367 rTHR, 132(9.7%) were positive for infection. Histology showed high specificity(92%, 95%CI:90–94), PLR (6.29, 95%CI:4.79–8.26), and NPV(94%, 95%CI:92–95), but low sensitivity(50%, 95%CI:41–59), NLR (0.54, 95%CI:0.45–0.64), and moderate PPV(44%, 95%CI:36–53), making it reliable for ruling-in infection but not ruling-out infection. Similar to histology, blood culture was useful adjunct for ruling-in infection (specificity(95%, 95%CI:94–97), PLR(14.10, 95%CI:9.90–20.08), NPV(96%, 95%CI:94–97)) but not at ruling-out infection (sensitivity(66%, 95%CI:56–76), NLR(0.35, 95%CI:0.27–0.47), and moderate PPV(64%, 95%CI:54–74)). In 5.2% of cases, both blood and sample cultures grew the same organism, while 76% were both negative.
While blood culture still serves as a useful adjunct in the diagnostic process, our findings suggest that routine histology sampling in rTHR may not be necessary, but rather when infection is suspected or during multi-stage revision. These findings challenge the routine PJI investigation practices among UK revision-arthroplasty surgeons and offer potential for substantial cost-savings.
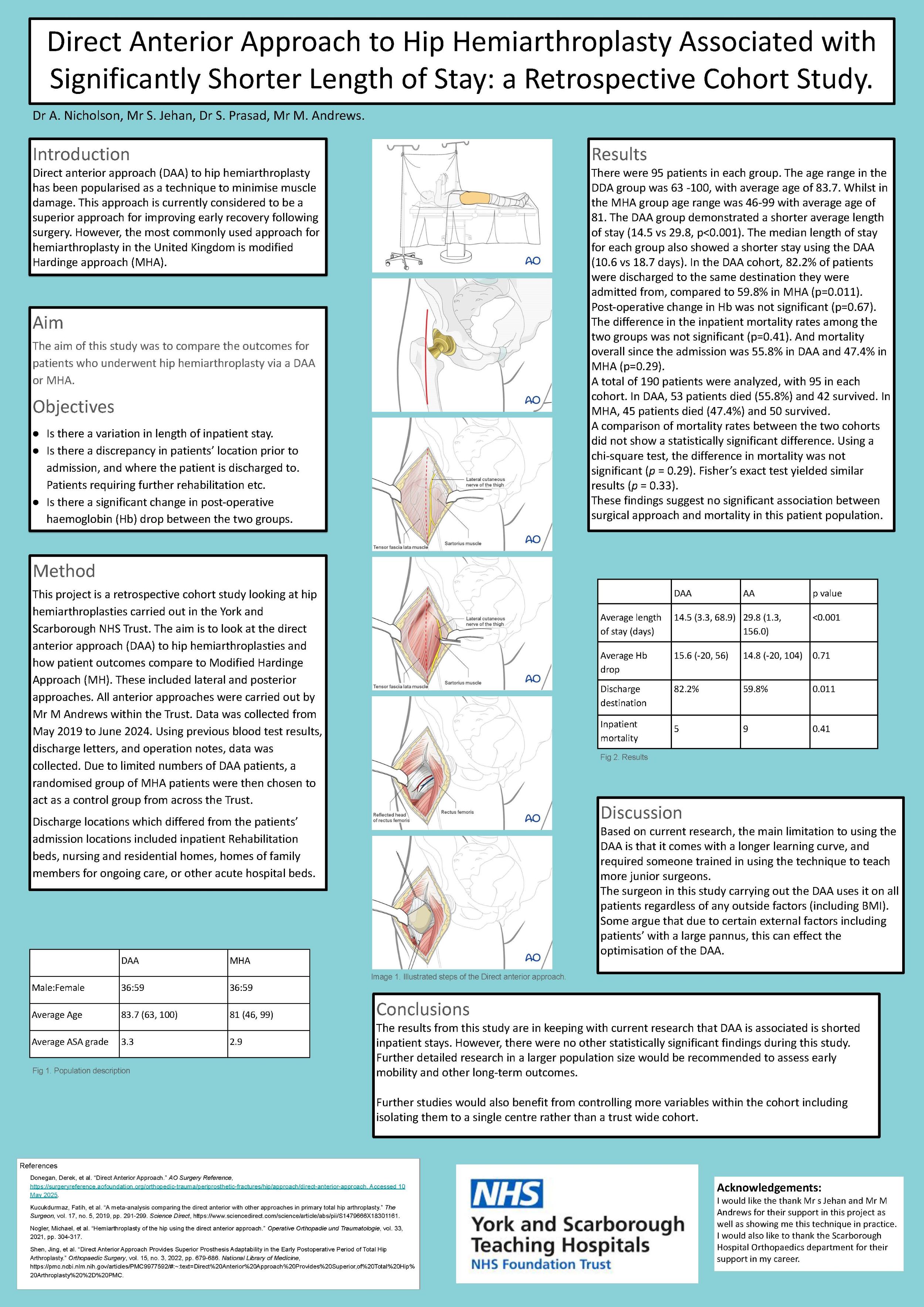
623 - Direct Anterior Approach to Hip Hemiarthroplasty Associated with Significantly Shorter Length of Stay: a Retrospective Cohort Study.
Alice Nicholson, Shah Jehan, Surya Prasad, Mark Andrews
York and Scarborough Teaching Hospitals NHS Trust, Scarborough, United Kingdom
Introduction: Direct anterior approach (DAA) to hip hemiarthroplasty has been popularised as a technique to minimise muscle damage. is currently considered to be a superior approach for improving early recovery following surgery. However, the most commonly used approach for hemiarthroplasty in the United Kingdom is modified Hardinge approach (MHA).
The aim of this study was to compare the outcomes for patients who underwent hip hemiarthroplasty via a DAA or MHA.
Methods: A retrospective analysis was conducted on patients in our institute who underwent hip hemiarthroplasty between May 2019 and June 2024. Patients were grouped into DAA or MHA. A total of 95 patients were identified in whom DAA was used. We then selected 95 age and gender matched patients who had hemiarthroplasty via MHA. Primary outcomes included post-operative Hb changes, length of hospital stay, and discharge destination. Secondary outcomes included mortality rates.
Results: There were 95 patients in each group. The average age in the DDA group was 83.7 (63-100). The average age for MHA group age was 81 (46-99). The DAA group demonstrated a shorter length of stay (14.5 vs 29.8, p<0.001). In the DAA cohort, 82.2% of patients were discharged to the same destination they were admitted from, compared to 59.8% in MHA (p=0.011). Post-operative change in Hb was not significant (p=0.67). The difference in the inpatient mortality rates among the two groups was not significant (p=0.41). And mortality overall since the admission was 55.8% in DAA and 47.4% in MHA (p=0.29).
Discussion: The results from this study are in keeping with current research that DAA is associated is shorted inpatient stays. However, there were no other statistically significant findings during this study. Further detailed research in a larger population size would be recommended to assess early mobility and other long-term outcomes.
626 - A comparative analysis of four surgical approaches to total hip replacements: a propensity matched study
Nimra Akram1, Sai Pendyala1, Ameen Ahamad2, Irrum Afzal1, Sarkhell Radha1,2
1South West London Elective Orthopaedic Centre, London, United Kingdom. 2Croydon University Hospital, London, United Kingdom
Total hip replacement (THR) is a common and highly successful orthopaedic procedure, but the optimal surgical approach is debated.
Whichever approach is used, the primary goals of the surgery is pain relief and enhancement in the quality of the patient's life suffering from hip pathologies. To further understand the advantages and potential pitfalls associated with different surgical approaches, we compared the outcomes of three widely used approaches: anterolateral, direct anterior and posterior - against a minimally invasive, piriformis- and quadratus femoris-sparing posterior approach (MIS). A total of 600 patients (150 per each approach) undergoing THR between 2017 and 2022 were included. All patients were propensity-matched to account for confounding variables like age, sex, BMI, ASA grade, preoperative scores and grade of osteoarthritis. Primary outcomes included Oxford Hip and EQ5D scores, patient satisfaction at 6-weeks and 6-months, length of hospital stay, re-admission rates and complication rates. Radiological analysis was conducted on pre-operative and immediate post-operative x-rays comparing factors such as leg length discrepancy, global offset, cup version, cup inclination and stem alignment. The MIS posterior approach showed higher Oxford Hip Scores (42.88) and EQ-5D scores with greater pre-to-post-operative improvements compared to the other approaches. However, no statistical significance was found in scores or mean improvements at 1 and 2 years. Outcome satisfaction at 6 months was 97.10 for the MIS posterior approach, 97.04 for direct anterior, and 96.18 for anterolateral, with no significant differences. The MIS approach had a significantly shorter hospital stay (1.3 days, P<0.005) in comparison to the other three approaches. This study demonstrates the post-operative outcomes and advantages of a muscle-sparing posterior approach to traditional THR approaches. However further work with a larger patient cohort is needed to validate these encouraging findings
716 - Total Hip Arthroplasty Restores Population Health Related Quality of Life Norms: A Propensity-Matched Study with Mediation Analysis of BMI
Andrew Ablett, Liam Yapp, Nick Clement, Chloe Scott
Royal Infirmary of Edinburgh, Edinburgh, United Kingdom
Background
This study compares health-related quality of life (HRQoL) between patients undergoing primary total hip arthroplasty (THA) for osteoarthritis (OA) and a propensity-matched general population cohort. We also aimed to clarify the relationship between body mass index (BMI) and postoperative improvements, mediated via preoperative HRQoL.
Methods
In this retrospective case-controlled study using the Edinburgh Arthroplasty database (2013-22; n=3495) and Health Survey for England (2010-12; n=25,320), propensity score matching (1:1) was performed based on age, sex, and BMI. The primary outcome was EQ-5D-3L index score. Secondary outcomes included EQ-VAS and mediation analysis examining how preoperative EQ-5D-3L mediated the relationship between BMI and postoperative improvement.
Results
Preoperatively, THA patients had significantly lower EQ-5D-3L scores compared with matched general population (median difference: 0.280, bootstrapped 95% confidence intervals; 0.258 to 0.306; p<0.001). At one-year follow-up, THA patients exceeded population norms (THA median: 0.814 vs. general population: 0.796, p=0.014). Patients >85 years showed the greatest relative improvements compared with the age-matched general population (THA median: 0.796 vs. general population: 0.696, p=0.142). Mediation analysis revealed that BMI's negative direct effect on improvements in EQ-5D-3L was counterbalanced by stronger indirect effects transmitted through preoperative scores (indirect effects: Obesity I (30-34.9kg/m2): β=0.048, p<0.01; Obesity II (35-39.9kg/m2): β=0.108, p<0.001; Obesity III (³40kg/m2): β=0.151, p<0.001).
Conclusions
THA was shown to restore HRQoL to that expected of a matched normal population, but in younger patients this was less than expected, whereas this was exceeded in older patients. Postoperative HRQoL improvement was predominantly influenced by preoperative functional status, rather than BMI alone. These findings challenge current BMI based eligibility thresholds and support surgical prioritization based on functional impairment severity.
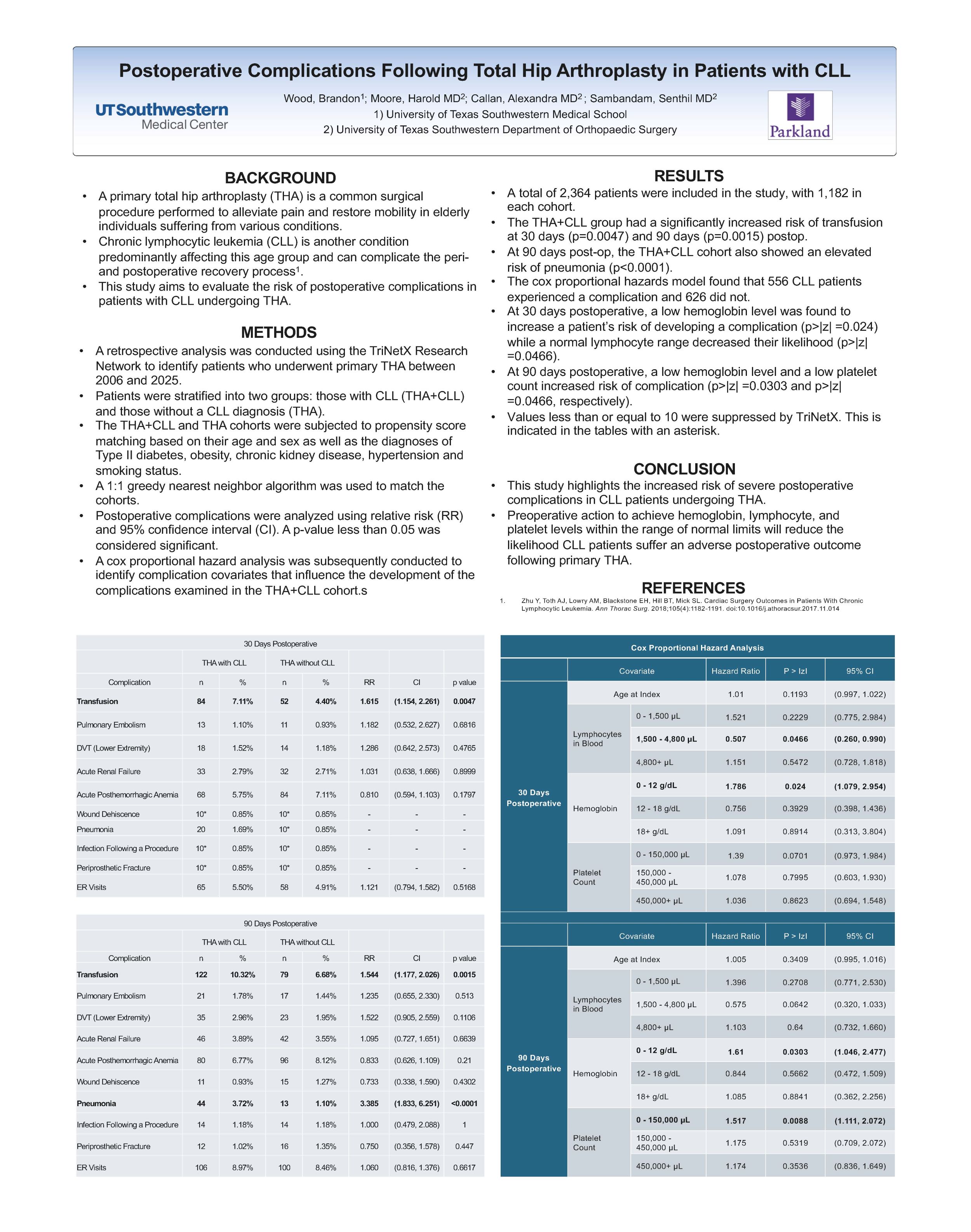
758 - Post-Operative Complications Following Total Hip Arthroplasty in Patients with Chronic Lymphocytic Leukemia
Brandon Wood, Gregory Moore, Senthil Sambandam
UT Southwestern Medical Center, Dallas, USA
Introduction: Total hip arthroplasty (THA) is a surgical procedure performed to alleviate pain and restore mobility in elderly individuals. Chronic lymphocytic leukemia (CLL) is another condition predominantly affecting this age group and can complicate the postoperative recovery process. This study aims to evaluate the risk of postoperative complications in patients with CLL undergoing primary THA.
Methods: We retrospectively analyzed primary THA patients (2005–2025) using the TriNetX Research Network, stratified into CLL (THA+CLL) and non-CLL (THA) groups. Propensity score matching was used to assess complications at 30 days, 90 days, 1 year, and 5 years postoperative. The THA+CLL cohort was further stratified into those patients that experienced complications and those who did not. Cox proportional hazard analysis identified complication covariates that influence the development of these complications.
Results: After matching, a total of 2,364 patients were included. The THA+CLL group had a significantly increased risk of transfusion at both 30 days (RR: 1.615; 95% CI: 1.154-2.261) and 90 days (RR: 1.544; 95% CI: 1.177-2.026) postoperative. These patients were also at an increased risk of developing pneumonia at 90 days (RR: 2.285; 95% CI: 1.833-6.251). We found that at 30 days postoperative, a hemoglobin level under 12 (HR: 1.786; 95% CI: 1.079-2.964) increased risk of complication while a normal lymphocyte range of 1,500 – 4,800 µL (HR: 0.507; 95% CI: 0.260-0.990) decreased their risk. At 90 days postoperative, a hemoglobin level less than 12 g/dL (HR: 1.613, 95% CI: 1.048-2.481) and a platelet count less than 150,000 µL (HR: 1.517; 95% CI: 1.111-2.072) increased risk of complication.
Conclusion: This study highlights the increased risk of severe postoperative complications in CLL patients undergoing THA. Tailored perioperative management, including enhanced fluid management, infection control, and close monitoring, is crucial to improving outcomes in this high-risk population.
793 - Longevity and Life Course Orthopaedics: Does Procedure Success Influence Long-Term Mortality Benefit after Primary Total Joint Arthroplasty?
Nicholas Sauder1, Danielle Blank2, Shian Peterson1, Tim Lindsay3,4, Anoop Prasad5, Christopher Melnic1, Hany Bedair1
1Massachusetts General Hospital, Boston, USA. 2Harvard Medical School, Boston, USA. 3London North West University Hospitals NHS Trust, London, United Kingdom. 4Imperial College London, London, United Kingdom. 5Chelsea and Westminster Hospital, London, United Kingdom
Background: Total joint arthroplasty (TJA) may improve not only joint-specific symptoms but also overall patient health. This may lead to a long-term mortality benefit for both total knee arthroplasty (TKA) and total hip arthroplasty (THA). Yet it is unclear whether the mortality benefit depends on the success of the procedure, which can be defined based on achievement of the minimal clinically important difference (MCID). This study investigated whether achieving the MCID after primary TJA is associated with improved long-term mortality.
Methods: A retrospective analysis was performed using a prospectively-maintained multi-institutional arthroplasty registry. The cohort included 1,382 primary TKAs and 1,076 primary THAs performed for osteoarthritis, with minimum 8-year follow-up. Procedure success was defined by achievement of literature-based MCID thresholds in the Knee or Hip Osteoarthritis Outcome Score Physical Function-Short Form (KOOS-PS or HOOS-PS). Kaplan-Meier survival curves and multivariable binary logistic regression models were used to evaluate the independent association between MCID achievement and 8-year mortality, adjusting for demographics and baseline health.
Results: MCID achievement was 67.8% for primary TKA and 73.5% for primary THA. In primary TKA, 8-year mortality rate was 3.3% for patients achieving MCID, and 4.2% for patients not achieving the MCID (p=0.705). In primary THA, 8-year mortality rate was 3.7% for patients achieving MCID, and 7.8% for patients not achieving MCID (p=0.028). MCID achievement remained associated with reduced 8-year mortality rate in primary THA after controlling for potential confounding variables (Odds Ratio=0.51; p=0.044).
Conclusion/Findings: Primary THA patients who achieve the MCID may derive a greater mortality benefit from the procedure, as compared to primary THA patients who do not achieve the MCID. The same correlation was not observed in primary TKA. The ability of primary THA to empower patients to lead longer, healthier lives may vary with how successful the procedure was.
Knee
61 - Impact of Psychological and Social Factors on Total Knee Arthroplasty - A Prospective Longitudinal Study
Joanne Brennan1, David Lennon2, Deirdre Desmond1, Aaron Glynn2
1National University of Ireland, Maynooth, Maynooth, Ireland. 2Our Lady's Hospital, Navan, Ireland
Background: Total knee arthroplasty (TKA) is an effective treatment to relieve pain and increase function for advanced osteoarthritis of the knee. However, after surgery some patients continue to experience pain, do not demonstrate anticipated functional improvements, and/or are dissatisfied with the outcomes. The aims of the current study were to investigate the relationship between preoperative psychosocial variables and rehabilitation engagement and TKA outcomes.
Methods: This was a prospective cohort longitudinal study. Patient reported data were collected at two time points: within 6 weeks before surgery (Time 1); and six months postoperatively (Time 2). Clinician rated data were collected during physiotherapy sessions. Rehabilitation engagement was rated by physiotherapists during the participant’s inpatient stay.
Results: Eighty-two participants were included at Time 1 and 46 were included at Time 2. Mental health, measured at Time 1, contributed significantly to the variance of postoperative patient satisfaction. Unfulfilled expectations, measured at Time 2, contributed significantly to the variance of postoperative pain intensity. No single psychosocial factor measured at time 1 was found to be predictive of patient satisfaction, however when considered as a whole through regression modelling they accounted significantly for the variance. There was no significant association between the psychosocial variables measured at Time 1 and rehabilitation engagement.
Conclusion: The findings of this study are consistent with previous studies in identifying that worse preoperative mental health is associated with patient satisfaction post-operatively in patients undergoing TKA. However, when individual psychosocial factors were examined, none appear to be significant predictors of PROMS on their own, despite accounting significantly for the variance when considered as a whole. This suggests that the interplay of psychosocial factors and reported outcomes is complex and is indicative of the importance of considering preoperative psychosocial factors. Preoperative screening could help to identify at-risk patients and offer opportunities for preoperative interventions.
69 - Comparison of Early Results Between Bone-Conserving and Conventional High-Flexion Posterior-Stabilized Total Knee Arthroplasty
Eunjung Kim
The Joint Replacement Center of Seoul Metropolitan Government, SeoNam Hospital, Seoul, Korea, Republic of. Department of Orthopedic Surgery, Ewha Womans University, Seoul Hospital, Seoul, Korea
Young-Hoo Kim1*, Jang-Won Park2, Young-Soo Jang1, and Eun-Jung Kim1
1The Joint Replacement Center of Seoul Metropolitan Government, SeoNam Hospital, Republic of Korea; 2Department of Orthopedic Surgery, Ewha Womans University, Seoul Hospital, Republic of Korea
Abstract: The purpose of this study was to compare early clinical and radiographic results between bone-conserving and conventional high-flexion posterior-stabilized TKRA. Two hundred and eighty-five patients (477 knees; mean age, 68.7 years) received a NexGen Legacy posterior-stabilized high-flex (NexGen LPS-Flex) TKA and 280 patients (472 knees; mean age, 70.1 years) received a Freedom posterior-stabilized prosthesis. The mean follow-up was 3.5 (range, 2 to 5 years) for each group. The present study suggests that the early clinical and radiographic results of the bone-conserving Freedom TKA were similar to those of the conventional NexGen LPS-Flex TKA.
77 - Peripheral Nerve Stimulation HF-EMC Technology to Power an Implanted Neurostimulator with a Separate Receiver for the Treatment of Chronic Knee Pain after Total Knee Replacement
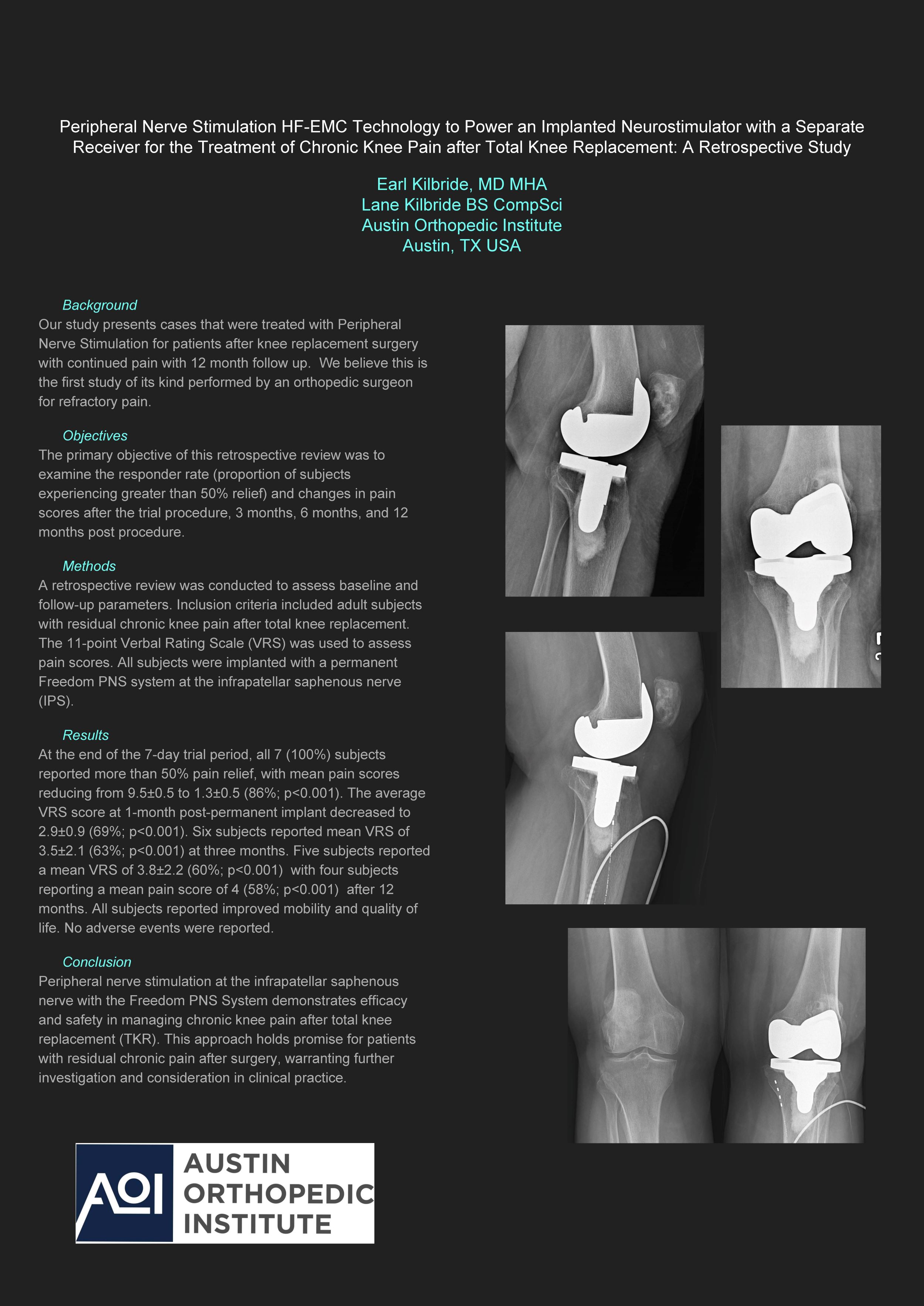
Earl Kilbride, Lane Kilbride
Austin Orthopedic Institute, Austin, TX, USA
Background: Our study presents cases that were treated with Peripheral Nerve Stimulation for patients after knee replacement surgery with continued pain with 12 month follow up. We believe this is the first study of its kind performed by an orthopedic surgeon for refractory pain.
Objectives: The primary objective of this retrospective review was to examine the responder rate (proportion of subjects experiencing greater than 50% relief) and changes in pain scores after the trial procedure, 3 months, 6 months, and 12 months post procedure.
Methods: A retrospective review was conducted to assess baseline and follow-up parameters. Inclusion criteria included adult subjects with residual chronic knee pain after total knee replacement. The 11-point Verbal Rating Scale (VRS) was used to assess pain scores. All subjects were implanted with a permanent Freedom PNS system at the infrapatellar saphenous nerve (IPS).
Results: At the end of the 7-day trial period, all 7 (100%) subjects reported more than 50% pain relief, with mean pain scores reducing from 9.5±0.5 to 1.3±0.5 (86%; p<0.001). The average VRS score at 1-month post-permanent implant decreased to 2.9±0.9 (69%; p<0.001). Six subjects reported mean VRS of 3.5±2.1 (63%; p<0.001) at three months. Five subjects reported a mean VRS of 3.8±2.2 (60%; p<0.001) with four subjects reporting a mean pain score of 4 (58%; p<0.001) after 12 months. All subjects reported improved mobility and quality of life. No adverse events were reported.
Conclusion: Peripheral nerve stimulation at the infrapatellar saphenous nerve with the Freedom PNS System demonstrates efficacy and safety in managing chronic knee pain after total knee replacement (TKR). This approach holds promise for patients with residual chronic pain after surgery, warranting further investigation and consideration in clinical practice.
82 - Comparative Outcomes, Indications, and Complications of Trochleoplasty in Moderate vs. Severe Trochlear Dysplasia – A Systematic Review and Meta-analysis of Over 1600 knees
Matthew Bellamy1, Jack Doyle1, James Murray2, Nikki Totton1,3, Graeme Hancock2, James Stoddard2, Matthew Hampton2
1The University of Sheffield, Sheffield, United Kingdom. 2Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom. 3Sheffield Centre for Health and Related Research, Sheffield, United Kingdom
Background: Trochleoplasty addresses patellar instability caused by trochlear dysplasia (TD), with strong evidence supporting its use in severe cases, but limited evidence for its use in moderate TD. The aim of this review and meta-analysis was to compare the outcomes of trochleoplasty in moderate and severe TD.
Methods: A systematic search of OVID Medline, EMBASE, and Cochrane Library was conducted through November 2024 using the term "Trochleoplasty." Two reviewers independently evaluated studies against inclusion criteria, which required trochleoplasty patients as complete cohorts or distinct subgroups. Studies were categorised by dysplasia severity: complete cohort, severe-only, mixed (>30% moderate), and non-severe. Analysis included weighted changes in outcomes scores, surgical indications, complications, and concurrent procedures. Random effects modelling generated pooled outcomes with 95% confidence intervals.
Results: Of 644 papers screened, 43 studies (67% retrospective) met inclusion criteria, comprising 1,621 knees in 1,470 patients (mean age 21.3 years, follow-up 5.9 years). Mean MINORs score was 9 (range 2-18). The severe only group comprised 7 papers, 16 included mixed severe/moderate dysplasia, and 5 had non-severe cases. Pooled post-operative Kujala scores were 86.2 (severe), 84.6 (mixed), and 81.6 (non-severe) with weighted improvements of 28.1, 24.7 and 18.0 points respectively. Mixed and non-severe groups underwent more concurrent procedures at primary surgery, with MPFL reconstruction performed in 43% (severe), 41% (mixed), and 50% (non-severe). Non-severe cases showed higher rates of instability, re-operation, and post-operative pain, but had lower rates of long-term cartilage degeneration. Major complications (death, infection, thromboembolism, neurological) remained low across all groups.
Conclusion: Trochleoplasty may produce superior outcomes in severe TD, gaining greater improvements in outcome scores, ultimately leading to better post-operative scores overall. However, improvements and post-operative outcomes are still reasonable in non-severe cases. Future studies are needed to strengthen conclusions, given the heterogeneity and bias alongside the factors leading to difference in outcomes.
86 - Does the Patellotrochlear Index Correctly Identify Patella Alta in Moderate and Severely Dysplastic Trochlears?
Harvey George1, Matthew Bellamy1,2, Kiran Madhvani1, Graeme Hancock1, James Stoddard1, Matthew Hampton1
1Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom. 2The University of Sheffield, Sheffield, United Kingdom
Background: While the Caton-Deschamps (CD) ratio remains the standard tibial-based measure of patellar height, the patellotrochlear index (PTI) is a newer technique which directly assesses patellofemoral articulation based on MRI. Despite PTI's reported increased accuracy in trochlear dysplasia, we hypothesise it underestimates patella alta in more moderate and severe trochlear dysplasia. This study evaluates PTI's diagnostic accuracy across varying trochlear dysplasia severities.
Methods: We conducted a retrospective radiographic analysis of cases from 2017-2024. Patients were identified through four surgical procedures: ACL reconstruction, trochleoplasty, MPFL reconstruction, and tibial tubercle transfer. Pre-operative knee radiographs and MRI scans were analysed. Cases were stratified by trochlear dysplasia severity using the Oswestry-Bristol Classification (OBC). Patellar height was assessed using both the PTI and CD ratio, while trochlear length was measured using the trochlear centre edge angle (TCEA) on MRI scans.
Results: Analysis of 120 scans revealed that the PTI and CD ratio showed comparable detection of patella alta in normal and mild dysplastic trochleas (OBC 1 and 2) (p >0.05). However, in moderate (OBC 3) and severe (OBC 4) dysplasia, agreement between measures significantly dropped to 30% and 40% respectively (p <0.05). PTI failed to detect 30% of cases that met CD ratio criteria for patella alta. Linear regression modelling suggested a novel PTI diagnostic threshold of 0.42.
Conclusions: Our findings demonstrate that the patellotrochlear index lacks diagnostic reliability for patella alta in patients with moderate and severe trochlear dysplasia. We propose a novel diagnostic threshold of 0.42 for PTI in these more dysplastic cases. Prospective validation studies with larger cohorts are needed to confirm the clinical utility and reproducibility of this modified diagnostic criteria.
Disclosures: The authors declare no conflicts of interest in the conduct or reporting of this research. No external funding was received for this study.
91 - Key Predictors of Same Day Discharge after Medial Unicompartmental Knee Arthroplasty
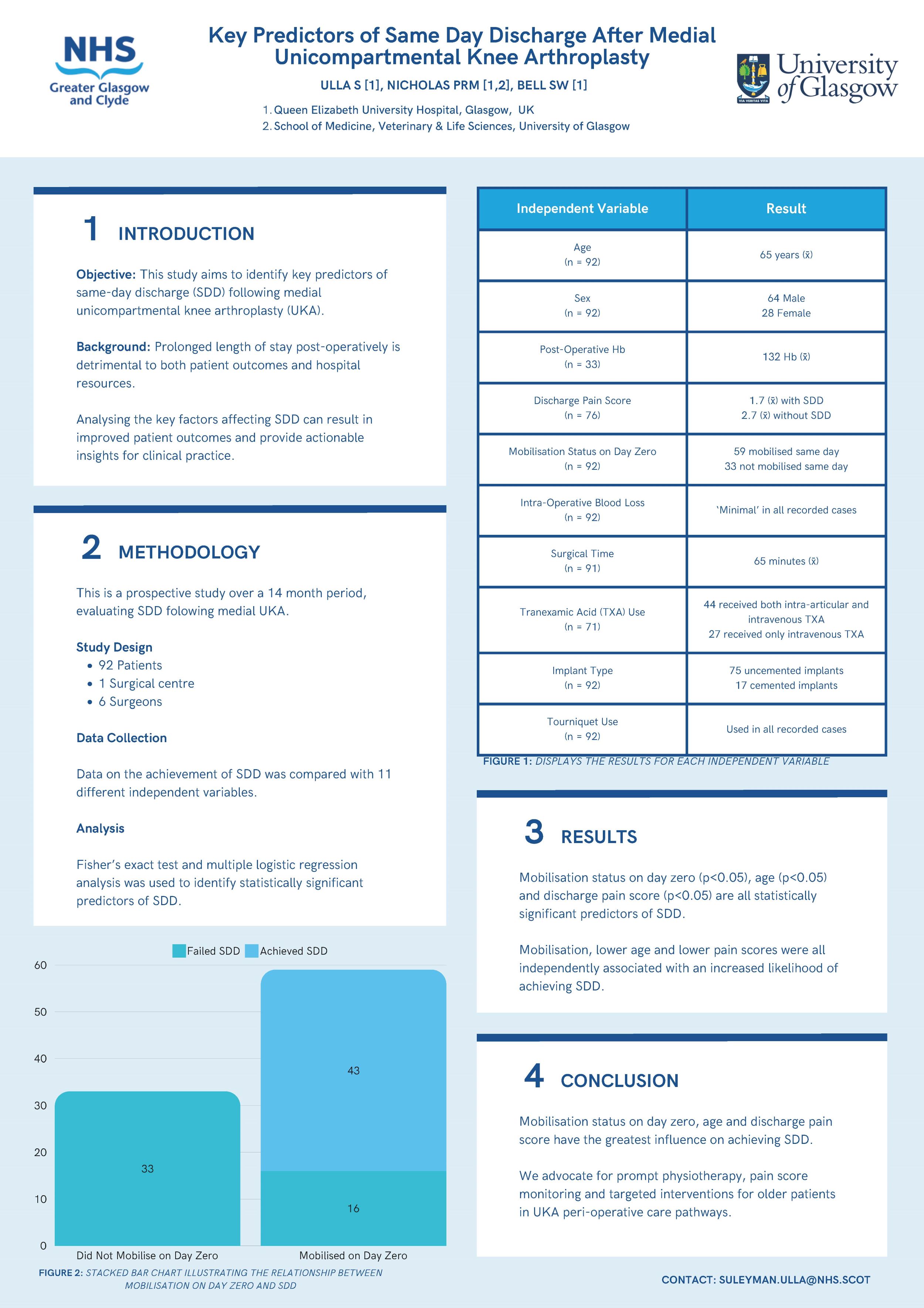
Suleyman Ulla1, Patrick RM Nicholas1,2, Stuart W Bell1
1Queen Elizabeth University Hospital, Department of Trauma & Orthopaedic Surgery, Glasgow, United Kingdom. 2College of Medicine, Veterinary and Life Sciences, University of Glasgow, Glasgow, United Kingdom
Aims: Prolonged bed stay post-operatively can lead to increased morbidity and complications. This study aims to identify significant predictors of same-day discharge (SDD) following medial unicompartmental knee arthroplasty (UKA).
Methods: A total of 92 patients who underwent medial UKA at a single elective surgical centre by 6 different surgeons was retrospectively evaluated over 14 months. Data on whether SDD was achieved was compared with patient and surgical factors. These were age, sex, pre- and post-operative haemoglobin (Hb), tourniquet use, surgical time, intra-operative blood loss, mobilisation on day zero, tranexamic acid (TXA) use, implant type and discharge pain score.
Results: 30% (28/92) patients were female. The median age was 65 years old. Post-operative Hb was recorded for 33 patients (M=134). A tourniquet was used for all patients. Surgical time was recorded for 91 patients (M=60 minutes). 59 patients were mobilised on day zero. TXA use was recorded for 71 patients. 44 patients received intra-articular and intravenous (IV) TXA and 27 patients received only IV TXA. 75 patients received uncemented implants. The median discharge pain score was 0 for patients with SDD and 2.0 for patients that failed SDD. 43 patients achieved SDD.
Fisher’s exact test and multivariable logistic regression analysis was performed, statistical significance was set as p < 0.05. Mobilisation on day zero, age and discharge pain score were statistically significant.
Conclusion: Mobilisation on day zero, age and discharge pain score are the best predictors of SDD. This indicates prioritisation of early mobilisation, pain score monitoring and targeted interventions for older patients in UKA peri-operative pathways.
97 - MRI-Based Assessment of Donor Site Healing Following Osteochondral Autograft Transfer Surgery (OATS): Evidence of Good Cartilage Regeneration At a mean Follow-up of 1.9 Years
Rakan Kabariti, Nicolas Dziadulewicz, James Richardson, Peter Gallacher, Paul Jermin
Robert Jones & Agnes Hunt Orthopaedic NHS Hospital, Oswestry, United Kingdom
Background: Healing of the donor site following Osteochondral Autograft Transfer Surgery (OATS) has not been evaluated. Magnetic Resonance Imaging (MRI) offers a promising method for assessing donor site recovery and cartilage regeneration following OATS. This study aims to evaluate donor site cartilage regeneration following OATS using MRI.
Methods: A database was used to identify OATS cases from a tertiary centre where patients had a post-operative MRI for various reasons. Patients who had additional cartilage regeneration procedures performed to the donor site were excluded. Patient demographics, operative techniques, donor and recipient sites were evaluated. The International Cartilage Society (ICRS) grading was used to classify the defects and a Magnetic Resonance Observation of Cartilage Repair Tissue (MOCART) 2.0 system was applied to determine the quality of cartilage regeneration at the donor site on the post-operative MR images by two independent assessors.
Results: 14 patients (mean age of 34 yrs.) met the inclusion criteria. The defects were located in the patella (36%), lateral femoral condyle (29%) and medial femoral condyle (36%) with a mean ICRS grade of 4. The mean time from surgery to the post-operative MRI was 1.9 yrs. (range 0.4 to 7.1 yrs.). 50% were performed on the left knee with a mean of 1 additional procedure performed at the time of index surgery. 43% and 48% had 8 mm and 10 mm plugs taken respectively. Donor sites included lateral (52%), central (29%) and medial (19%) trochlea. The median MOCART 2.0 score for all donor sites was 70 (range 35 – 90) with excellent inter-rater reliability (ICC=0.86).
Conclusion: Our findings show good robust donor site healing and effective cartilage regeneration following OATS, evidenced by MRI at a mean follow-up of 1.9 years. This provides re-assurance regarding the reliability of OATS at the donor site when treating cartilage defects.
100 - Outcomes of Meniscal Allograft Transplants: The Oswestry Experience
Rakan Kabariti, Peter Davies, Alexander Glover, Paul Jermin, Peter Gallacher
Robert Jones & Agnes Hunt Orthopaedic NHS Hospital, Oswestry, United Kingdom
Background: Meniscal allograft transplantation (MAT) is a viable option to improve pain and function in patients with symptomatic deficient menisci. The aim of this study is to report the outcomes of Meniscal allograft transplantations (MAT) performed over 10 years.
Methods: Consecutive MATs were identified from a prospective data base, done at a tertiary centre, between 2015-2024. Patient demographics, operative techniques used, length of stay (LOS), patient reported outcomes (Lysholm scores), follow-up and complications were retrieved. A post-operative Lysholm score < 65 was regarded as a clinical failure.
Results: A total of 56 MATs were identified with a mean patient age of 31 yrs (SD 6.7). 32% were females, 48% were right sided and 48% done to replace the medial meniscus. 55% have undergone additional procedures at the time of surgery – 13% Osteotomy, 18% ligament reconstruction, 32% cartilage regeneration and 8% combined. The mean (LOS) was 1 day (SD 1.2). 82% of the MATs were meniscus only and 18% used a bone block with a mean allograft donor age of 29 yrs (SD 16.6). Lysholm Scores improved from median 47 (SD 16.6) to median 82 (SD 24.8). 20% had a mechanical and/or clinical failure and 30% had subsequent surgery. 13% had a MAT tear confirmed on MRI and/or arthroscopy and 4% developed symptomatic arthritis which required a surgical intervention (osteotomy). The rate of infection, DVT, CRPS and stiffness was 2%, 2%, 2% and 7%, respectively.
Conclusion: Patients undergoing MATs demonstrated improvements in Lysholm score with an acceptable complication profile.
118 - Key factors influencing surgical outcomes in quadriceps tendon rupture A 16-year case series from a high-volume tertiary trauma centre
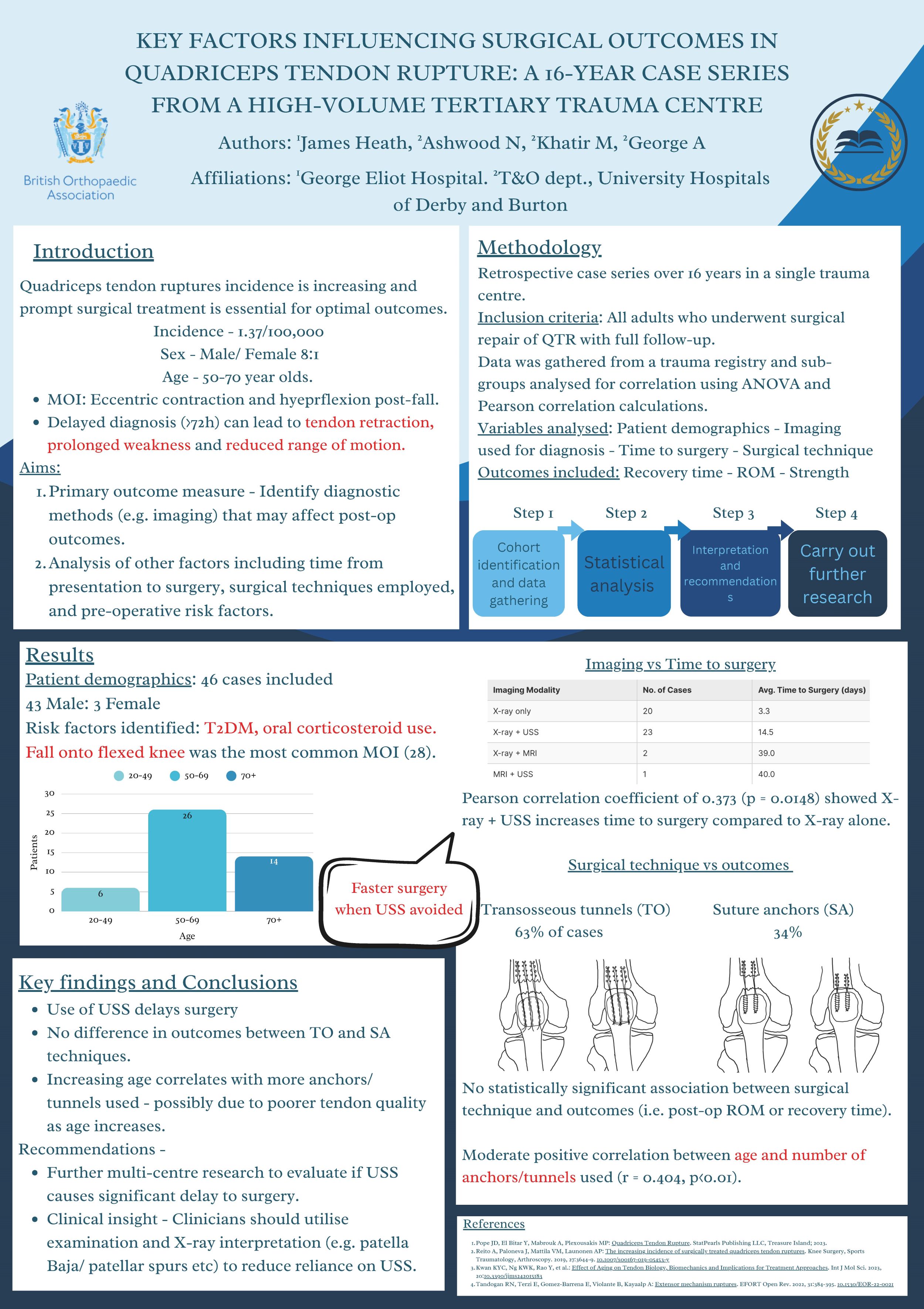
James Heath1, Neil Ashwood2, Mohammed Khatir2, Akhshay George2
1George Eliot Hospital, Nuneaton, United Kingdom. 2University Hospitals of Derby and Burton NHS foundation trust, Derby and Burton, United Kingdom
Background: Quadriceps tendon rupture (QTR) causes significant functional impairment, with recent studies showing an increasing incidence of these injuries. A delay in diagnosis significantly impacts outcomes, necessitating prompt diagnosis and treatment. This case series, spanning 16 years at a tertiary centre, examines factors influencing surgical outcomes, focusing on evaluating the correlation between diagnostic methods, time to surgery, surgical techniques, and post-operative outcomes.
Methods: An observational retrospective cohort study with data collected from a trauma registry and physiotherapy records. Study variables were identified through literature search and expert consultation. Data was gathered based on pre-, intra- and post-operative factors that could impact patient outcomes. Pearson correlation and ANOVA were used for statistical analysis (significance = p<0.05).
Results: Forty-six patients (predominantly males, aged 50-70 years) were included, with falls on a flexed knee the most likely aetiology. Choice of imaging significantly influenced time to surgery (TTS) (p=0.0148). A combination of X-ray and ultrasound (USS) proved most sensitive for diagnosis, though X-ray-only diagnosis resulted in shorter surgery wait times. TTS averaged 11 days, with over 52% waiting >72 hours. More than 90% of tears were osteotendinous with transosseous tunnels (TT) (63%) the predominant approach. No significant difference was seen in post-operative range of motion or recovery time between surgical techniques.
Conclusion: This series evaluates the impact of imaging modalities, surgical methods, and TTS on functional outcomes post QTR repair. Our results reinforce the male predominance and age-related risk of QTR. Comparable outcomes were observed across different surgical techniques, and surprisingly, early and delayed surgeries showed no differing effect on post-operative outcomes. We highlight the delay to surgery when USS is involved in the diagnostic work-up. Future research should investigate whether optimising clinical assessment and X-ray interpretation can negate the need for USS in diagnosis, thereby reducing wait times.
139 - Developing a Standardised Protocol for Management of Soft Tissue Knee Injuries to Improve Efficiency & Patient Outcome
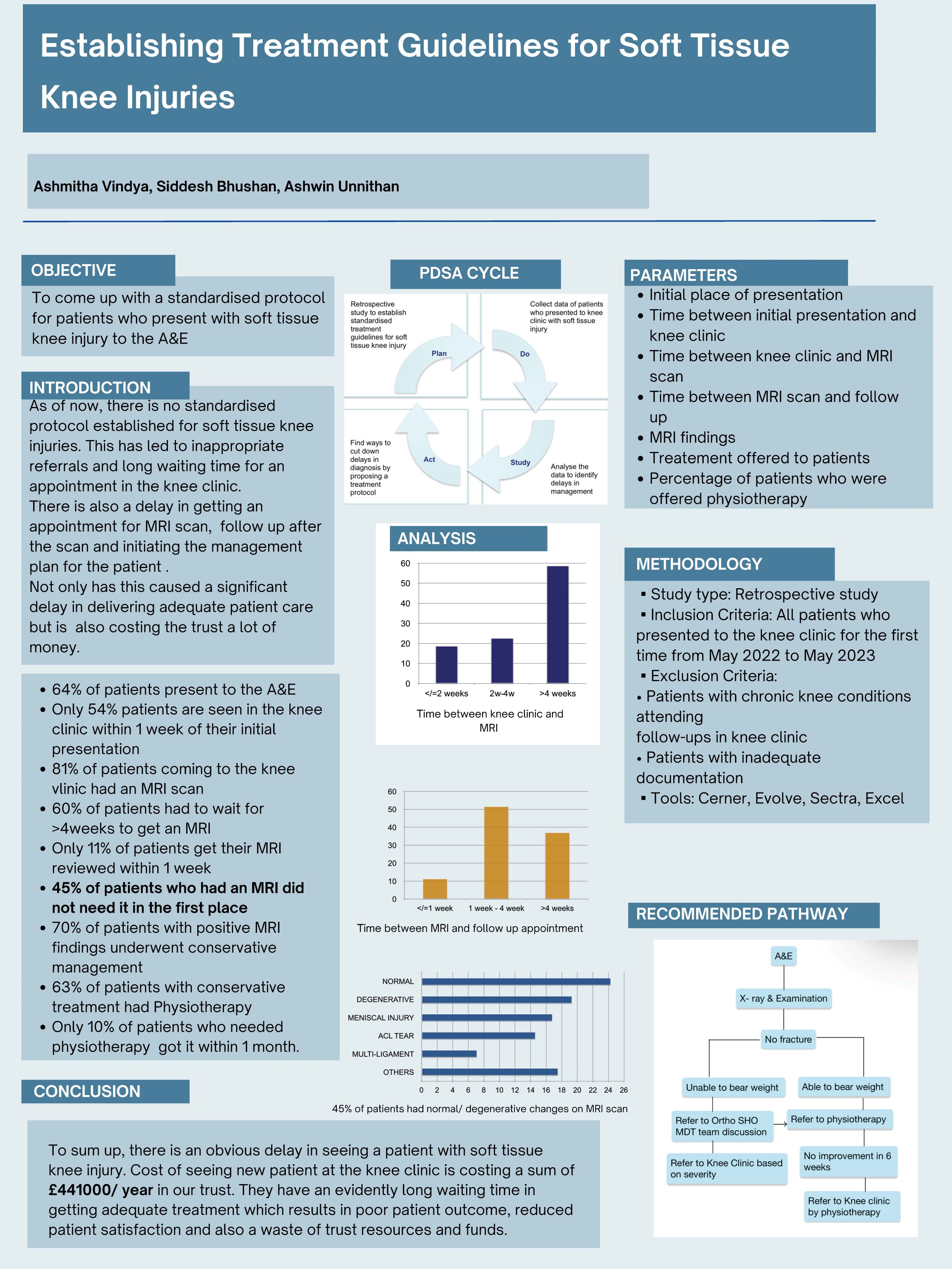
Ashmitha Vindya, Siddesh Nagabhushan
St Peter’s and Ashford Hospital NHS Trust, Woking, United Kingdom
Introduction/ Background: Soft tissue knee injuries (STKIs) are common presentations in emergency and orthopedic settings. However, there is no standardised protocol for their assessment and management, leading to delays in diagnosis, excessive MRI referrals, and inefficient use of resources.
Objective: This study aims to develop a standardised protocol to optimise patient care and reduce unnecessary MRI scans and clinic referrals.
Methodology: A retrospective study was conducted, analysing patients who presented to the knee clinic between January and May 2023. Patients with chronic knee conditions or inadequate documentation were excluded. The study assessed referral sources, time delays in imaging and diagnosis, and the effectiveness of MRI as a screening tool.
Results: Findings revealed that 81% of patients were referred for MRI, yet 45% of these did not necessarily need it. Nearly 60% waited over four weeks for MRI, and only 11% had results reviewed within a week. Most patients (82%) underwent conservative treatment despite 70% having positive MRI findings, with 63% receiving physiotherapy—yet only 10% accessed it within a month. The study estimated an annual cost of £441,000 for new patient consultations and MRI referrals. This opens up an opportunity to streamline referrals to knee clinic in order to reduce delays & save costs.
Conclusion: A structured STKI protocol, emphasising physiotherapy-led triage, could enhance care quality, reduce costs, and minimise delays in diagnosis and treatment
156 - Evaluating the impact of robotic assisted personalised alignment in TKA on coronal plane alignment and associated functional outcomes
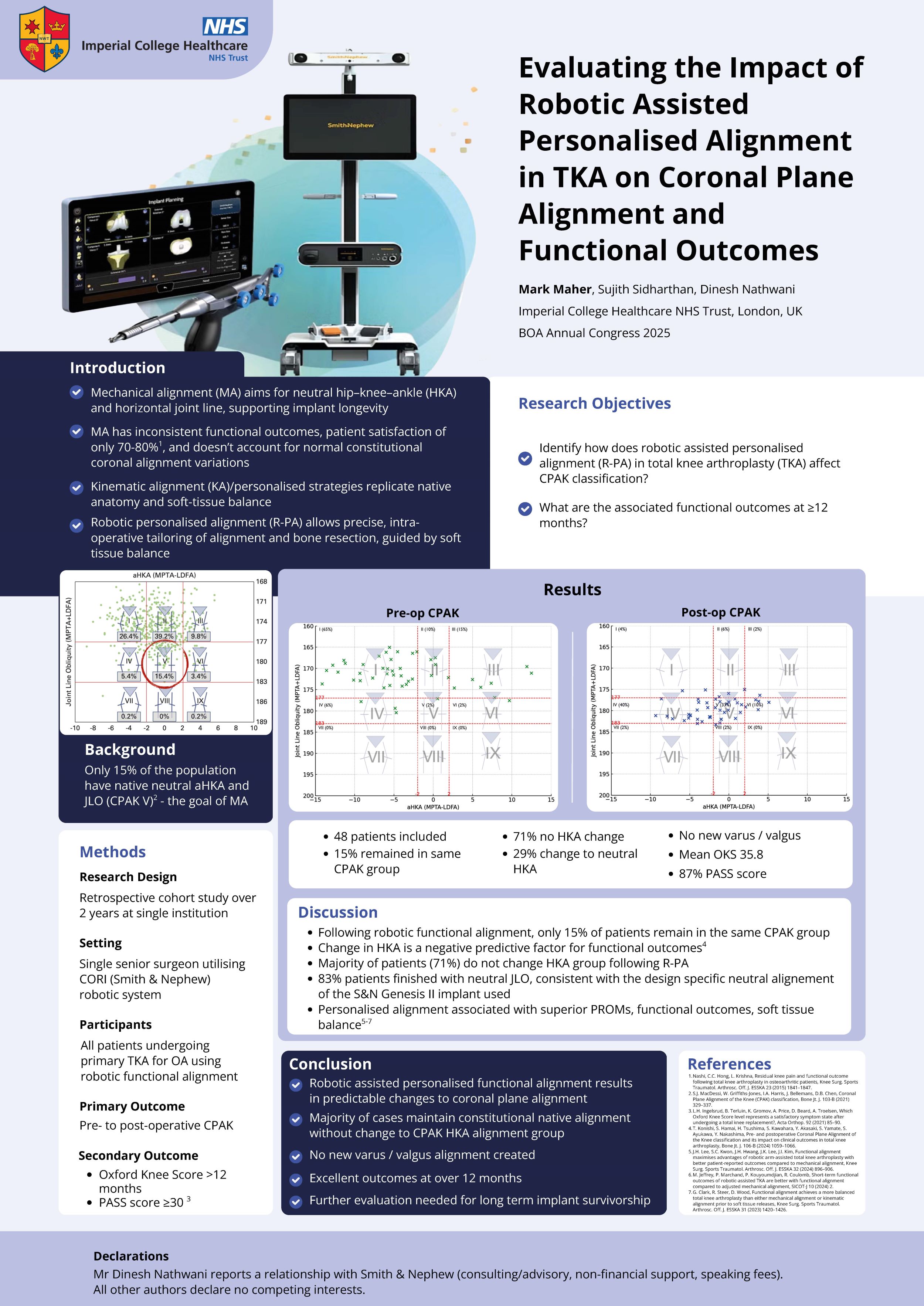
Mark Maher
Imperial College Healthcare NHS Trust, London, United Kingdom
Background: Traditional mechanical alignment (MA) in total knee arthroplasty (TKA) has long been the gold standard, targeting a neutral hip-knee-ankle (HKA) angle to enhance implant longevity. However, inconsistencies in functional outcomes and patient satisfaction have led to the emergence of personalized kinematic alignment strategies. This study evaluates the effects of robotic-assisted personalized alignment (R-PA) on coronal plane alignment of the knee (CPAK) and associated clinical outcomes.
Methods: A retrospective review was conducted on 48 patients who underwent primary TKA using the CORI Surgical System with R-PA from October 2021 to August 2023. CPAK classifications were assessed pre- and postoperatively, and functional outcomes were measured using the Oxford Knee Score (OKS) at a minimum of 12 months.
Results: Preoperatively, CPAK phenotype I (varus & apex distal joint line) was most common (65%), predominantly transitioning to type IV (varus & neutral joint line) (40%) following R-PA. Most patients (71%) maintained their HKA alignment category, and all other HKA category deviation resulted in neutral alignment. Postoperative joint line obliquity (JLO) shifted toward neutrality in 83% of cases. Mean OKS was 35.8, with 87% achieving a patient-acceptable symptom state (PASS).
Conclusion: R-PA in TKA results in predictable changes to CPAK, maintaining native constitutional alignment or transitioning to neutral aHKA without creating new varus/valgus alignment. This alignment strategy is associated with favorable functional outcomes scores at over 12 months follow up. Further large-scale and long-term randomized studies are warranted to assess implant survivorship and clinical outcomes.
Disclosure: Dinesh Nathwani reports a relationship with Smith and Nephew Inc that includes: consulting or advisory, non-financial support, and speaking and lecture fees. All other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
161 - Retrospective Comparative Review of Outcomes of Hamstring Autograft ACL Reconstruction With or Without Fibre Tape Supplementation
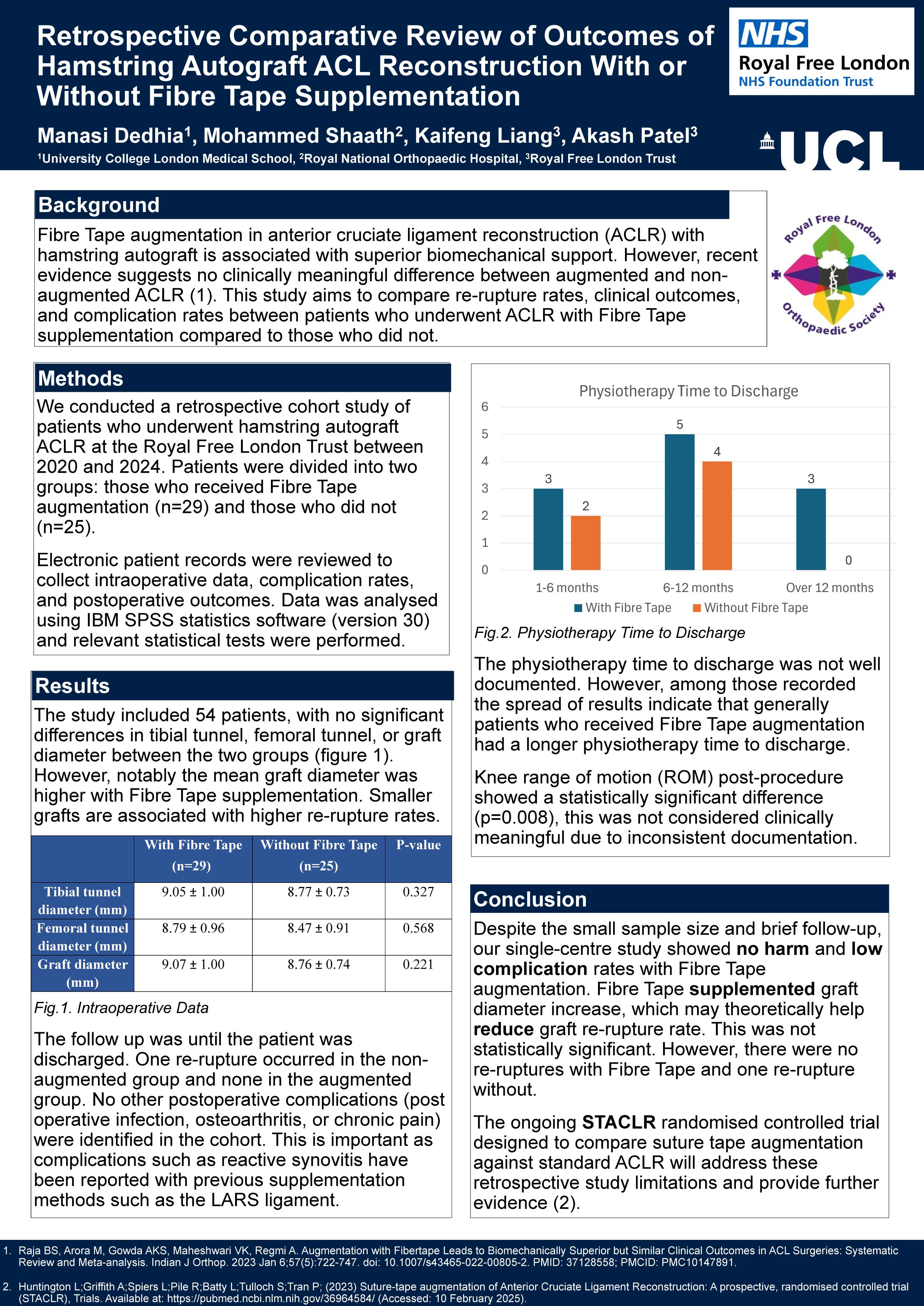
Manasi Dedhia1, Mohammed Shaath2, Kaifeng Liang3, Akash Patel3
1University College London Medical School, London, United Kingdom. 2Royal National Orthopaedic Hospital, London, United Kingdom. 3Royal Free London Trust, London, United Kingdom
Background: Anterior cruciate ligament reconstruction (ACLR), on occasion, can be augmented with Fibre Tape with the perception being that it provides increased biomechanical support. However, recently published evidence suggests no clinically meaningful difference between ACLR with Fibre Tape supplementation compared to those without. The purpose of this study is to compare re-rupture rates, clinical outcomes and complication rates following ACLR with Fibre Tape compared to ACLR without.
Methods: We conducted a retrospective cohort study comparing patients who received Fibre Tape augmentation with patients who did not receive Fibre Tape augmentation. The inclusion criteria for the study were all patients who underwent an ACL reconstruction with a hamstring autograft at the Royal Free London Trust between 2020 and 2024. Data was collected by reviewing the electronic patient records. Intraoperative data was collected, complication rates were reviewed and patient outcomes were extracted. Data was analysed using IBM SPSS statistics software (version 30).
Results: Fifty-four patients were included in the study. Of these, twenty-nine patients received augmentation with Fibre Tape and twenty-five patients did not. There was no statistically significant difference in tibial tunnel, femoral tunnel or graft diameter between the two groups (p=0.327, p=0.568, p=0.221). None of the patients in the cohort developed a post operative infection, osteoarthritis or chronic pain. A re-rupture occurred in one patient and they belonged to the group that did not receive augmentation with Fibre Tape. Knee ROM post procedure was significantly different between the two groups but there was no clinically meaningful difference (p=0.008).
Conclusion: This study did not demonstrate a clinically meaningful difference with Fibre Tape supplementation following ACLR surgery. This echoes existing literature; however, randomised controlled trials are awaited.
Implications: The use of Fibre Tape may be reconsidered due to the additional costs it bears.
Disclosure: No conflicts of interest.
171 - Comparative Proteomic Analysis of Proteins Involved in Knee Osteoarthritis using PROFASA Platform

Dragos Ioan Tabirca1, Anas El-Sibaei1, Yanlin Mi2
1CUH, Cork, Ireland. 2UCC, Cork, Ireland
Abstract: Osteoarthritis (OA), particularly Knee OA (KOA), is a significant cause of disability. To better understand KOA, this study characterised 21 key proteins previously implicated in its pathogenesis using Artificial Intelligence (AI). We employed the AI-driven PROFASA platform to predict their structures and calculate six crucial physicochemical parameters (including structural quality, hydrophobicity, stability, pI, molecular weight, and solvent accessibility) for these proteins based on their amino acid sequences. The analysis successfully generated structural models and a comprehensive physicochemical dataset for all 21 proteins. This work demonstrates the utility of AI tools like PROFASA for efficient protein characterisation, providing valuable data to accelerate future research into OA biomarkers, therapeutic targets, and drug development.
217 - The re-infection rate over time following two-stage revision knee arthroplasty for peri-prosthetic joint infection
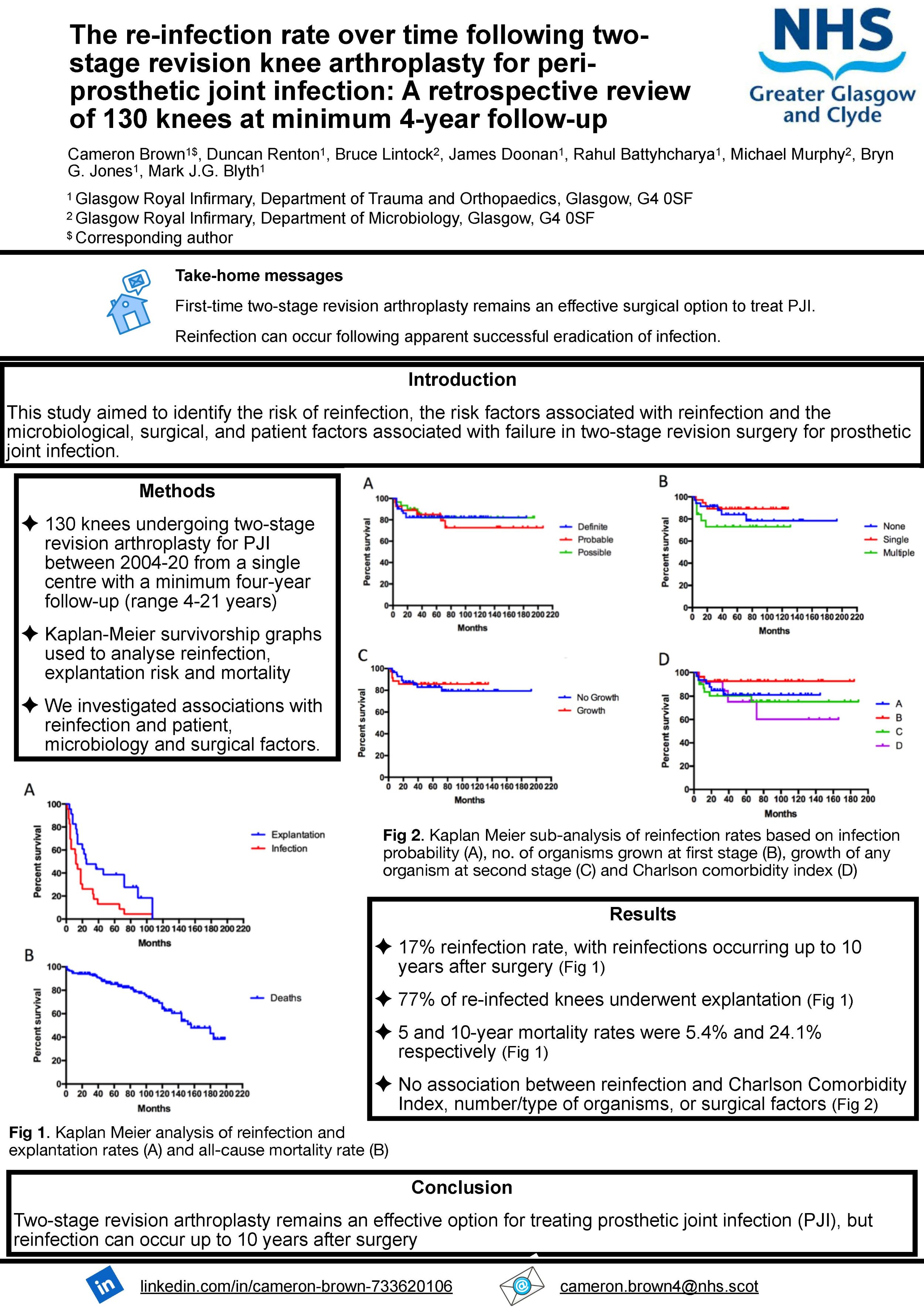
Cameron Brown, Duncan Renton, Bruce McLintock, James Doonan, Rahul Bhattyhcharyya, Michael Murphy, Bryn Jones, Mark Blyth
Glasgow Royal Infirmary, Glasgow, United Kingdom
Aims: This study aimed to identify the risk of reinfection, the risk factors associated with reinfection and the microbiological, surgical, and patient factors associated with failure in two-stage revision surgery for prosthetic joint infection.
Methods: 130 knees undergoing two-stage revision arthroplasty for prosthetic joint infection between 2004-20 from a single centre with a minimum four-year follow-up (range 4-21 years) were identified. Re-infection, the risk of prosthesis explantation and mortality were analysed using Kaplan-Meier survivorship graphs. Univariant and multivariate analyses were performed to identify any association between re-infection and patient, microbiological or surgical factors. Reinfection rates were compared for knees undergoing two-stage revision surgery for infection in patients following simple primary arthroplasty and those following revision arthroplasty surgery or where a complex primary had been carried out following fracture fixation.
Results: There was a 17% reinfection rate with reinfection occurring up to 10 years after the two-stage revision surgery. Of the re-infected knees, 77% underwent prosthesis explantation. The 5 and 10-year mortality rates were 5.4% and 24.1% respectively. The Charlson Co-morbidity Index, number or type of organisms, growth of organisms at second-stage, degree of bony defect or need for soft tissue flap coverage had no association with the risk of re-infection.
Conclusion: Two-stage revision arthroplasty remains an effective surgical option to treat PJI. Reinfection, however, can occur up to 10 years following apparent successful eradication surgery.
220 - Clinical differences in Patient Reported Outcome Measures between Kinematically Aligned Total Knee Replacement and medial Uni-condylar Knee Replacement; Systematic review and meta-analysis

Mohammed Elmajee1, Nandita J Nair2, Chathura Munasinghe3, Harriet Elson4, Nikolaides Anastasios5
1Queen Elizabeth Hospital, Birmingham, United Kingdom. 2University Hospital of North Midlands NHS trust, Stoke on Trent, United Kingdom. 3Harrogate NHS trust, Harrogate, United Kingdom. 4Leeds Teaching Hospital, Leeds, United Kingdom. 5Heartland Hospital, Birmingham, United Kingdom
Background: This systematic review and network meta-analysis compared patient-reported outcomes between kinematic-aligned total knee replacement (KA-TKR) and medial unicompartmental knee replacement (UKR). Historically, UKR has been associated with superior functional outcomes compared to traditional TKR, but advancements in kinematic alignment techniques may have narrowed this gap.
Methods: From an initial pool of 47 studies, 17 RCTs (1,554 patients) met inclusion criteria after rigorous manual screening. No automation tools were used in study selection. The analysis was performed using MetaXL v5.2 software with an Inverse Variance Heterogeneity (IVhet) model. Continuous outcomes (Oxford Knee Score, Forgotten Joint Score) were analyzed via Weighted Mean Difference (WMD), while differently scaled outcomes (Knee Society Score, KOOS subscales) used Standardized Mean Differences (SMD).
Results: No statistically or clinically significant differences were found between KA-TKR and UKR across all assessed metrics. The Oxford Knee Score showed a minimal non-significant trend favouring UKR (WMD 0.84, 95% CI: -1.68 to 3.37), while the Knee Society Score demonstrated negligible difference (SMD 0.012, 95% CI: -0.362 to 0.386). Similarly, KOOS subscales and Forgotten Joint Score revealed no meaningful advantage for either procedure, with only marginal, non-significant trends.
Conclusion/Findings: KA-TKR now provides functional outcomes comparable to UKR, closing the historical performance gap between partial and total knee replacements. These findings support individualized surgical decision-making, as both procedures yield excellent results when appropriately applied. Ongoing research is needed to refine long-term outcomes and patient selection criteria.
Disclosure: Nothing to disclose.
226 - Clinically Meaningful Thresholds in Patient-Reported Outcome Measures (PROMs) for Arthroscopic Meniscal Surgery A Systematic Review
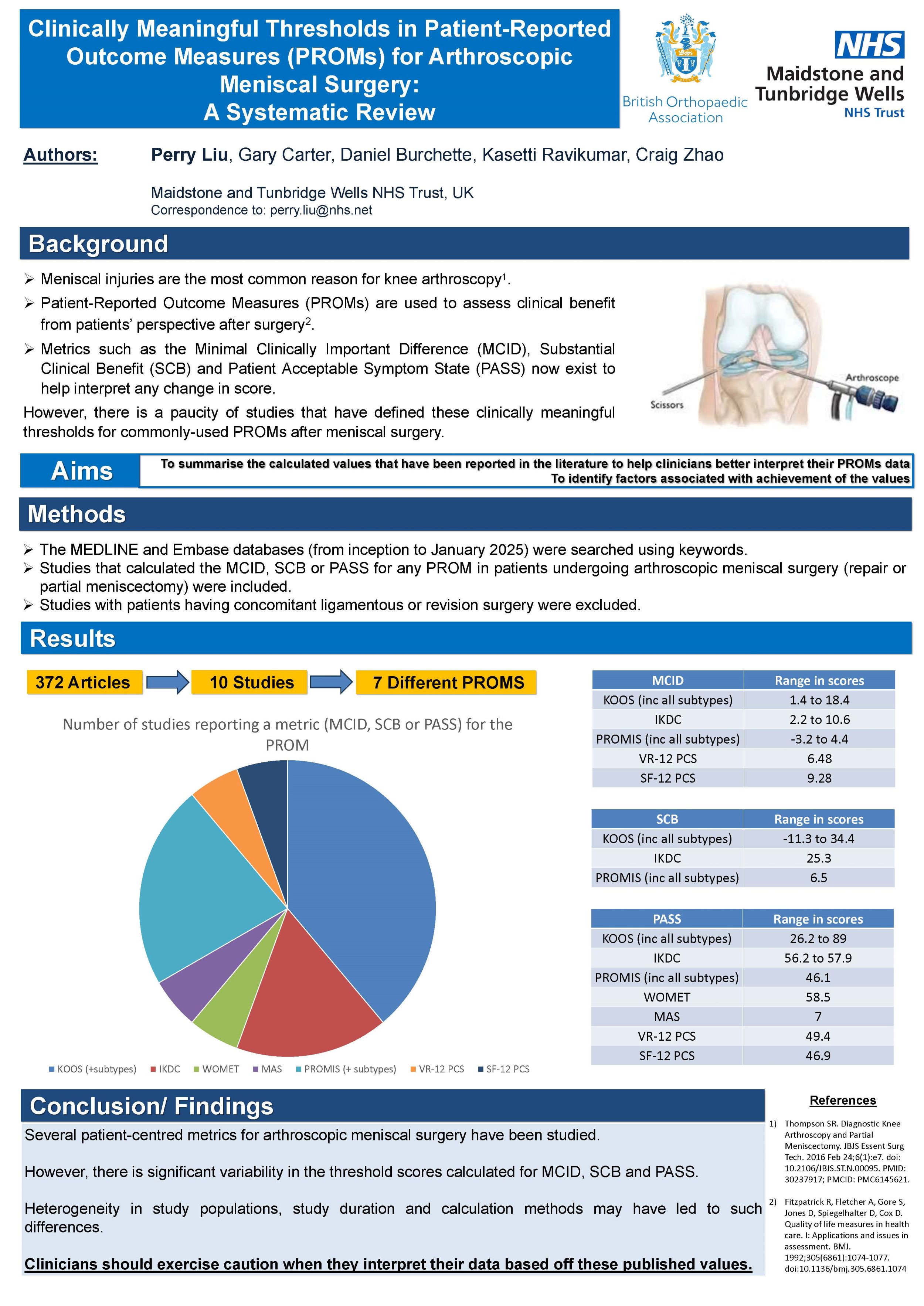
Perry Liu, Gary Carter, Daniel Burchette, Kasetti Ravikumar, Craig Zhao
Maidstone and Tunbridge Wells NHS Trust, Royal Tunbridge Wells, United Kingdom
Background: Meniscal injuries are the most common reason for knee arthroscopy. Patient-Reported Outcome Measures (PROMs) are used to assess clinical benefit from patients’ perspective after surgery. Psychometric measures such as the Minimal Clinically Important Difference (MCID), Substantial Clinical Benefit (SCB) and Patient Acceptable Symptom State (PASS) now exist to help interpret any change in score. However, there is a paucity of studies that have defined these clinically meaningful thresholds for commonly-used PROMs after meniscal surgery. The aim of this review was to summarise these values.
Methods: The MEDLINE and Embase databases (from inception to January 2025) were searched using keywords. Studies that calculated the MCID, SCB or PASS for any PROM in patients undergoing arthroscopic meniscal surgery (repair or partial meniscectomy) were included. Studies with patients having concomitant ligamentous or revision surgery were excluded. Relevant information was extracted and collated.
Results: 372 articles were screened and 10 studies (all Level 3 evidence), involving a total of 3436 patients, fulfilled the inclusion criteria. All studies assessed patients undergoing partial meniscectomy, with two also looking at meniscal repair. Seven different PROMs (including their subtypes) were investigated with the KOOS (n= 7) having the most threshold values reported for. MCID scores were reported in nine studies, SCB in three and PASS in six. For the most common PROM (KOOS), MCID values ranged from 6.4-10.4 (Symptoms subtype), 1.4-12 (Pain), 3.7-12 (ADL), 11.8-18.4 (Sport) and 3.1-15.6 (QoL). Similar variability was observed for SCB and PASS.
Conclusion/Findings: Several patient-centred metrics for arthroscopic meniscal surgery have been studied. However, there is significant variability in the threshold scores calculated for MCID, SCB and PASS. Heterogeneity in study populations, study duration and calculation methods may have led to such differences. Clinicians should exercise caution when they interpret their data based off these published values.
Disclosure: No conflicts.
248 - Effects of previous arthroscopic knee surgery on the outcomes of primary total knee arthroplasty a systematic review and meta-analysis
Desheng Wu
Bishan Hospital of Chongqing Medical University, Chongqing, China
Objective: The aim of this study was to evaluate the clinical effects of prior arthroscopic knee surgery on the prognosis of primary total knee arthroplasty (TKA).
Methods: A comprehensive literature search was performed in the PubMed, Embase, Cochrane Library, and other relevant databases up to December 2024. Cohort studies comparing the outcomes of patients with and without previous arthroscopic knee surgery were retrieved. Meta-analysis was performed to assess the differences in postoperative function, complications, and revision rates between the arthroscopy and primary TKA groups.
Results: The analysis included 10 cohort studies comprising a total of 172158 patients; 126732 of these patients had a history of knee arthroscopy. The meta-analysis results revealed no significant differences in postoperative range of motion, functional improvement, stiffness, periprosthetic fracture, venous thromboembolism (VTE), and other complications between the groups. However, the arthroscopic group showed a higher risk of postoperative prosthetic joint infection (PJI). The revision rate was also higher in the arthroscopic group (Relative Risk (RR) 1.304, 95% Confidence Interval (CI) 1.168 to 1.483). Subgroup analysis revealed an increased PJI risk within one year of arthroscopic TKA (RR 1.327, 95% CI 1.214 to 1.442). Sensitivity analysis confirmed the stability of the results, and Egger's test showed no publication bias.
Conclusion: Prior arthroscopic surgery was not found to have significant impacts on the functional outcomes of TKA but was found to increase the risks of postoperative infection and revision.
257 - Development of a complex intervention for people having knee replacement: My Knee Plan
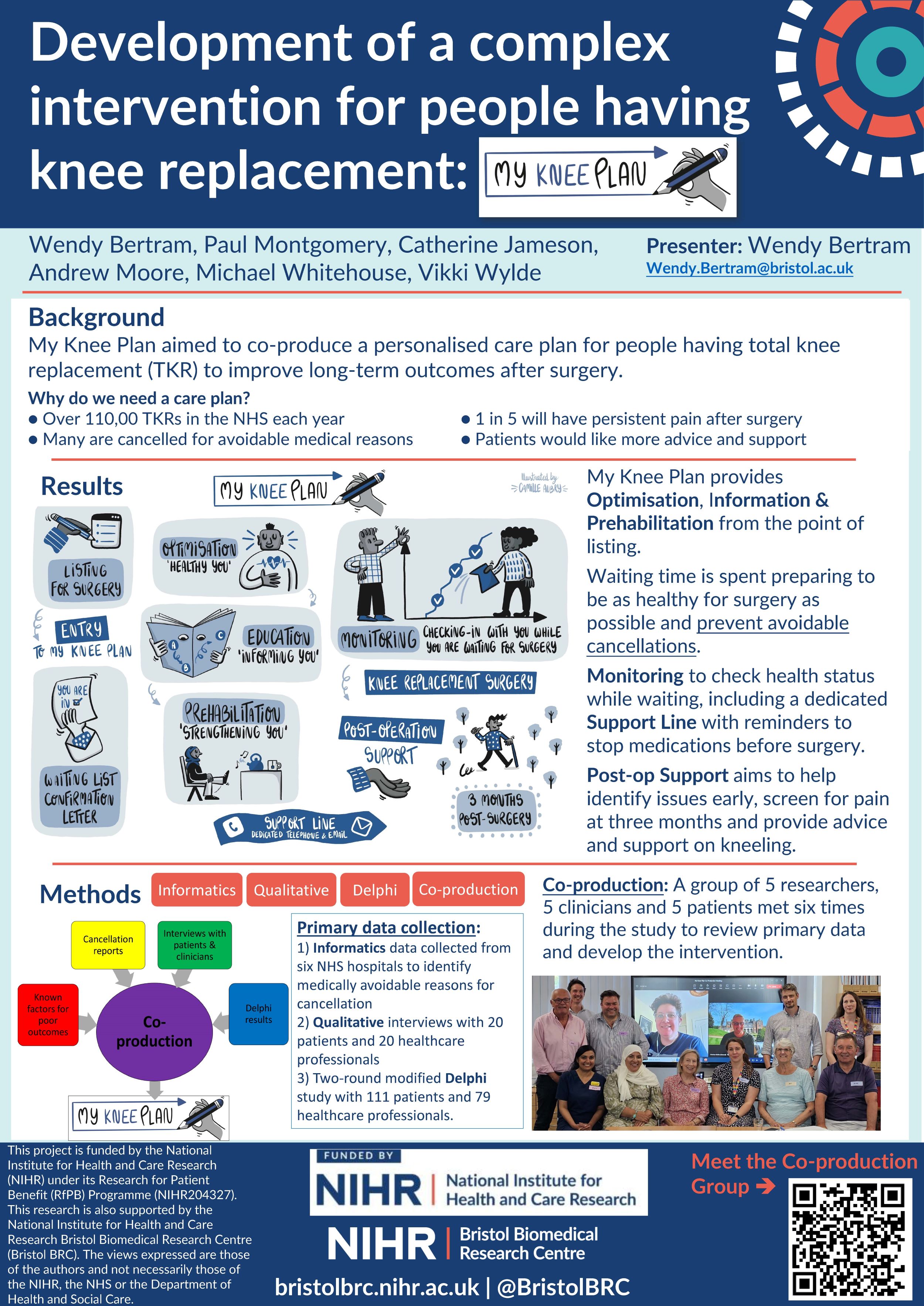
Wendy Bertram1,2, Paul Montgomery-Marks3, Catherine Jameson1,2, Andrew Moore1, Michael Whitehouse1,2, Vikki Wylde1,2
1University of Bristol, Bristol, United Kingdom. 2NIHR Bristol Biomedical Research Centre, Bristol, United Kingdom. 3University of Birmingham, Birmingham, United Kingdom
Background: Over 110,000 total knee replacements (TKRs) are performed annually in the UK. Many will have surgery cancelled at short notice after long waiting times. Typically, 20% of patients are dissatisfied and/or have chronic pain after surgery. Some feel abandoned post-surgery and would like more advice and support.
Delivering care with continuity from the point of listing through to recovery has the potential to reduce clinical cancellations and improve patient outcomes and satisfaction through provision of tailored optimisation, treatment, education and support.
This project used co-production to develop a care plan for TKR patients.
Methods: The intervention was co-produced by a group of 5 researchers, 5 health professionals and 5 patients, who met six times through the study. Intervention content was informed by primary data collection:
1. Informatics data collected from six NHS hospitals to identify medically avoidable reasons for cancellation
2. Qualitative interviews with 20 patients and 20 healthcare professionals
3. Two-round modified Delphi study with 111 patients and 79 healthcare professionals.
Results: My Knee Plan provides optimisation, information and prehabilitation from the point of listing, allowing patients to understand what they need to do to prepare and be as healthy as possible for their surgery and prevent avoidable cancellation. It continues to monitor patients while they wait, checking their health status with reminders to stop medication shortly before surgery, and provides support during recovery. It concludes at three months after surgery with advice and support on kneeling for those who need it, and screening for pain using the evidenced-based STAR care pathway.
Conclusion: We have developed a co-produced care intervention for patients undergoing TKR to optimise care from the point of listing until 3 months post-surgery. Further work is now needed to evaluate the clinical and cost-effectiveness of the My Knee Plan care pathway.
258 - What care for total knee replacement is important to patients and clinicians? The My Knee Plan modified Delphi Study
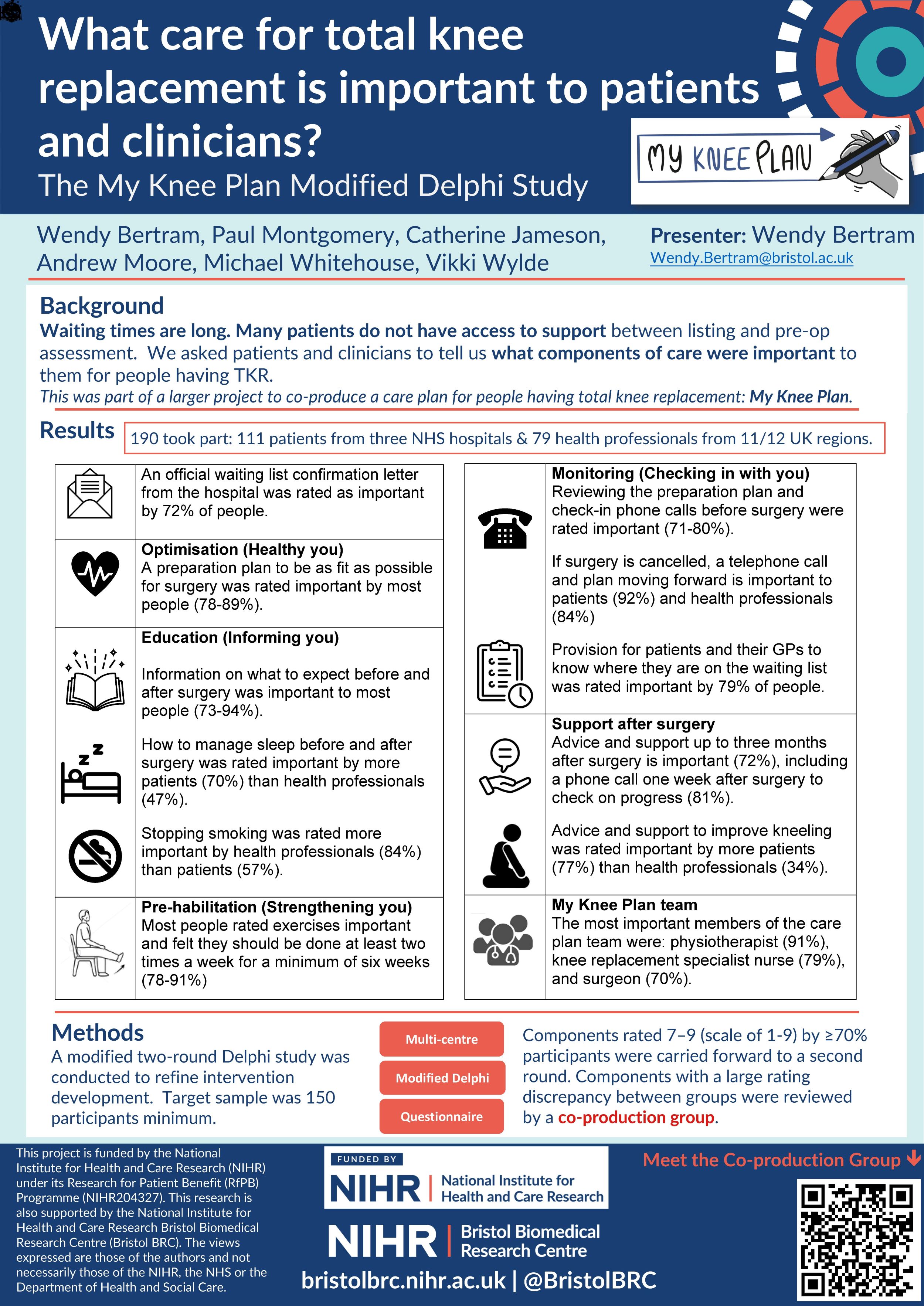
Wendy Bertram1,2, Paul Montgomery-Marks3, Catherine Jameson1,2, Andrew Moore1, Michael Whitehouse1,2, Vikki Wylde1,2
1University of Bristol, Bristol, United Kingdom. 2NIHR Bristol Biomedical Research Centre, Bristol, United Kingdom. 3University of Birmingham, Birmingham, United Kingdom
Background: Over 110,000 total knee replacements (TKRs) are performed annually in the UK. Waiting times have increased in the last five years. Many patients do not have access to advice or support between listing for surgery and pre-operative assessment. This project asked patients and clinicians what is important to include in a care plan for patients undergoing TKR.
Methods: Cancellation and interview study findings were collated into a preliminary list of care plan components. A modified two-round Delphi study was conducted to refine intervention development. Target sample was 150 participants minimum.
On a scale of 1-9, components rated 7–9 by ≥70% participants, or by ≥90% members of one panel, (and new suggestions) were carried forward to the second round. Components with a large rating discrepancy between groups were reviewed by a co-production group.
Results: 111 patients and 79 health care professionals took part. Both groups felt the following were important:
· Official waiting list confirmation letter
· Preparation plan to be as fit as possible for surgery
· Information on what to expect before and after surgery
· Exercises done at least twice weekly for six weeks minimum
· Monitoring with review of the preparation plan and check in phone calls
· If surgery is cancelled, a telephone call and plan moving forward
· Provision for patients and GPs to know where they are on the waiting list
· A phone call one week after surgery to check on progress
· Advice and support up to three months after surgery
Clinicians rated stopping smoking more important than patients.
Advice and support to improve both sleep and kneeling was rated higher by patients than by clinicians.
Conclusions: Most care components have consensus from both patients and clinicians, although patients rate some areas more important than clinicians. These findings could inform a new care plan for people having TKR.
274 - ‘A lot of patients have suffered for years, it is cruel’: the clinician perspective of waiting for and recovering from total knee replacement
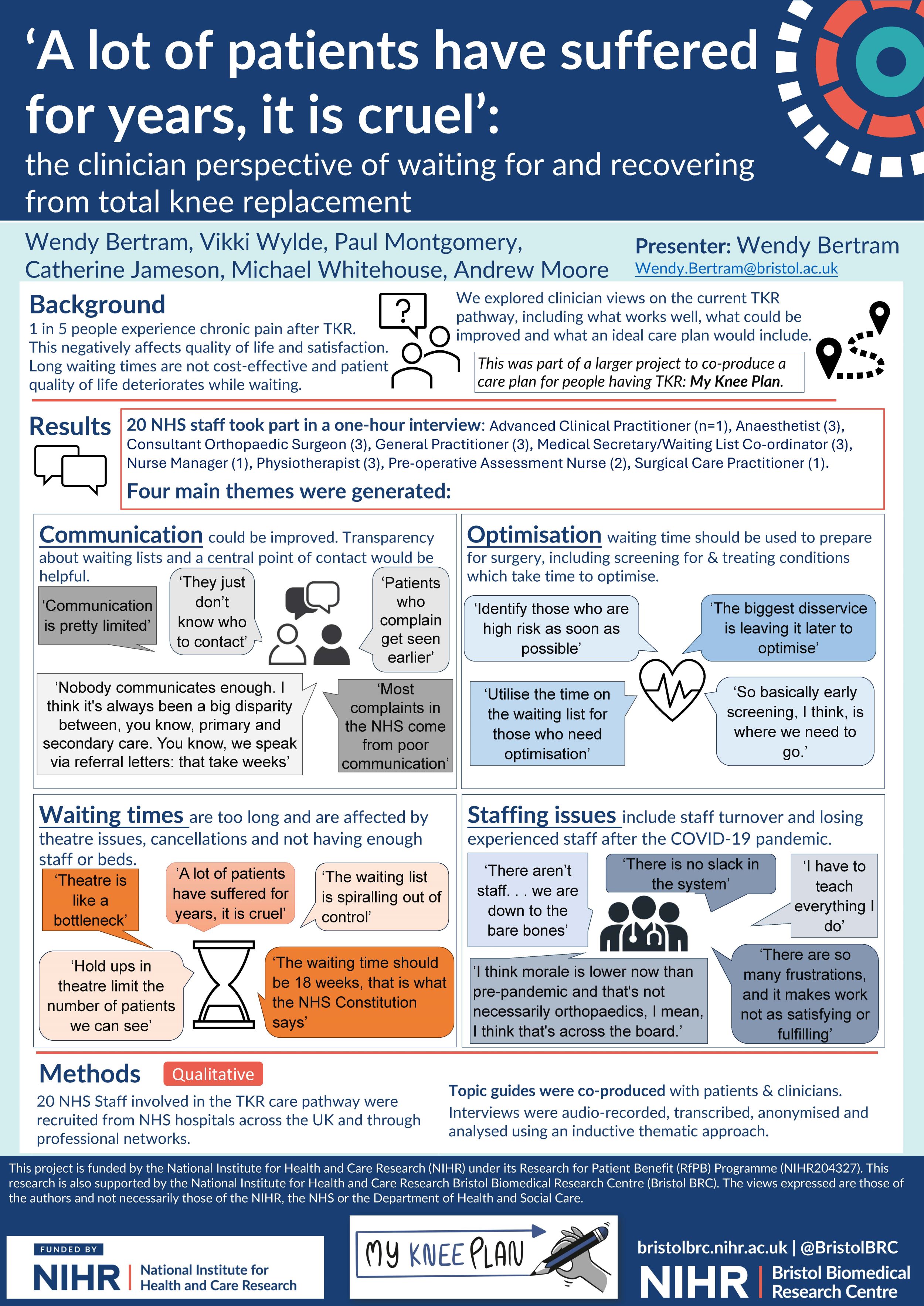
Wendy Bertram1,2, Vikki Wylde1,2, Paul Montgomery-Marks3, Catherine Jameson1,2, Michael Whitehouse1,2, Andrew Moore1
1University of Bristol, Bristol, United Kingdom. 2NIHR Bristol Biomedical Research Centre, Bristol, United Kingdom. 3University of Birmingham, Birmingham, United Kingdom
Background: Total knee replacement (TKR) is successful for most patients. However, 20% experience chronic pain after surgery which negatively affects quality of life and satisfaction. Waiting times for surgery have increased substantially in the last five years, with patient quality of life deteriorating while waiting.
We aimed to explore clinician views on the current TKR pathway, including continuity of care, patient optimisation and support, current demands on staff, and views on what an ideal care plan for TKR would include.
Methods: Twenty NHS staff involved in TKR care pathway were recruited from NHS hospitals and through our networks. Topic guides were co-produced with patients and clinicians.
Interviews were audio-recorded, transcribed, anonymised and analysed using an inductive thematic approach.
Results: Four main themes were generated:
· Communication: Communication could be improved between hospital departments, other healthcare providers, and with patients while they wait for and recover from surgery. Suggested improvements included a central point of contact, and transparency for patients about waiting times and how waiting lists work.
· Optimisation: To better prepare patients for surgery, the waiting period should be utilised to ensure fitness for surgery by screening for and treating health conditions which require time for optimisation, such as anaemia, uncontrolled diabetes and sleep apnoea.
· Waiting times: Common reasons for lengthy waiting times included not enough hospital staff or beds, and last-minute cancellations. Suggested improvements included early optimisation, adequate staffing, and ensuring teams work together consistently in theatre to improve efficiency.
· Staffing issues: Following the COVID-19 pandemic, increased staff turnover and loss of experienced staff was identified as a major cause of inefficiency.
Conclusion: Poor communication, missed opportunities for patient review and optimisation, and inefficiency in theatre use, compounded by staffing limitations, were highlighted as areas for improvement. There is a need for a new care plan to address these issues.
285 - Role of Arthroscopy in Management of Tibial Plateau Depression Fractures
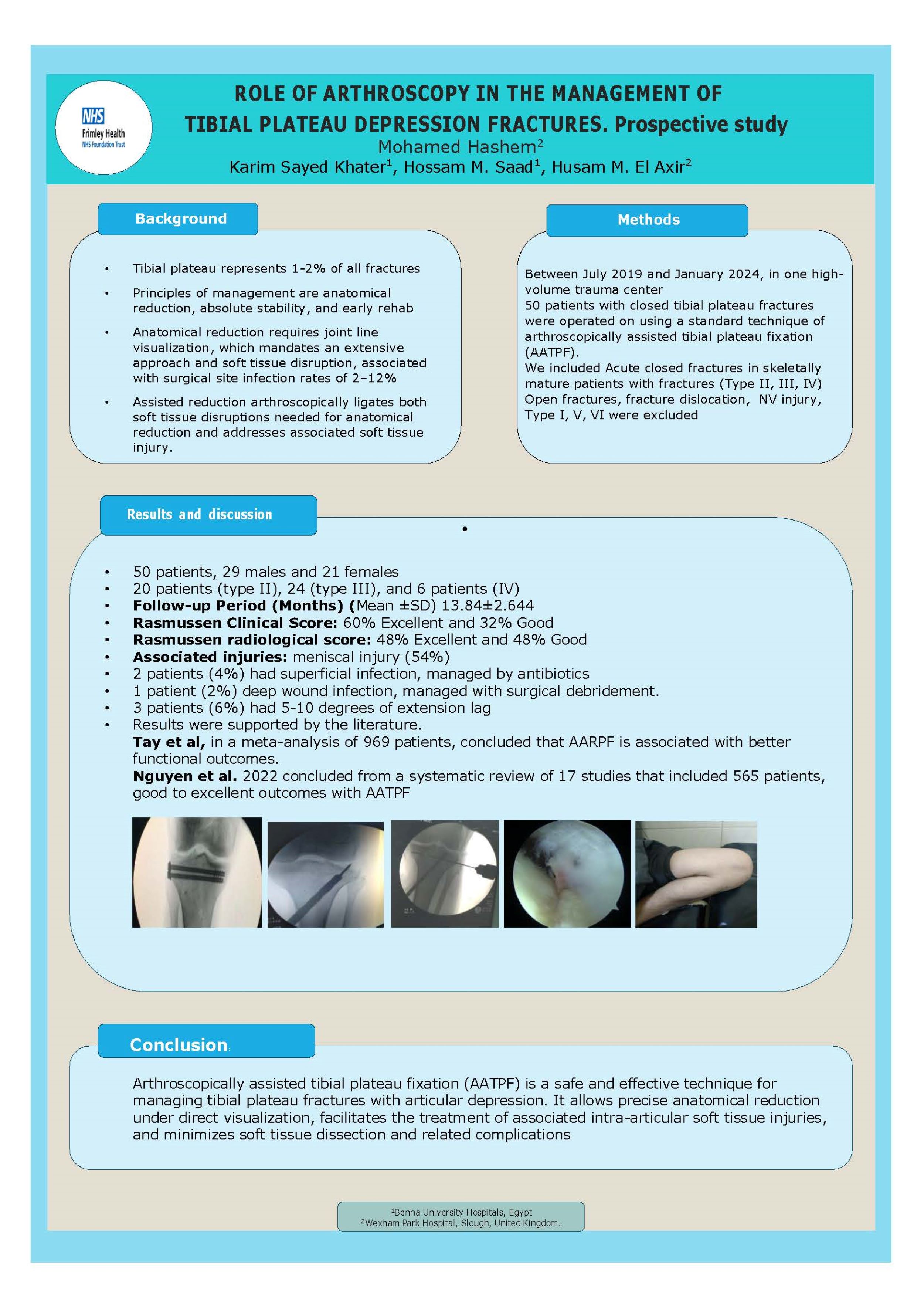
Karim Khater1, Mohamed Hashem2, Hossam Saad1, Hosam ElAxir2
1Benha faculty of medicine, Benha, Egypt. 2Frimley Health NHS Trust, Slough, United Kingdom
Background: Surgical intervention in tibial plateau fractures is the main modality of management with very limited role for conservative treatment. Open reduction and internal fixation (ORIF) is the standard treatment option but it has several complications so arthroscopic assisted fixation is a good alternative with many advantages.
Aim: To evaluate clinical and radiological results of arthroscopically assisted reduction and internal fixation of tibial plateau depression fractures. Patient and
Methods: It is a prospective study conducted between July 2019 and January 2024 in Benha University Hospitals included 50 consecutive patients with closed depressed tibial plateau fractures who had undergone arthroscopic assisted fixation. Results
The mean age of patients in this study was about 38 years old. According to Rasmussen clinical score 30 patients (60%) were excellent, 16 patients (32%) were good while only 4 patients was fair (8%). According to Rasmussen radiological score 24 patients (48%) were excellent, 24 patients (48%) were good while 2 patient were fair (4%).
Conclusion: Arthroscopy is a valuable tool for management of tibial plateau depression fractures with many advantages specially regarding fracture reduction and management of associated intraarticular injuries.
293 - Robotic Assisted Total Knee Arthroplasty with MAKO is Associated with Improved Functional Outcomes
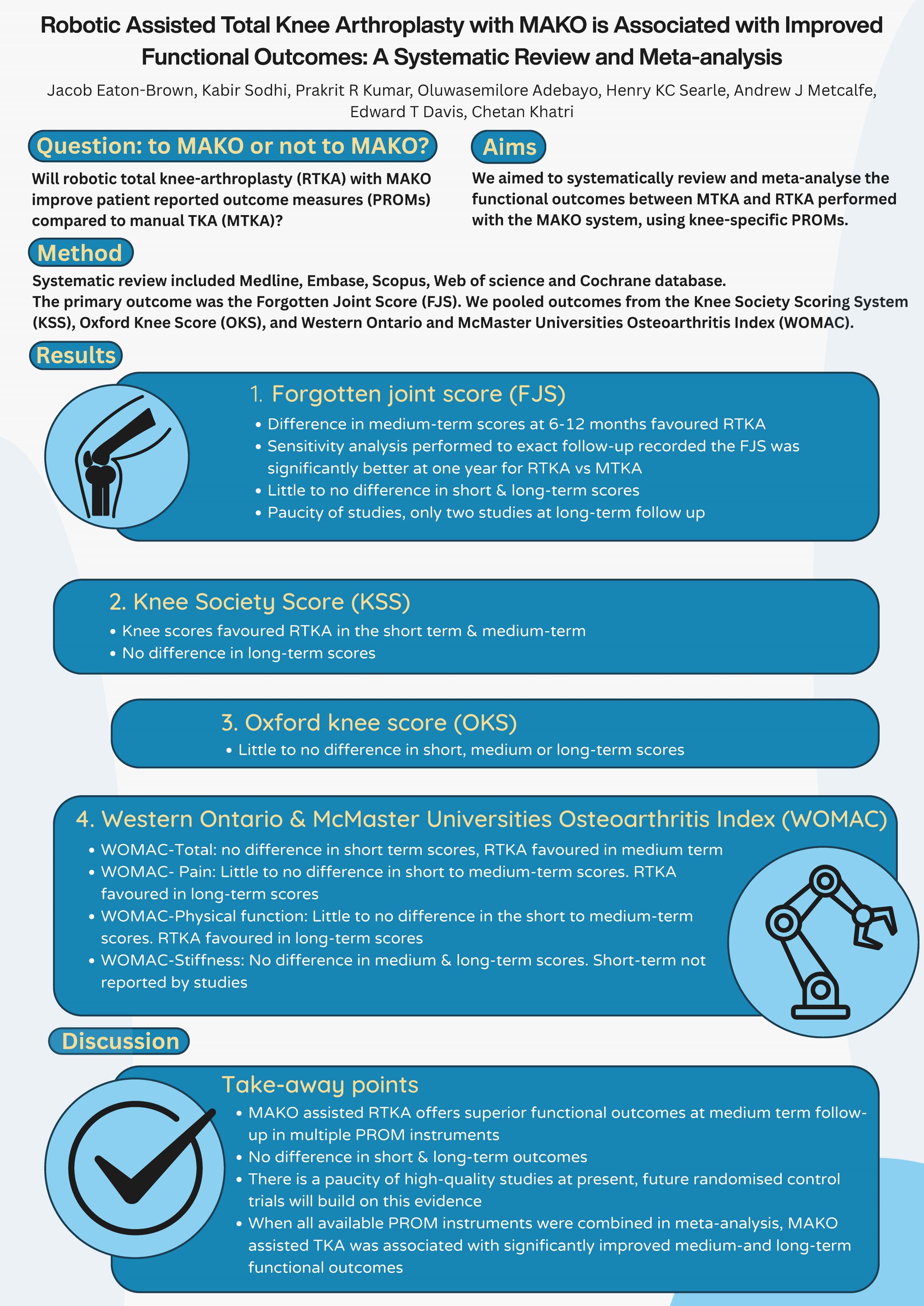
Kabir Sodhi1, Jacob Eaton-Brown1, Prakrit Kumar1, Oluwasemilore Adebayo2, Henry Searle1, Andrew Metcalfe1, Edward Davis3, Chetan Khatri1
1University of Warwick, Coventry, United Kingdom. 2Lister Hospital, Stevenage, United Kingdom. 3Royal Orthopaedic Hospital, Birmingham, United Kingdom
Background: To improve functional outcomes following total knee arthroplasty (TKA), robotic systems have been introduced such as the MAKO (Stryker). This systematic review aimed to compare the patient reported outcome measures (PROMs) of robotic TKA (RTKA) to manual TKA (MTKA).
Methods: Five electronic databases were systematically searched for eligible articles that used PROMs to compare MAKO RTKA to MTKA. The primary outcome was the Forgotten Joint Score (FJS). We defined follow up periods as short- (up to three months), medium- (three months to one year) and long-term (beyond one year). We pooled outcomes combining the Knee Society Scoring System (KSS), Oxford Knee Score (OKS), and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Meta-analyses were conducted using a random-effects model and reported using mean difference (MD) or standardised mean difference (SMD) and 95% confidence intervals (CI).
Results: Twenty-two articles evaluating 3738 TKAs were included, 1835 MTKAs and 1903 RTKAs. The evidence level for most studies were IIa, reflecting a lack of high-level studies. Using FJS, meta-analysis showed little difference at short-term (MD 11.49, 95% CI -5.62 to 28.59), but found a difference at medium-term (MD 5.50, 95% CI 2.19 to 8.81), but this was not sustained at long-term follow-up (MD 23.89, 95% CI -16.50 to 64.27). Pooling all PROMs showed no difference in short-term (SMD 0.27, 95% CI -0.05 to 0.59), but results favoured RTKA at medium- (SMD 0.46, 95% CI 0.22 to 0.70) and long-term (SMD 0.40, 95% CI 0.13 to 0.66).
Discussion: There are few high-level studies, but based on current data MAKO RTKA results in improved functional outcomes compared to MTKA in medium- and long-term term. Further randomised controlled trials are required to provide robust data and to assess clinical and cost effectiveness as well as a wider spectrum of early and late outcomes.
297 - Prehabilitation ahead of joint preservation surgery alters knee kinematics, pain levels and proprioception
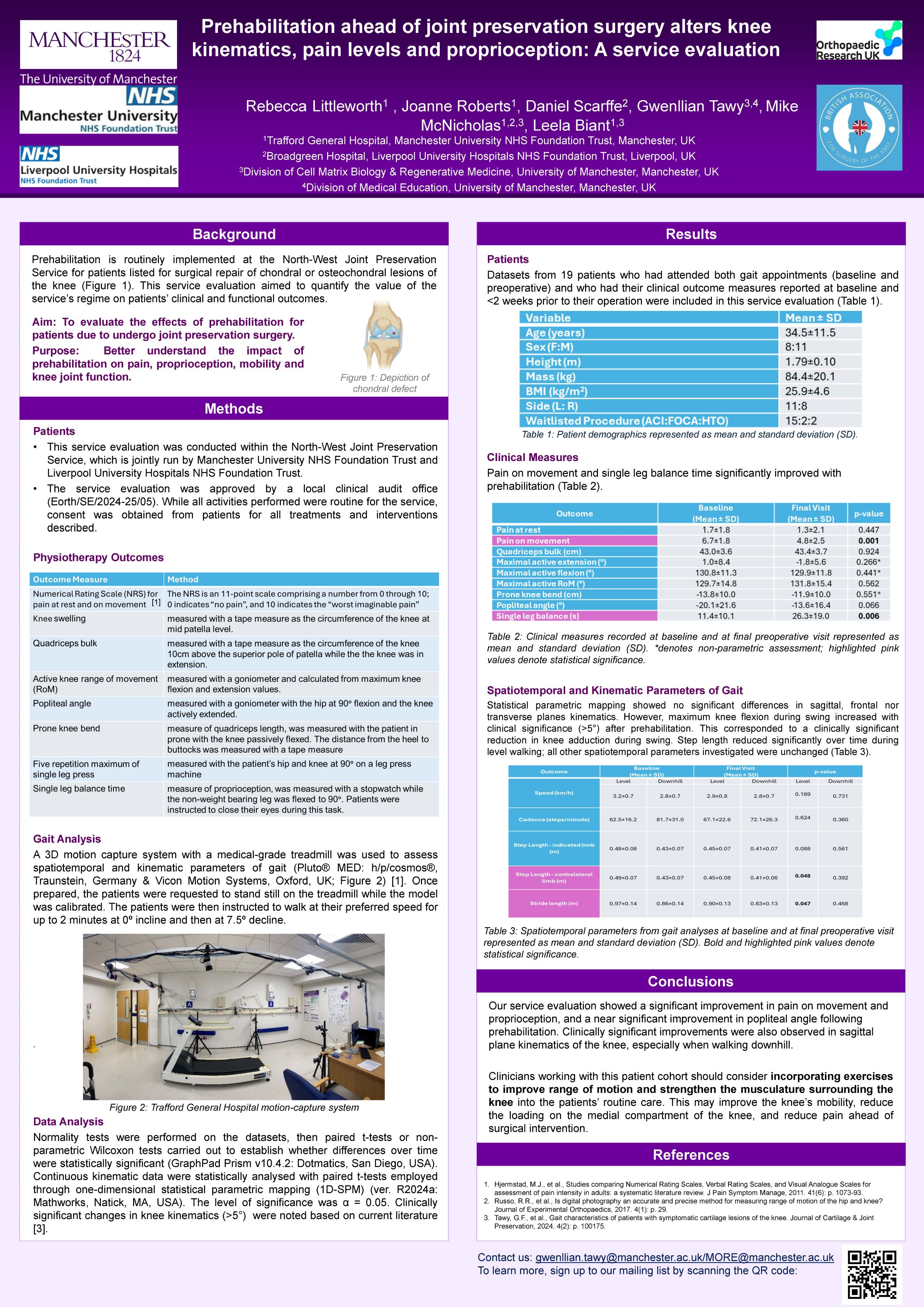
Rebecca Littleworth1, Joanne Roberts1, Daniel Scarffe2, Mike McNicholas2,1, Leela Biant3,1, Gwenllian Tawy3
1Manchester University NHS Foundation Trust, Manchester, United Kingdom. 2Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom. 3University of Manchester, Manchester, United Kingdom
Background: Patients awaiting surgery for chondral lesions of the knee at the North-West Joint Preservation Centre undergo a routine prehabilitation regime. This service evaluation aimed to quantify the impact of the centre’s regime on patients’ gait characteristics and common clinical markers.
Methods: Patients listed for cartilage repair surgery of the knee underwent prehabilitation with specialised musculoskeletal physiotherapists. Routine biomechanical and clinical assessments were performed before prehabilitation and immediately prior to surgery (after prehabilitation).
Knee kinematics and spatiotemporal parameters of gait were objectively assessed on a treadmill with 3D motion capture.
Additional objective markers included quadriceps bulk, knee range of movement, prone knee bend, popliteal angle, and single leg balance. Pain at rest and pain on movement were also assessed by the Numerical Rating Scale.
Statistical analyses in GraphPad Prism and MATLAB compared changes over time (α = 0.05).
Results: 16 patients walked at an average speed of 3.2±0.8km/h at baseline and 3.0±0.8km/h after prehabilitation (p=0.144), with stride lengths of 0.972±0.144m and 0.896±0.067m (p=0.064), and cadences of 62.5±16.2 steps/minute and 67.1±22.6 steps/minute, respectively (p=0.512).
Statistical parametric mapping showed no significant differences in sagittal, frontal nor transverse planes kinematics. However, maximum knee flexion during swing increased with clinical significance (>5°) after prehabilitation. This corresponded to a clinically significant reduction in knee adduction.
Pain on movement (p=0.047), single leg balance (p=0.013) and popliteal angle (p=0.013) significantly improved after prehabilitation. Range of movement (p=0.749), prone knee bend (p=0.581), quadriceps bulk (p=0.854) and pain at rest (p=0.449) did not change.
Conclusion: Improvements to patient reported pain levels, hamstring length and single leg balance demonstrate immediate benefits to prehabilitation ahead of joint preservation surgery. Changes observed in the sagittal and frontal planes during gait may have longer-term benefits through reduced loading across the medial compartment of the knee.
322 - No Difference in Career Longevity of Professional Football and Rugby Players After ACL Reconstruction with Associated MCL Injuries Compared to Uninjured Matched Controls
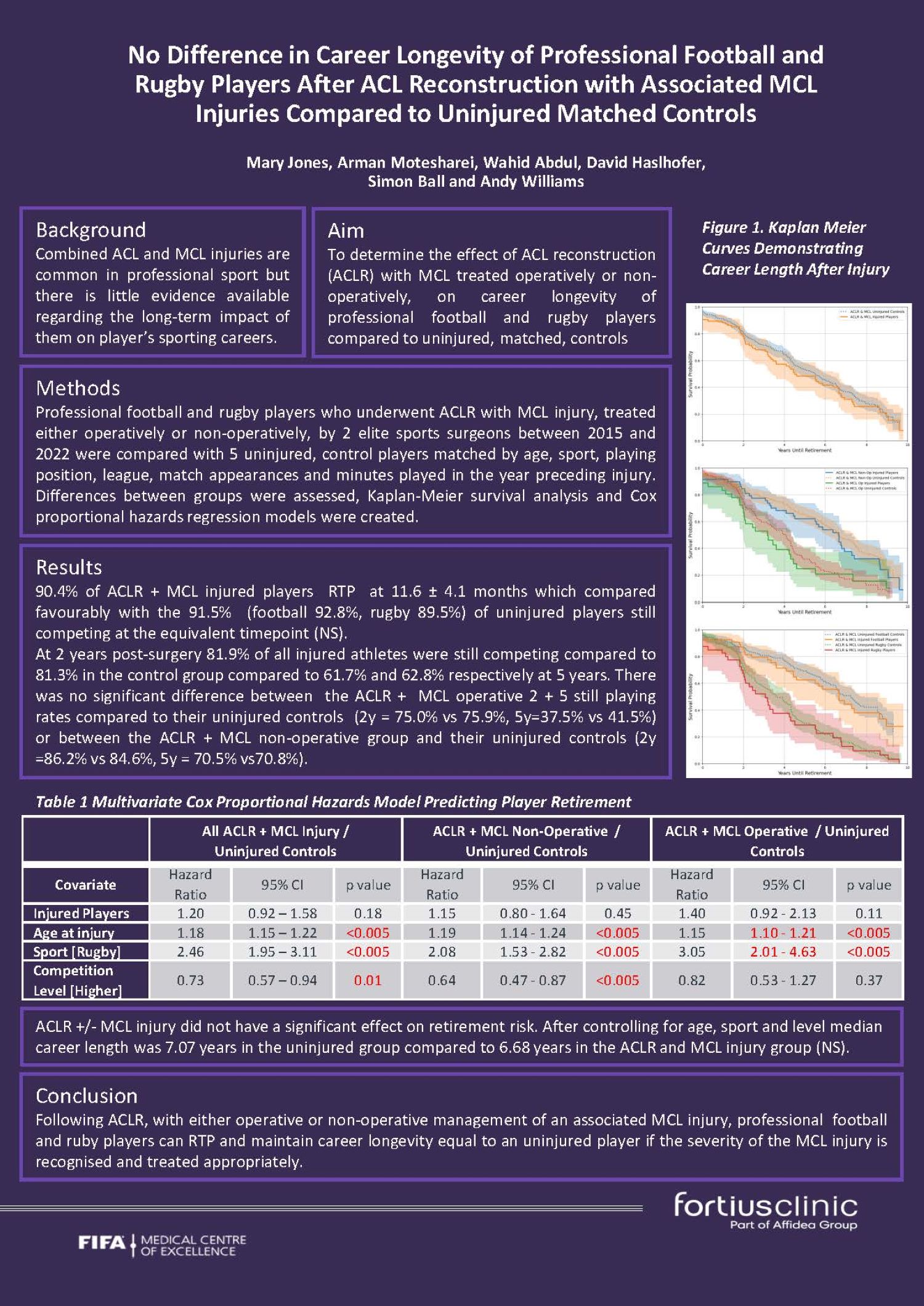
Mary Jones, Arman Motesharei, Wahid Abdul, David Haslhofer, Simon Ball, Andy Williams
Fortius Clinic, London, United Kingdom
Background: The impact of combined ACL and MCL injuries, which are common in professional sport, on a professional football or rugby player’s career is unknown. This study aimed to determine the effect
of ACL reconstruction (ACLR) with MCL treated operatively or non-operatively, on career longevity of professional football and rugby players compared to uninjured, matched, controls.
Methods: Professional football and rugby players who underwent ACLR with MCL injury, treated either operatively or non-operatively, by 2 elite sports surgeons between 2015 and 2022 were compared with 5 uninjured, control players matched by age, sport, playing position, league, match appearances and minutes played in the year preceding injury. Differences between groups were assessed, Kaplan-Meier survival analysis and Cox proportional hazards regression models were created.
Results: 90.4% (football 92.6%, rugby, 87.5%) of ACLR & MCL injured players RTP at 11.6 ± 4.1 months compared to 91.5% (football 92.8%, rugby 89.5%) of uninjured control players at 11 months post equivalent operation date (NS). Mean career length after RTP was 5.46 years versus 5.56 years (NS) in controls.
At 2 years post-surgery 81.9% (ACLR & MCL non-operative 86.2% vs ACLR & MCL operative 75%) compared to 81.3% in the control group (84.6% and 75.9% respectively, NS) were still competing. This reduced to 61.7% (70.5 and 37.5% respectively) by 5 years in the injured group and 62.8% (70.8% and 41.5%, NS).
After controlling for age, sport and level played, median career length was 7.07 years in the uninjured group compared to 6.68 years in the ACLR and MCL injury group (NS)
Conclusion: Following ACLR with either operative or non-operative management of an associated MCL injury professional football and rugby players can RTP and maintain career longevity equal to an uninjured player if the severity of the MCL injury is recognised and treated appropriately.
327 - Comparative Outcomes of Isolated Lateral Meniscus Repair and Meniscectomy in Elite Footballers: Implications for Return to Play, Career Longevity and Performance
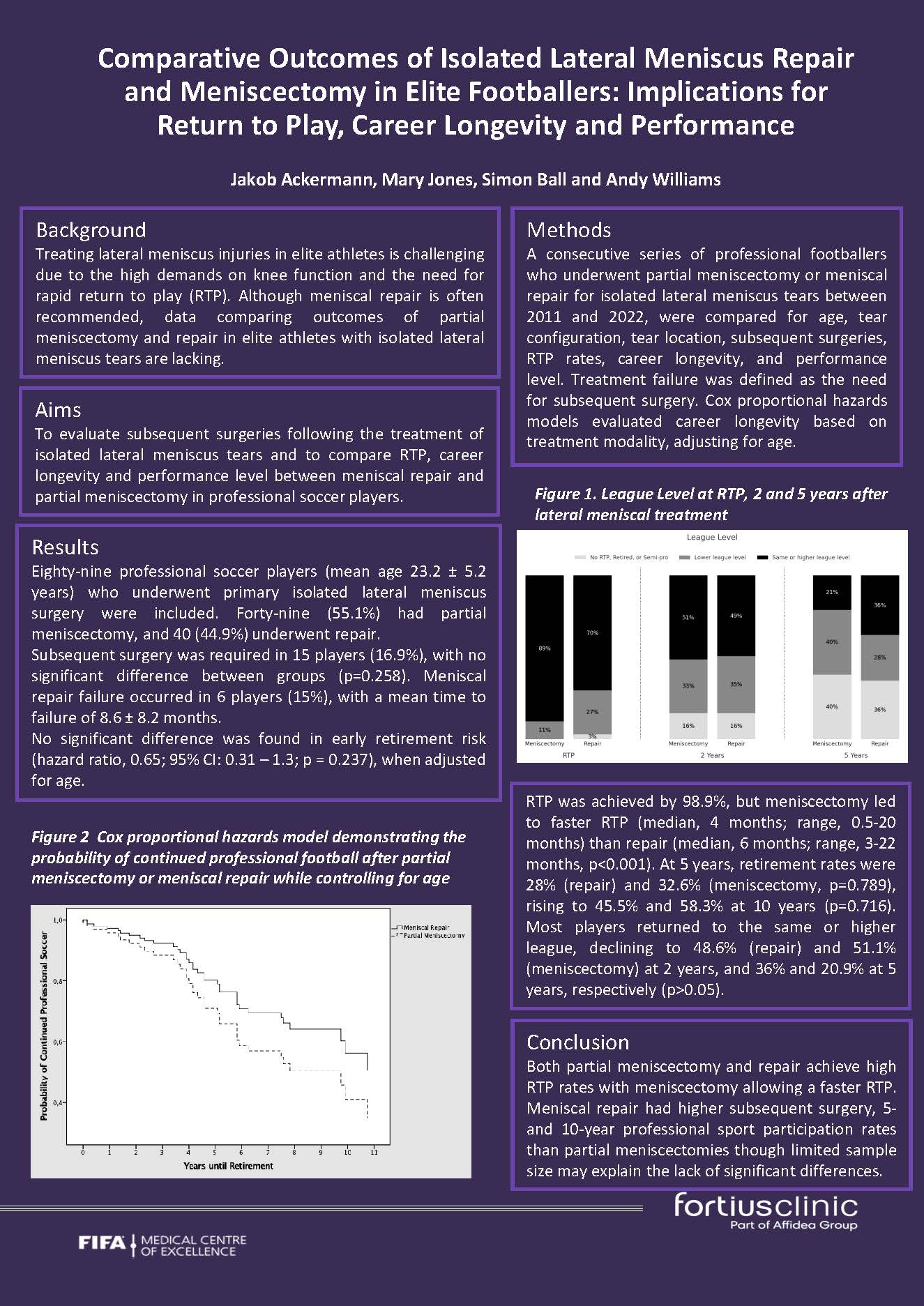
Jakob Ackerman, Mary Jones, Simon Ball, Andy Williams
Fortius Clinic, London, United Kingdom
Background: Repair of lateral meniscal tears is recommended in elite athletes but the evidence for this is limited. Therefore, return to play (RTP), career longevity and subsequent surgery in professional footballers after meniscal repair and partial meniscectomy for isolated lateral meniscal tears were compared.
Methods: A consecutive series of professional footballers who underwent partial meniscectomy or meniscal repair for isolated lateral meniscus tears between 2011 and 2022, were compared for age, tear configuration, tear location, subsequent surgeries, RTP rates, career longevity, and performance level. Treatment failure was defined as the need for subsequent surgery. Cox proportional hazards models evaluated career longevity based on treatment modality, adjusting for age.
Results: 89 professional footballers (mean 23.2 ± 5.2y were included.49 (55.1%) had partial meniscectomy, and 40 (44.9%) underwent repair. Subsequent surgery was required in 15 players (16.9%), with no significant difference between groups (12.2% (meniscectomy) vs. 22.5% (repair), p=0.258). Meniscal repair failure occurred in 6 players (15%), at mean 8.6 ± 8.2 months. 98.9%, RTP was faster after meniscectomy (median, 4 months; range, 0.5-20 months) than repair (median, 6 months; range, 3-22 months, p<0.001). No significant difference was found in early retirement risk (hazard ratio, 0.65; 95% CI: 0.31 – 1.3; p = 0.237), when adjusted for age. At 5 years, retirement rates were 28% (repair) and 32.6% (meniscectomy, p=0.789), rising to 45.5% and 58.3% at 10 years (p=0.716). 70% (repair) and 89% (meniscectomy)) returned to the same or higher league, declining to 48.6% (repair) and 51.1% (meniscectomy) at 2 years, and 36% and 20.9% at 5 years, respectively (p>0.05).
Conclusion: Both partial meniscectomy and repair achieve high RTP rates with meniscectomy allowing a faster RTP. Meniscal repair had more subsequent surgery, and higher 5- and 10-year professional sport participation rates than partial meniscectomies though limited sample size may explain the lack of significant differences.
328 - Isolated Lateral Collateral Ligament Injuries in Elite Athletes Can Be Successfully Treated Non-Operatively
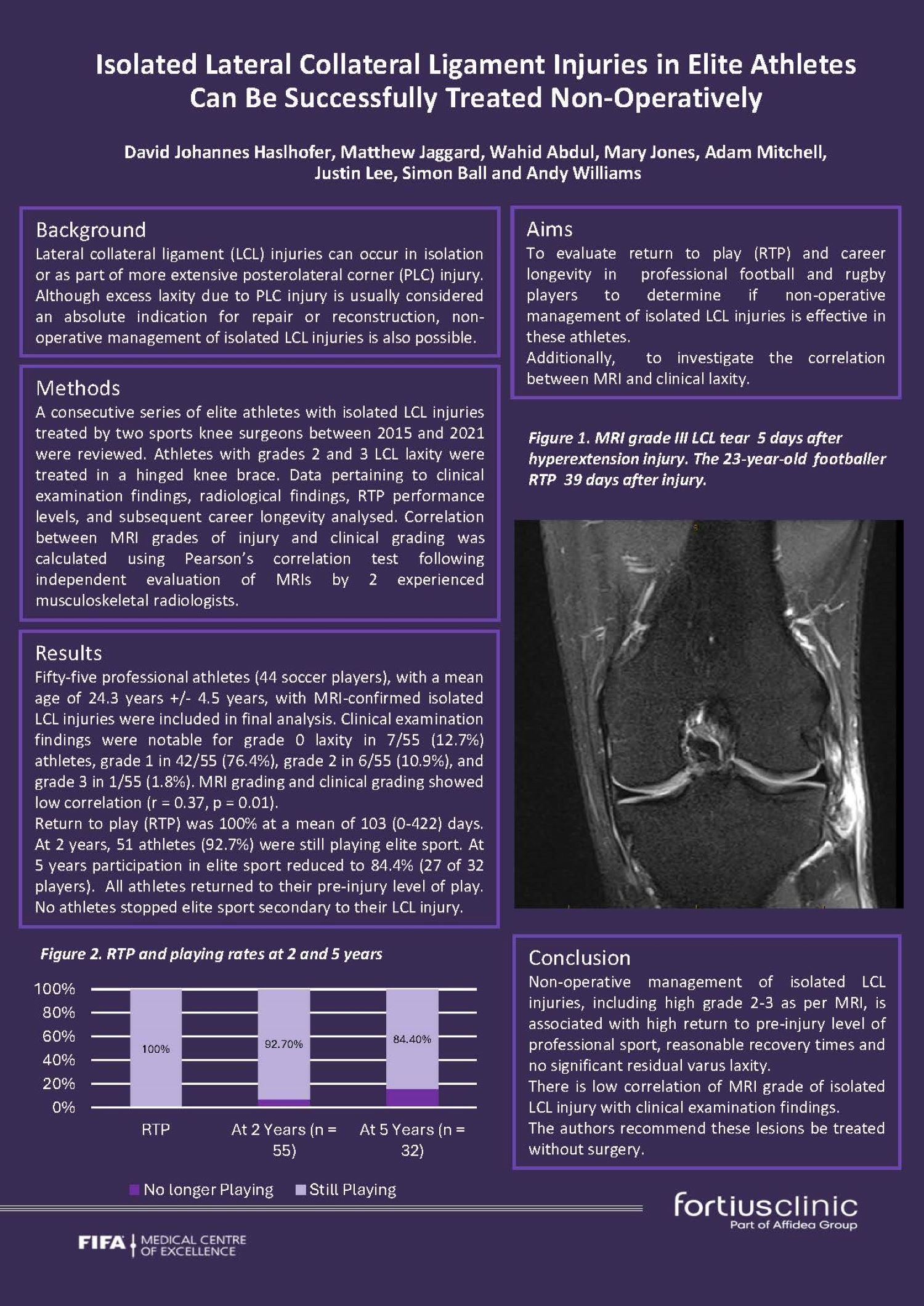
David Haslhofer, Matthew Jaggard, Wahid Abdul, Mary Jones, Adam Mitchell, Justin Lee, Simon Ball, Andy Williams
Fortius Clinic, London, United Kingdom
Abstract
Background
Lateral collateral ligament (LCL) injuries can occur in isolation or as part of a more extensive posterolateral corner (PLC) injury. Evaluation of return to play (RTP) and career longevity in elite athletes was undertaken to determine if non-operative management of isolated LCL injuries is effective. Additionally correlation between MRI and clinical laxity was investigated.
Methods
A consecutive series of elite athletes with isolated LCL injuries treated by two sports knee surgeons between 2015 and 2021 were reviewed. Athletes with grades 2 and 3 LCL laxity were treated in a hinged knee brace. Data pertaining to clinical examination findings, radiological findings, RTP performance levels, and subsequent career longevity analysed.Correlation between MRI grades of injury and clinical grading was calculated using Pearson’s correlation test following independent evaluation of MRIs by 2 experienced musculoskeletal radiologists.
Results
Fifty-five professional athletes (44 soccer players), with a mean age of 24.3 years +/- 4.5 years were included. Clinical examination findings found grade 0 laxity in 7/55 (12.7%) athletes, grade 1 in 42/55 (76.4%), grade 2 in 6/55 (10.9%), and grade 3 in 1/55 (1.8%). MRI grading and clinical grading showed low correlation (r = 0.37, p = 0.01). 100% RTP at a mean of 96.8 (±75.6) days. At 2 years, 51 athletes (92.7%) were still playing elite sport reducing to 84.4% (27 of 32 players) at 5 years. All athletes returned to their pre-injury level of play. No athletes stopped elite sport due to their LCL injury.
Conclusion
Non-operative management of isolated LCL injuries, including high grade 2-3 as per MRI, is associated with high return to pre-injury level of sport, reasonable recovery times and no significant residual varus laxity. There is low correlation of MRI grade of isolated LCL injury with clinical examination findings. The authors recommend these lesions be treated without surgery.
357 - Understanding the Factors that Influence Decision-Making regarding Management of ACL Injuries: a UK, Australian and Canadian-based Delphi Study
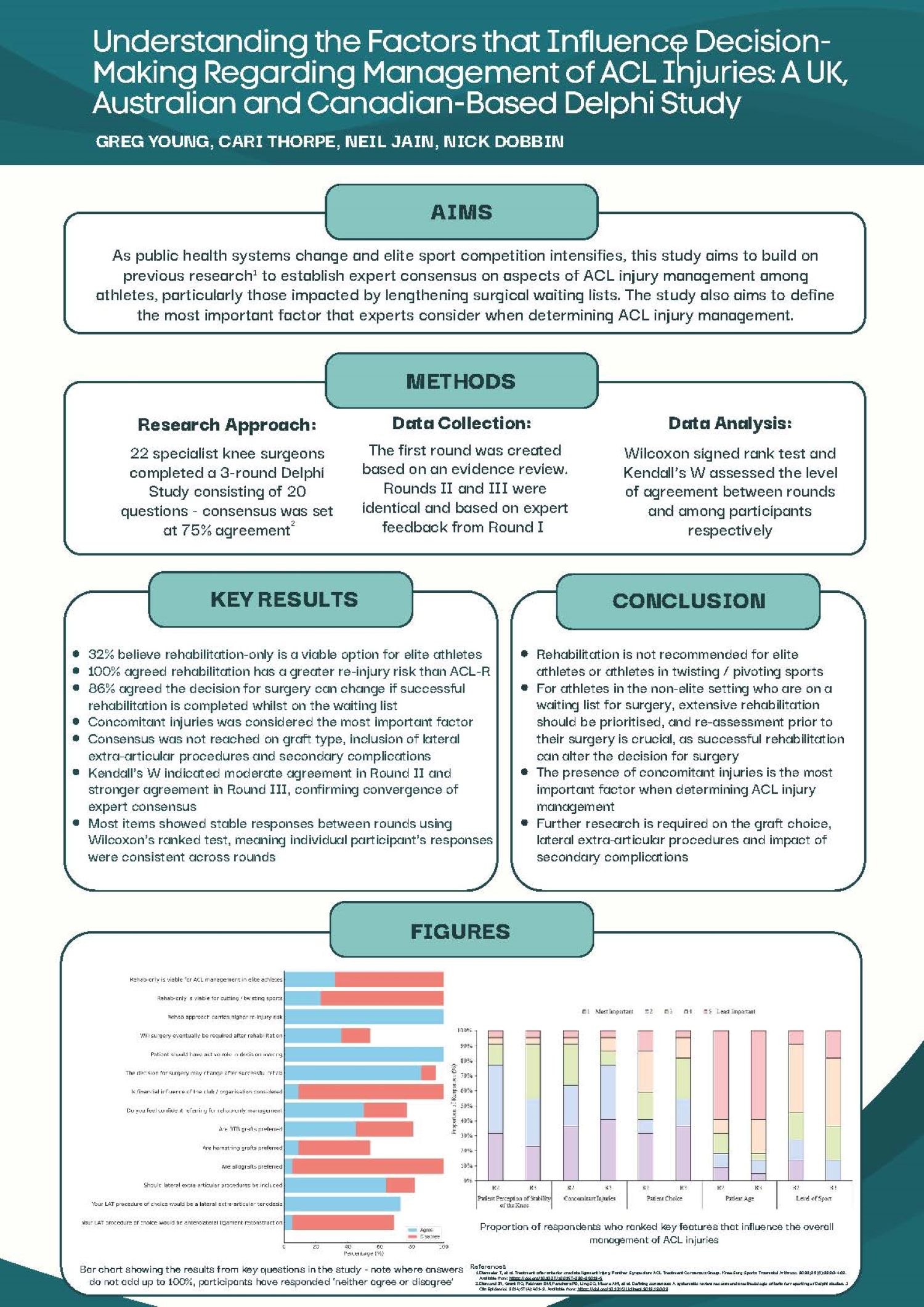
Greg Young1, Neil Jain2, Cari Thorpe1
1Manchester Metropolitan University, Manchester, United Kingdom. 2Manchester Institute of Health and Performance, Manchester, United Kingdom
Background: Management of anterior cruciate ligament (ACL) injuries remains highly debated, with conflicting findings within the literature. As the landscape within public health systems alters and competition within elite sport increases, this study aims to establish expert consensus on recommendations of ACL injury management on those impacted by lengthy waiting lists for surgery in public healthcare and amongst elite athletes.
Methods: Twenty-four experts from around the world completed a three-round survey based on the Delphi method of achieving consensus. Participants were asked to agree or disagree using a Likert-scale for statements developed and based on a review of recent literature in Round I. Feedback was obtained to improve the existing statements and incorporate any additional information. Round II and III used Likert-scale voting to assess consensus, which was defined as ≥75% agreement.
Results: Consensus was achieved in 11/20 statements, including strong consensus recommending ACL-Reconstruction (ACL-R) in patients participating in cutting, twisting, or pivoting sports. Agreement suggested patients may avoid surgery if undertaking successful rehabilitation whilst waiting for surgery. Most experts agreed rehabilitation alone isn’t recommended for elite athletes, and concomitant injuries are the most important finding when determining surgical or conservative management.
Conclusions/Findings: Rehabilitation alone is not recommended for elite athletes in treatment for ACL tears. Re-assessment prior to ACL-R is crucial for non-elite athletes. Key areas of non-consensus included the impact of surgery or rehabilitation on secondary complications, graft choice and the inclusion of lateral extra-articular procedures, suggesting further research is required in these areas.
Disclosure: The authors declare no conflicts of interest.
368 - Epidemiological Analysis of Mental Health Disorders in the Total Knee Replacement Population
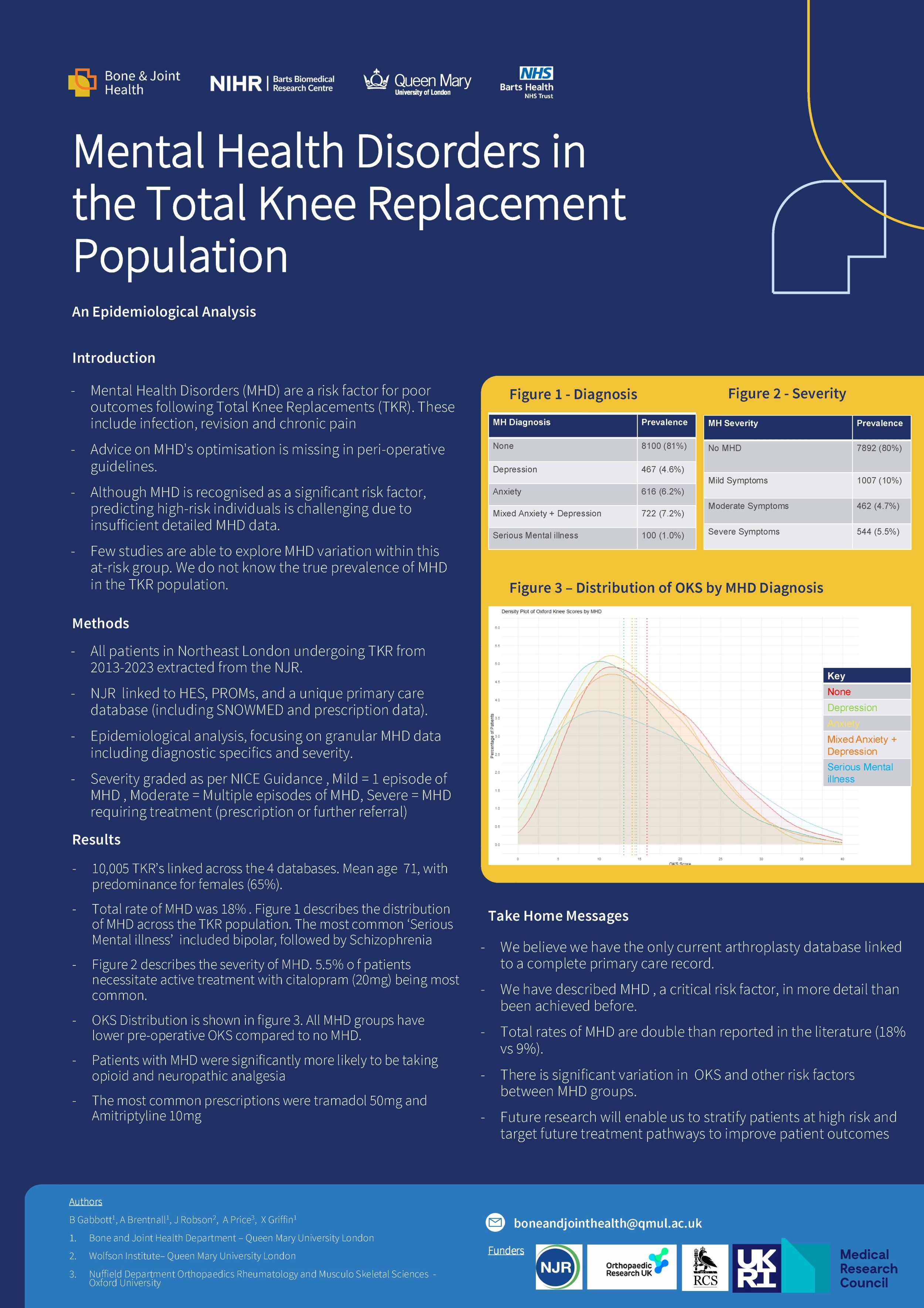
Ben Gabbott1, Adam Brentnall1, John Robson1, Andrew Price2, Xavier Griffin1
1Bone and Joint Health Department , Queen Mary University London, London, United Kingdom. 2NDORMS, Oxford University, Oxford, United Kingdom
Introduction: Chronic pain after total knee replacement(TKR) costs the NHS £33million annually. Patients with Mental Health Disorders(MHD) face higher risks of chronic pain post-TKR. Advice on MHD's optimisation is missing in peri-operative guidelines.
Although MHD is recognised as a significant risk factor, predicting high-risk individuals is challenging due to insufficient detailed MHD data. It is often treated incorrectly as a binary predictor.
Few studies are able to explore MHD variation within this at-risk group. We do not know the true prevalence of MHD in the TKR population.
Methods: All patients in Northeast London undergoing TKR from 2013-2023 extracted from the NJR and linked to HES, PROMs, and a unique primary care database (including SNOWMED and prescription data).
Subsequent descriptive epidemiological analysis, focusing on granular MHD data including diagnostic specifics, timing and severity.
Results: 10,005 TKRs were linked across 4data sources. Of these, 1,905(19.2%) patients had an MHD diagnosis. The most common was Mixed Anxiety and Depression(722-7.2%), followed by Anxiety(616-6.2%) and Depression(467-4.7%). 100(1.0%) were diagnosed with 'Serious Mental Illness,' including bipolar disorder, psychosis, and schizophrenia.
544(5.5%) had a MHD severe enough to necessitate active treatment, with 'citalopram 20mg' as the most frequent prescription. 247(2.5%) experienced an acute MHD exacerbation, needing a GP appointment within a year before TKR.
MHD patients had larger prescribed analgesia needs (opioids/neuropathic) and lower PROMs scores (OKS/ EQ5D).
Discussion: We believe we have the only arthroplasty database linked to a complete primary care record in the world. We described MHD, a significant risk factor, in more detail than before, capturing critical data on it's distribution and severity. Rates of MHD are higher than reported in the literature. This research will enable us to stratify patients at high risk and target future treatment pathways to improve patient outcomes.
445 - Aseptic Tibial Loosening in NexGen Legacy Posterior Stabilised Tibial Implants: A Single-Centre Comparative 10 year Outcomes Study
Saskia Locke1, James Doonan1,2, Emma Bailey1,2, Emily Seymour-Jackson2, Nathan Campbell1, Mark Blyth1, Bryn Jones1
1Glasgow Royal Infirmary, Glasgow, United Kingdom. 2University of Glasgow, Glasgow, United Kingdom
Introduction: Aseptic tibial loosening is a leading cause of revision surgery after total knee arthroplasty (TKA). Concerns exist about the performance of non-augmentable NexGen Legacy Posterior Stabilised (LPS) tibial implants due to increased rates of aseptic loosening requiring revision. This study compares the survivorship of augmentable and non-augmentable implants over a minimum 10-year follow-up and identifies a high-risk cohort for aseptic tibial loosening following primary TKA with the non-augmentable tibial implant.
Methods: A retrospective review of 1830 primary NexGen LPS TKAs performed between 2009 and 2014 was conducted, including 811 augmentable and 1019 non-augmentable tibial implants. Revision rates, reasons for revision, and patient demographics were analysed. Kaplan-Meier analysis assessed implant survivorship and subgroup analyses examined the influence of age and BMI on aseptic loosening.
Results: Non-augmentable tibial implants had higher all-cause revision rates (6.4% vs. 4.1%; p=0.036) and aseptic loosening rates (2.5% vs. 0.7%; p=0.005) compared to augmentable tibial implants. Kaplan-Meier analysis showed significantly lower 10-year survivorship for non-augmentable implants (p=0.0084) and for aseptic loosening specifically (p=0.0012). Younger patients (<65 years) with BMI >40 kg/m² receiving non-augmentable implants had the highest aseptic loosening rate (9.1%); no aseptic loosening was observed in older patients (>65 years) with the same BMI and implant type.
Conclusion: Non-augmentable NexGen LPS tibial implants are associated with significantly higher rates of aseptic loosening, particularly in younger, high-BMI patients. These findings inform implant selection and long-term follow-up strategies in knee arthroplasty. Future studies should further investigate implant factors contributing to aseptic loosening and optimise strategies for early detection of underperforming implant subtypes within national datasets.
670 - Incidence, Predictors, and Cost of Sepsis Following Septic TKA Revisions
Islam Sherif1, Maile Wedgwood2, Khaled Elmenawi3, Nicolas Piuzzi3
1South Warwickshire NHS Foundation Trust, Warwick, United Kingdom. 2Warwick Medical School, Coventry, United Kingdom. 3Cleveland Clinic, Cleveland, USA
Introduction: Limited data exist on the incidence of sepsis following septic revision total knee arthroplasty (TKA). We aimed to estimate the incidence, predictors, and cost of sepsis within 90 days of revision of TKA for periprosthetic joint infection (PJI).
Methods: A retrospective analysis of first-time both-component revision TKA for PJI (n=16,535) using a national all-payer database between 2016-2022 was performed. Patients were divided into those who developed sepsis within 90 days of revision TKA for PJI (n=2365) and those who did not (n=14,170). The overall and annual incidence of sepsis were estimated. Multivariate regression was performed to predict risk of 90-day sepsis following surgery. The average 90-day reimbursement per patient was compared between patients with and without sepsis after propensity score matching.
Results: Overall, 14% of patients developed sepsis within 90 days of surgery. Male gender (OR 1.2, p<0.001), renal failure (OR 1.2, p<0.001), tobacco use (OR 1.1, p<0.01), morbid obesity (OR 1.1, p=0.01), Elixhauser Comorbidity Index (ECI) (OR 1.08, p<0.001), and hypoalbuminemia (OR 1.1, p=0.03) were associated with a higher risk of sepsis within 90 days of revision TKA for PJI. Average reimbursement per patient in the 90 days following surgery was significantly higher among patients who developed sepsis compared to those who did not ($15,979 vs $11,306, p<0.001).
Conclusion: Approximately 14% of revision TKA PJI patients developed sepsis within 90 days. Male gender, renal failure, tobacco use, morbid obesity, higher ECI, and hypoalbuminemia independently increased the risk of sepsis. Optimizing modifiable risk factors such as smoking may help reduce the incidence and associated cost of sepsis following revision TKA for PJI.
Limb Reconstruction
635 - Timely Orthoplastic Care in Open Lower Limb Trauma: A Retrospective Cohort Study of Flap Outcomes and Predictive Variables
Louis John Stephen1,2, Pei-Ru Chew2, Mark Doran2, Neil Fairbairn2, Sherilyn Tay2, John Biddlestone1,2
1School of Medicine, Veterinary & Life Sciences, University of Glasgow, Glasgow, United Kingdom. 2Department of Plastic & Reconstructive Surgery, Canniesburn Plastic Surgery Unit, Glasgow Royal Infirmary, Glasgow, United Kingdom
Background: Despite growing evidence that orthoplastic care improves outcomes and reduces complications, global provision remains inconsistent. Orthoplastic care reduces infections (RR 0.37, p<0.0001), reliance on secondary intention healing (RR 0.02, p<0.0001), and hospital stays by 30% when soft tissue coverage occurs within 72 hours. In the UK, Major Trauma Centres (MTCs) halve flap failure rates compared to non-orthoplastic centres (p<0.05). This retrospective cohort study evaluates flap data and outcomes from our local database for open lower limb fractures, with particular focus on timing of orthopaedic and plastic surgical intervention.
Methods: Data was collected at Queen Elizabeth University Hospital, Glasgow, from October 2020 to November 2023. Of 256 patients treated for lower limb trauma, 95 (98 flaps) met inclusion criteria. Demographic data, injury specifics, Gustilo-Anderson classification, orthopaedic fixation methods, and patient outcomes were analyzed using Fisher’s Exact Test, Chi-square tests, and logistic regression. Cases were reviewed to identify delays in referral, fixation, and flap coverage.
Results: Initial fixation was 82.5% external and 17.5% internal, with definitive fixation at 56.3% external and 43.7% internal. External fixation was primarily achieved with the use of Ilizarov frames. ALT flaps were used in 50% of cases, with flap distribution as 68.4% free, 21.4% pedicled, and 10.2% local. The amputation rate was 10.2%, with a return-to-theatre rate of 35.7%. Delays in orthoplastic referral and soft tissue coverage significantly correlated with complications (p=0.0048, p=0.0210). Logistic regression identified time to coverage as an independent predictor of complications (OR: 2.4, CI: 1.5–3.9).
Conclusions / Implications: This study reinforces the importance of coordinated orthoplastic care. Timely bony fixation and in particular, soft tissue reconstruction, reduces complications, supporting continued efforts to streamline multidisciplinary pathways. Our findings further reinforce the BOA/BAPRAS guidelines, highlighting early referral and a collaborative orthoplastic approach as essential to optimising outcomes in lower limb trauma.
Disclosures: None.
766 - Elective amputations in adult limb reconstruction - a 15-year analysis of indications and outcomes
Lidia Nunez Jaramillo1, Charles Merry2, Luke Marsh2, Badri Narayan2, William Harrison2
1Liverpool University School of Medicine, Liverpool, United Kingdom. 2Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom
Background: Elective limb amputation is a recognised treatment option for a potentially salvageable limb. This study aims to investigate the differences between patients offered primary elective amputations versus patient with delayed elective amputations and determine differences in outcomes.
Methods: Retrospective observational study in a tertiary centre for limb reconstruction. Inclusion criteria were all adult elective amputations on lower extremities. Exclusion criteria were amputations secondary to ischaemic leg disease, malignancy or congenital anomalies.
Patient demographics, comorbidities, indication for amputation and prior number of operations were recorded as well as revision surgeries following amputations.
Results: There were 150 amputations, of which 93 met inclusion criteria, mean age 59 years.
Early decision to amputate occurred in 35% (n=33) of patients with a mean time to amputation of 50 days. Of the 65% (n=60) with delayed amputation, mean time to amputation was 245 days with a mean of 2.58 surgeries performed by the tertiary centre prior to amputation.
The major indication in both groups for amputation was osteomyelitis – 42% of patients in primary decision to amputate and 49% in delayed amputation. Mean length of stay for delayed amputations was 40 days (vs 28 days). One third of all patients required revision surgery. Only one patient had amputation for CRPS. There was a 4% inpatient mortality.
Conclusions/Findings: Age did not influence the decision to amputate or attempt salvage. The indication for amputation did not have an impact on whether the patient was offered primary or delayed amputation. Comparison of the two cohorts is limited by sample size however the data suggests that there is no significant difference in the number of unscheduled operations required, nor the amount of time between first and final revision. The high rate of revision surgery is important for informed consent.
Disclosure: No conflict of interest to declare
Medical Students
85 - The beneficial impact of pre-operative hand therapy appointments for Plastic Surgery handtrauma patients
Dhanuja Senn, Milen Santhosh, Lucy Wimmer, Emma Baker, Nitin Vaingankar
Northampton General Hospital, Northampton, United Kingdom
Aims: BSSH standards of care in soft tissue hand trauma have a clear 3-5 day target for hand therapy post-operatively. However, due to lack of patient education or mismanaged expectations, this target is frequently breached. Our project aimed to improve outcomes for hand trauma patients within the department. We aimed to evaluate the sustainable value of implementing a pre-operative consultation with the hand therapy team.
Methods: This prospective study identified new patients suffering with soft tissue hand trauma during April 2024, assessing patient outcomes, total number of appointments, including those missed, breach of 3-5 day target and total dressings costs. A modification to the pathway of patients was made, with a view to reduce missed appointments and improve outcomes, enabling patients to be seen by a hand therapist pre-operatively. This intervention was deemed to improve patient education and stress the importance of post-operative rehabilitation. The unit was re-assessed in September 2024.
Results: For all patients there was a statistically significant reduction in complications, number of appointments, number of missed appointments and duration under consultant care. This was forecasted to save our trust £88,000 per year. The reduction in appointments, translated to an added environmental benefit, with an average saving of 171.6kgCO2e per patient. Verbal feedback from patients was positive, with a reduction in stress and anxiety pre-operatively.
Conclusions: This study has demonstrated sustainable value across environmental, social, financial and clinical perspectives. The impact of this small process change, which required minimal disruption to service, had a significantly positive impact on patient experience and outcomes, it created a more efficient use of NHS resources with a more cohesive working between Hand Therapy and Plastic Surgery, whilst also benefiting the environment.
175 - Post-treatment outcomes of rigid bracing compared to surgical correction in moderate to severe adolescent idiopathic scoliosis– a systematic review
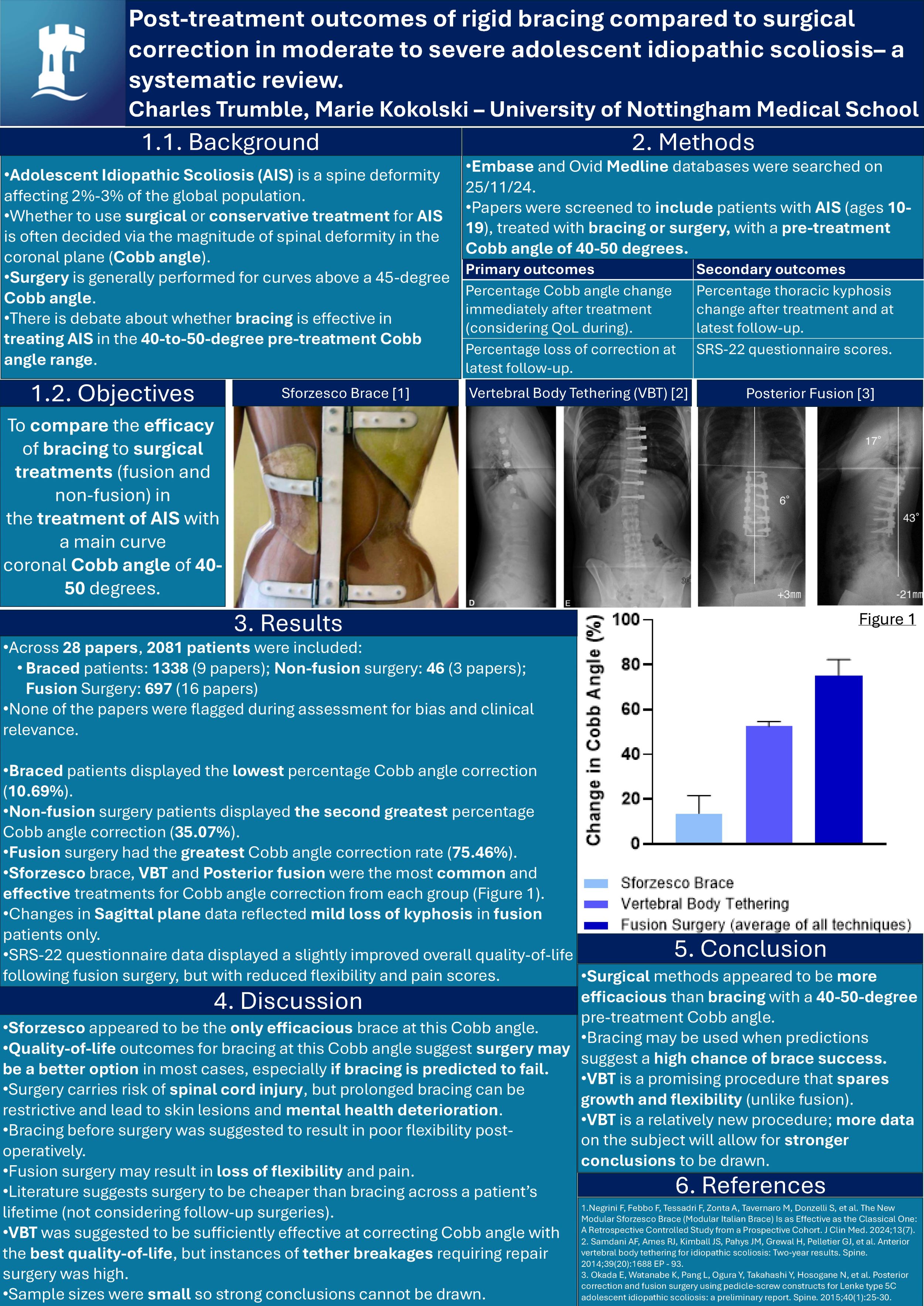
Charles Trumble, Marie Kokolski
University of Nottingham Medical School, Nottingham, United Kingdom
Background: Adolescent idiopathic scoliosis (AIS) is a spine deformity with a two to three percent prevalence globally. Treatment for AIS is often decided via the magnitude of spinal deformity in the coronal plane (Cobb angle). Surgery is generally performed at curves above 45 degrees, but there is debate whether bracing is effective in AIS treatment within the 40-to-50-degree Cobb angle range. This paper aims to compare the efficacy of bracing to surgical treatments (fusion and non-fusion) in AIS with a 40-to-50-degree main curve Cobb angle.
Methods: Embase and Ovid Medline were searched on 25/11/2024. Screening was performed for papers investigating bracing or surgical treatments for AIS strictly with a pre-treatment Cobb angle of 40-to-50-degree. Risk of bias appraisal was performed on papers following full text review.
Results: Across 28 studies, 2081 patients were sampled (85.87% female with a 14.37yr mean age when beginning treatment). Braced patients displayed the lowest percentage Cobb angle correction (10.69%) with the Sforzesco brace being most effective (13.66%). Vertebral body tethering (VBT) had the highest percentage Cobb angle correction in the non-fusion group (52.50%). Fusion surgery had the greatest Cobb angle correction rate (75.46%). Sagittal plane data was unremarkable with the acceptation of mild loss of kyphosis in fusion patients. SRS-22 questionnaire data displayed a mildly improved quality-of-life following fusion surgery. Most sampled patients were braced.
Conclusion: Surgery appeared to be more efficacious than bracing at this Cobb angle range especially where surgery is required following bracing failure. Quality-of-life outcomes for bracing appeared to be lower than surgery. Fusion surgery potentially causes loss of range of motion. VBT spares growth and motion while notably correcting Cobb angle. Few papers on non-fusion surgery were available due to this being a relatively new procedure. As more papers are published, a stronger conclusion on VBT efficacy may be drawn.
239 - Do Learning Curves Associated with Robotic Total Knee Arthroplasty Differ by Robotic Platform
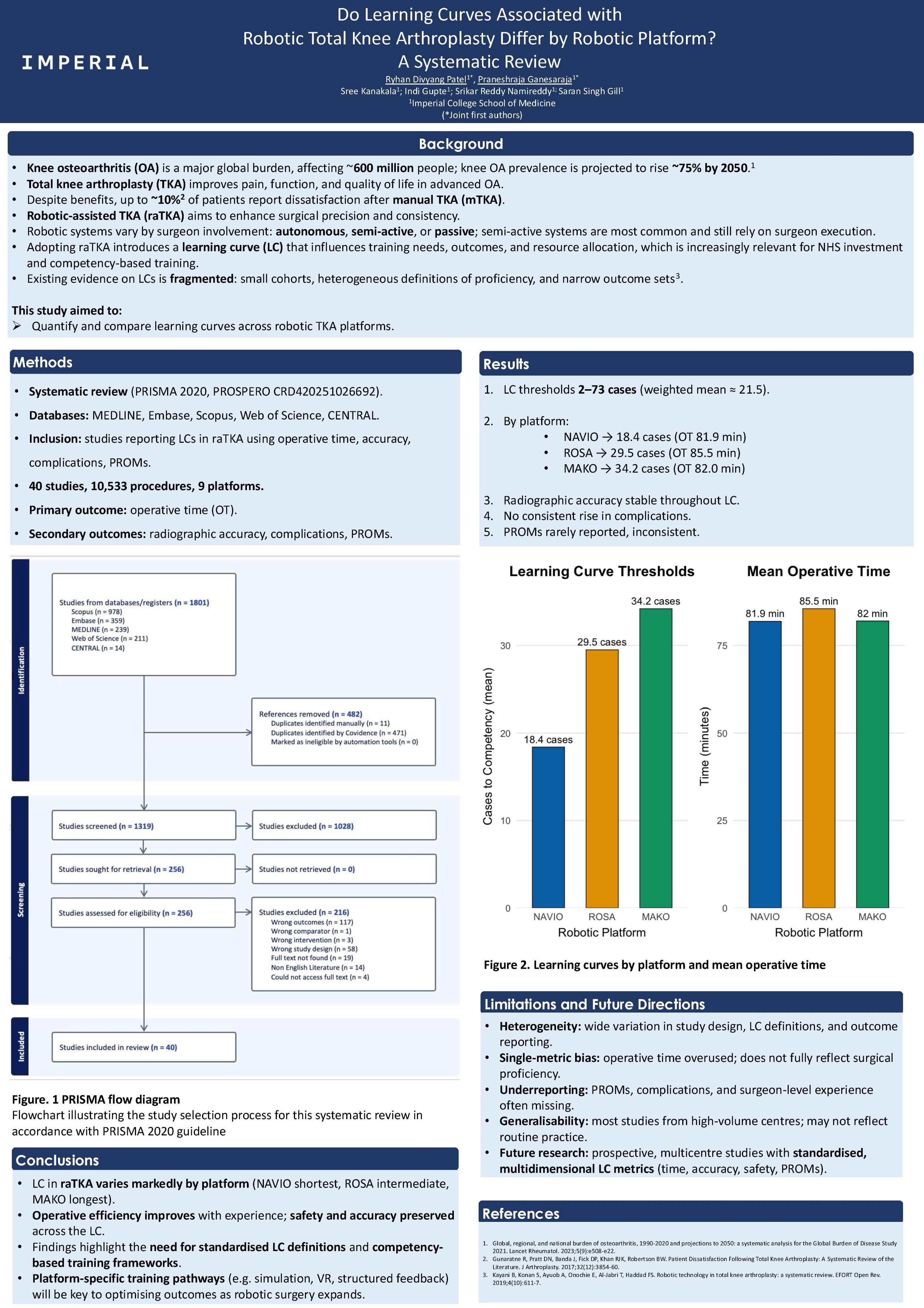
Ryhan Patel, Praneshraja Ganesaraja, Sree Kanakala, Indi Gupte, Srikar Namireddy, Saran Gill
Imperial College School of Medicine, London, United Kingdom
Background: Robotic-assisted total knee arthroplasty (raTKA) has seen widespread adoption due to its potential to enhance surgical precision and implant alignment. However, the learning curves (LC) associated with different robotic platforms remain poorly characterised, complicating training strategies and safe implementation. This systematic review aimed to quantify the LC across major raTKA systems, focusing on operative time and the number of cases required to achieve procedural proficiency.
Methods: A systematic search was conducted on December 16, 2024, across MEDLINE, Embase, Scopus, Web of Science, and CENTRAL, following PRISMA 2020 guidelines (PROSPERO registration pending) and SWiM guidelines. Studies reporting original data on LCs in raTKA or UKA were included. Outcomes were operative time, radiographic alignment, complication rates, and patient-reported outcome measures (PROMs). Due to methodological heterogeneity, meta-analysis was not performed; weighted means were calculated where appropriate.
Results: Thirty-nine studies were included, comprising 10,533 procedures across nine robotic platforms. Operative time, reported in 37 studies, served as the primary LC metric. The number of cases required to reach proficiency ranged from 2 to 73, with a weighted mean of 21.5 cases. Stratified analysis demonstrated that proficiency was achieved after a mean of 18.4 cases for NAVIO (mean operative time 81.9 minutes), 26.5 cases for ROSA (85.5 minutes), and 78.3 cases for MAKO (82.0 minutes). Radiographic accuracy and complication rates remained stable throughout the LC period. PROMs were underreported and showed inconsistent trends, limiting definitive conclusions.
Conclusion: The LC for raTKA is markedly platform dependent. Inconsistent reporting of radiographic and safety outcomes, particularly with the ROSA system, limited the analysis of secondary endpoints. These findings underscore the need for standardised LC definitions and robust comparative studies. Future research should focus on informing the development of robotic training curricula, aiding surgical accreditation, and supporting the safe integration of robotic platforms into clinical practice.
346 - Hip Spica - What Do Parents Really Think
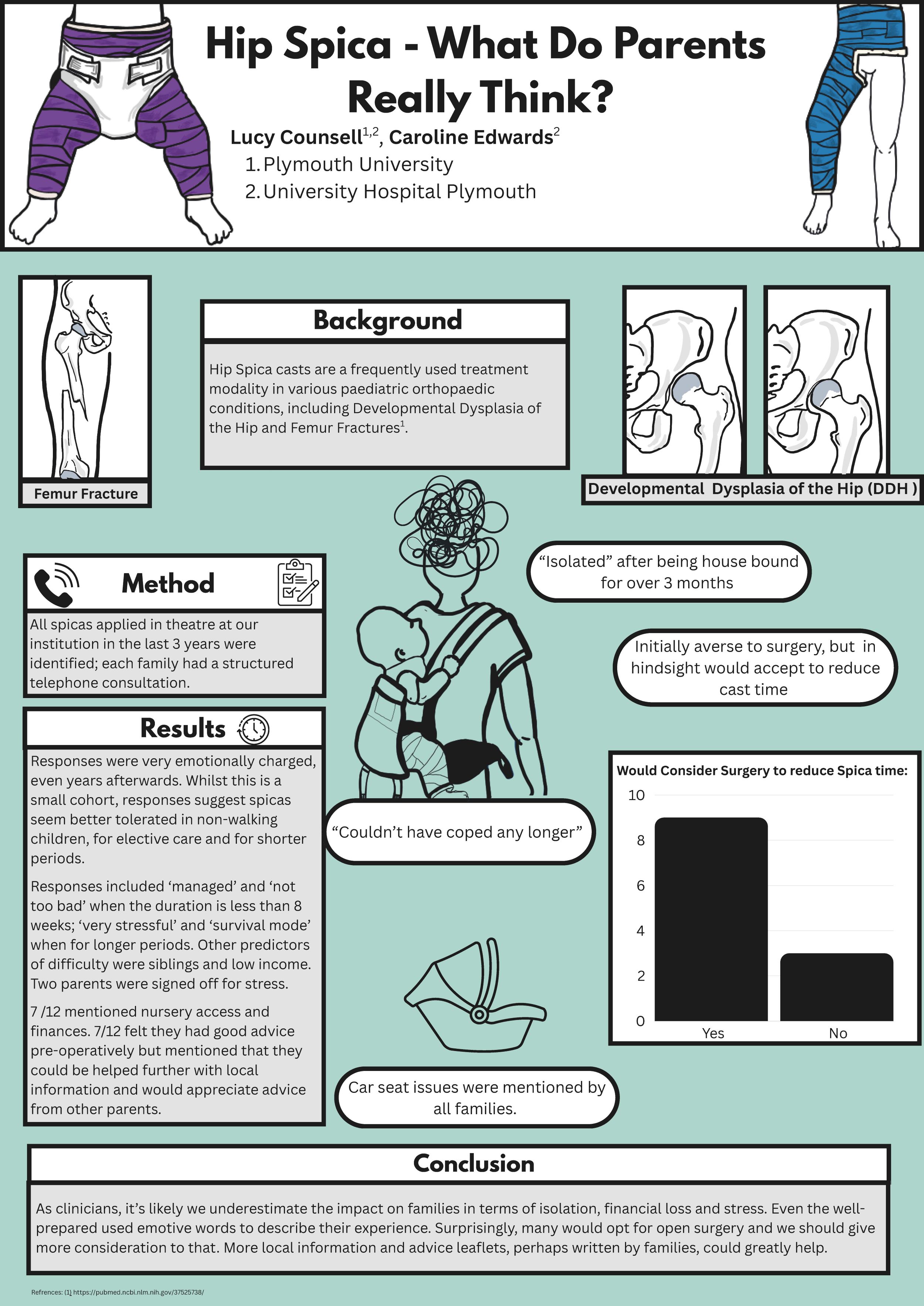
Lucy Counsell1, Caroline Edwards2
1Plymouth University, Plymouth, United Kingdom. 2University hospitals Plymouth, Plymouth, United Kingdom
Aim: Spica casts are frequently used in paediatric orthopaedics for elective and emergency care. We explored parents’ views and preoperative preparation. Is hip spica casting acceptable, or should we be seeking alternatives?
Method: All spicas applied in theatre at our institution in the last 3 years were identified; each family had a structured telephone consultation.
Results: Responses were very emotionally charged even years after. One parent expressed how isolated they felt being housebound for over 3 months. Another ‘couldn’t have coped any longer’. Another, initially averse to surgery, would, in hindsight, accept it to reduce cast time.
This is a small cohort, but responses suggest spicas seem better tolerated in non-walking children; elective care and shorter periods. Responses included ‘managed’, ‘not too bad’ when’ <8 weeks; ‘very stressful’, ‘survival mode’ for longer periods. Other predictors of difficulty were siblings and low income. 2 parents were signed off for stress.
9/12 would consider surgery to lessen spica time. Car seat issues were mentioned by all. 7 /12 mentioned nursery access and finances. 7/12 felt they had good advice pre-operatively but mentioned could be helped further with local information and appreciated advice from other parents.
Conclusion: As clinicians, it’s likely we underestimate the impact on families in terms of isolation, financial loss and stress. Even the well-prepared used emotive words to describe their experience. Surprisingly, many would opt for open surgery and we should give more consideration to that. More local information and advice leaflets, perhaps written by families, could greatly help.
361 - The Holy Grail in Early Diagnosis of DDH
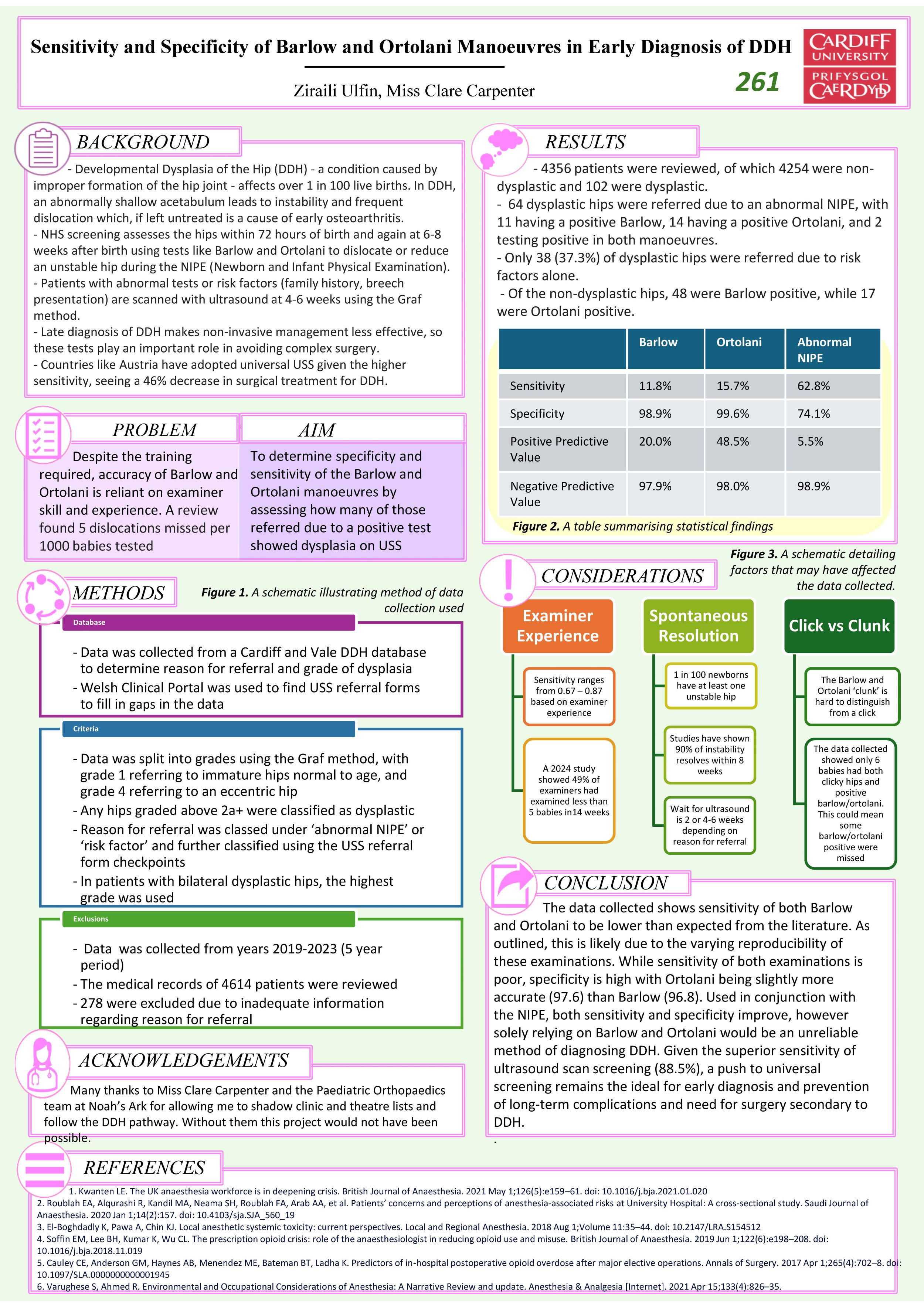
Ziraili Ulfin1, Clare Carpenter2
1Cardiff University, Cardiff, United Kingdom. 2Noah's Ark Hospital, Cardiff, United Kingdom
Background: UK screening for developmental hip dysplasia (DDH) involves the Neonatal Infant Physical Examination (NIPE) within 72 hours and at 6-8 weeks after birth. Sonography is requested for those with an abnormal NIPE or high-risk factors for DDH. Despite this robust programme, 5 in 1000 patients are missed.
Several countries have implemented universal ultrasound screening for DDH, noting reduced delayed diagnoses and necessity for surgical treatment.
Aim: The aim of this study was to determine sensitivity and specificity of Barlow and Ortolani which have been considered the “Holy Grail” in screening hip dysplasia.
Method: Medical records of 4614 patients over a 5-year period were reviewed. 278 children were excluded due to inadequate information.
Results: Of the 4614, 102 were sonographically-proven DDH. 63% of these were screened by ultrasound due to an abnormal NIPE finding. The sensitivity of Barlow was 11.8% with a specificity of 98.9% and a Positive Predictive Value (PPV) was 20% while Ortolani performed slightly better with a sensitivity of 15.7%, specificity of 99.6% and PPV of 48.5%. Despite the poor results, these manoeuvres outperformed isolated use of examinations such as clicks, limited abduction and asymmetrical creasing in identifying dysplasia.
Conclusion: Based on our study, the Barlow and Ortolani manoeuvres are poor predictors of dysplasia when used in isolation, but in conjunction with other elements of NIPE are more reliable than DDH risk factors in identifying sonographically-dysplastic hips.
433 - Scapular Morphometrics Predict Safe Zones and Optimal Screw Placement in Reverse Shoulder Arthroplasty
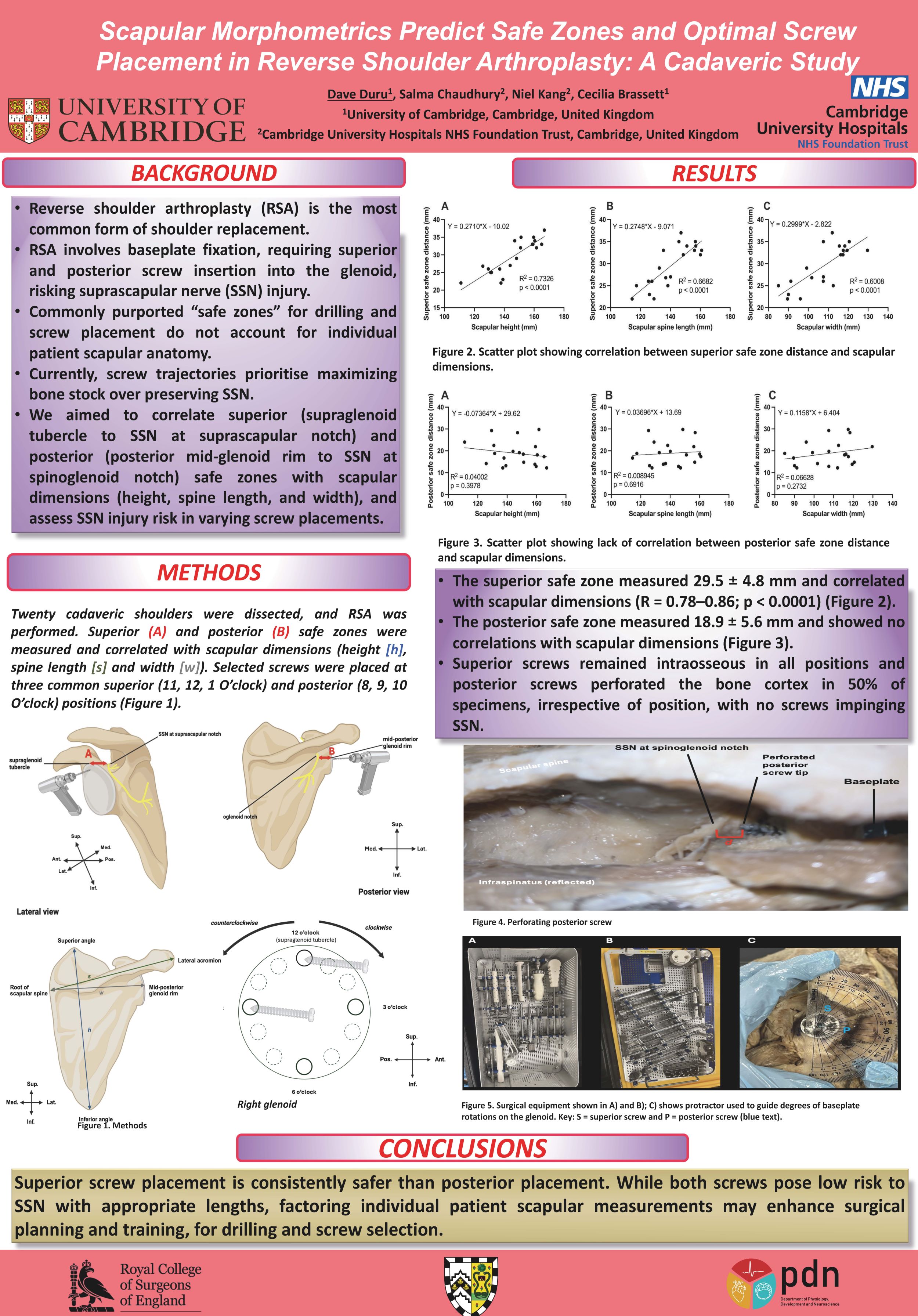
Dave Duru1, Salma Chaudhury2, Niel Kang2, Cecilia Brassett1
1University of Cambridge, Cambridge, United Kingdom. 2Cambridge University Hospitals NHS Foundation Trust, UK, Cambridge, United Kingdom
Background: Reverse total shoulder arthroplasty (rTSA) is a well-established treatment for glenohumeral joint arthritis. Glenoid baseplate fixation using peripheral screws can injure the suprascapular nerve (SSN). Current purported safe zone definitions do not account for anatomical variations and may still place SSN at risk. This study assessed if scapular morphometrics predict safe zones, and investigated optimal screw placement in rTSA.
Methods: Twenty cadaveric shoulders were dissected. The superior safe zone (distance from supraglenoid tubercle to SSN at suprascapular notch) and posterior safe zone (distance from mid-posterior glenoid rim to SSN at spinoglenoid notch) were measured. Scapular morphometrics (height, width, spine length) were recorded. Baseplates were fixed by screw insertion at standard superior (11, 12, or 1 o'clock) and posterior (8, 9, or 10 o'clock) positions. Screw lengths were determined based on glenoid depth. Cortical breach and SSN proximity were recorded. Linear regression evaluated correlations between scapular morphometrics and safe zones.
Results: The superior safe zone (mean 29.5 ± 4.8 mm) significantly correlated with scapular morphometrics (r=0.78–0.86; p<0.0001), enabling patient-specific prediction of SSN proximity. All superior screws remained intraosseous and outside the SSN path. The posterior safe zone (mean 18.9 ± 5.6 mm) showed no correlation. Posterior screws breached the cortex in 50% of specimens, at all positions (8–10 o’clock). Breached scapulae were morphometrically smaller than non-breached scapulae (unpaired t-test; p=0.027). There was no significant difference in SSN risk between the three baseplate screw configurations.
Conclusion: Scapular morphometrics reliably predict superior, but not posterior, safe zones. Smaller scapulae carry higher risk of posterior breach in rTSA (50%), suggesting caution in posterior screw selection. Common baseplate configurations display no significant difference in SSN risk, suggesting screw position should be guided by bone stock, not SSN risk. Preoperative assessment of scapular morphometry may inform patient-specific safe zones and screw selection, reducing rTSA complications
601 - Outcome of Elbow Arthroscopy in Paediatric & Adolescent Patients
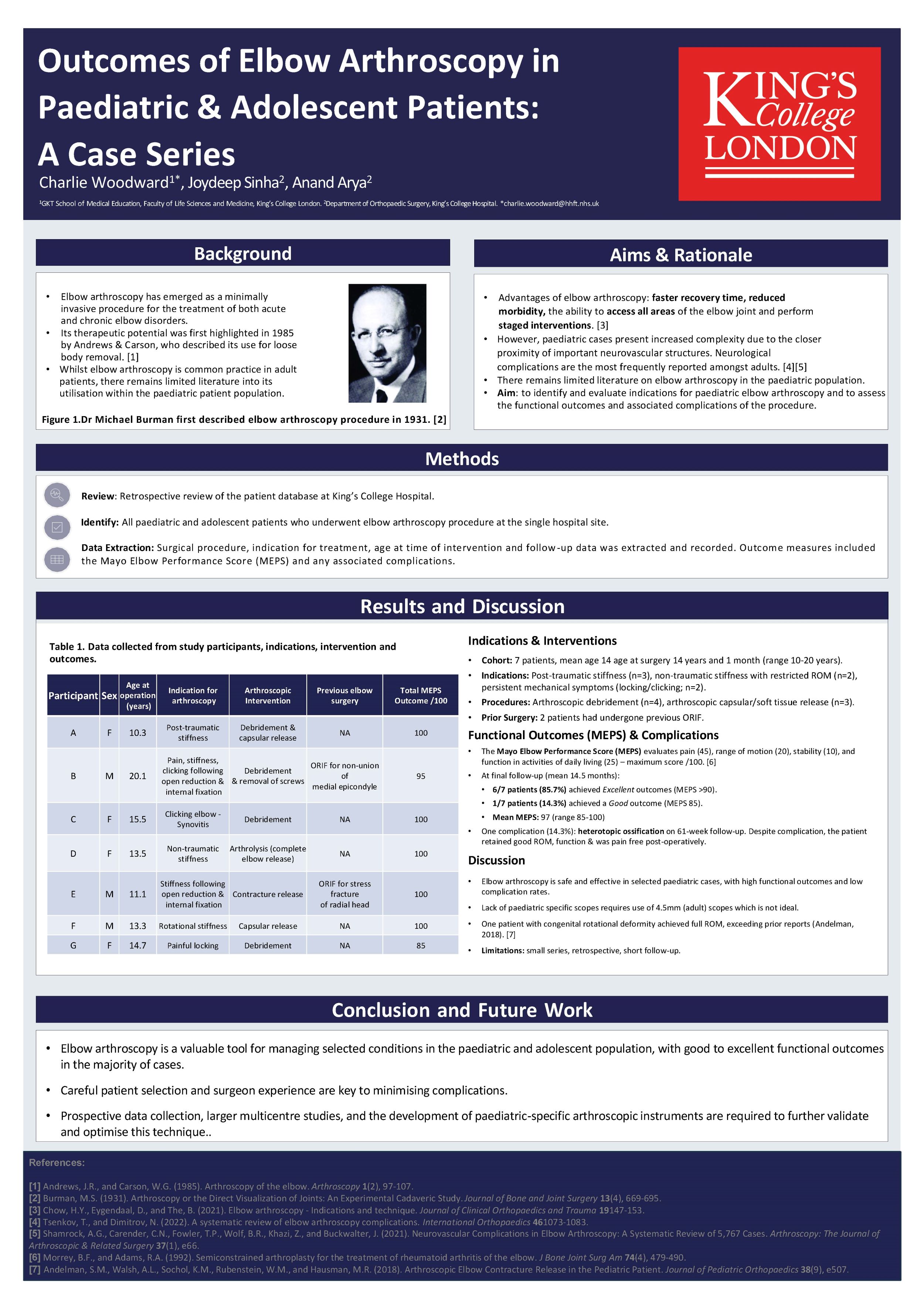
Charlie Woodward1, Joydeep Sinha2, Anand Arya2
1GKT School of Medical Education, Faculty of Life Sciences and Medicine, King's College, London, United Kingdom. 2King's College Hospital, London, United Kingdom
Elbow arthroscopy is an established procedure for managing elbow conditions. However, there is not much in the literature about its use in the paediatric patients. There is no clarity about the indications and technique of elbow arthroscopy in children and if it is different from that of adults.
We reviewed all the paediatric patients who underwent elbow arthroscopy in a tertiary referral centre. We used the adult arthroscopy set up and fluid management system. We found the standard arthroscope too long for paediatric patients but could not find any alternative. We used the wrist scope in the beginning but found it unsuitable. Portals were created with extra precaution due to increased vulnerability of neurovascular structures. Handling a long arthroscope in a small elbow needed extra efforts.
11 patients were included in this study who underwent this procedure for traumatic and non-traumatic rotational stiffness, clicky elbows, locking, OCD and stiff elbows. Average age of the patients was 14 yrs 1 month. The outcome measurement was range of movements, pain and Mayo Elbow Performance Score (MEPS). 87.5% patients achieved excellent and 14.3% achieved good outcome on MEPS. All the patients achieved functional range of movements, good function and were pain free post-operatively. We had one complication (heterotrophic ossification) in our patients which compromised the outcome. We did not find any difference between arthroscopy in children and adults.
There are not many experienced and expert elbow arthroscopist around. Lesser number of surgeons do elbow arthroscopy in children. With our experience of routinely doing elbow arthroscopy in children, we wish to disseminate the message that elbow arthroscopy in children is a useful tool in a surgeon’s armamentarium provided it is done in appropriate indications and precautions are taken to avoid the complications. A smaller arthroscope would have made the procedure slicker.
684 - Comparative Biomechanical Analysis of Sit-to-Stand and Squat Using CRAFT Metrics and MAI Motion Technology
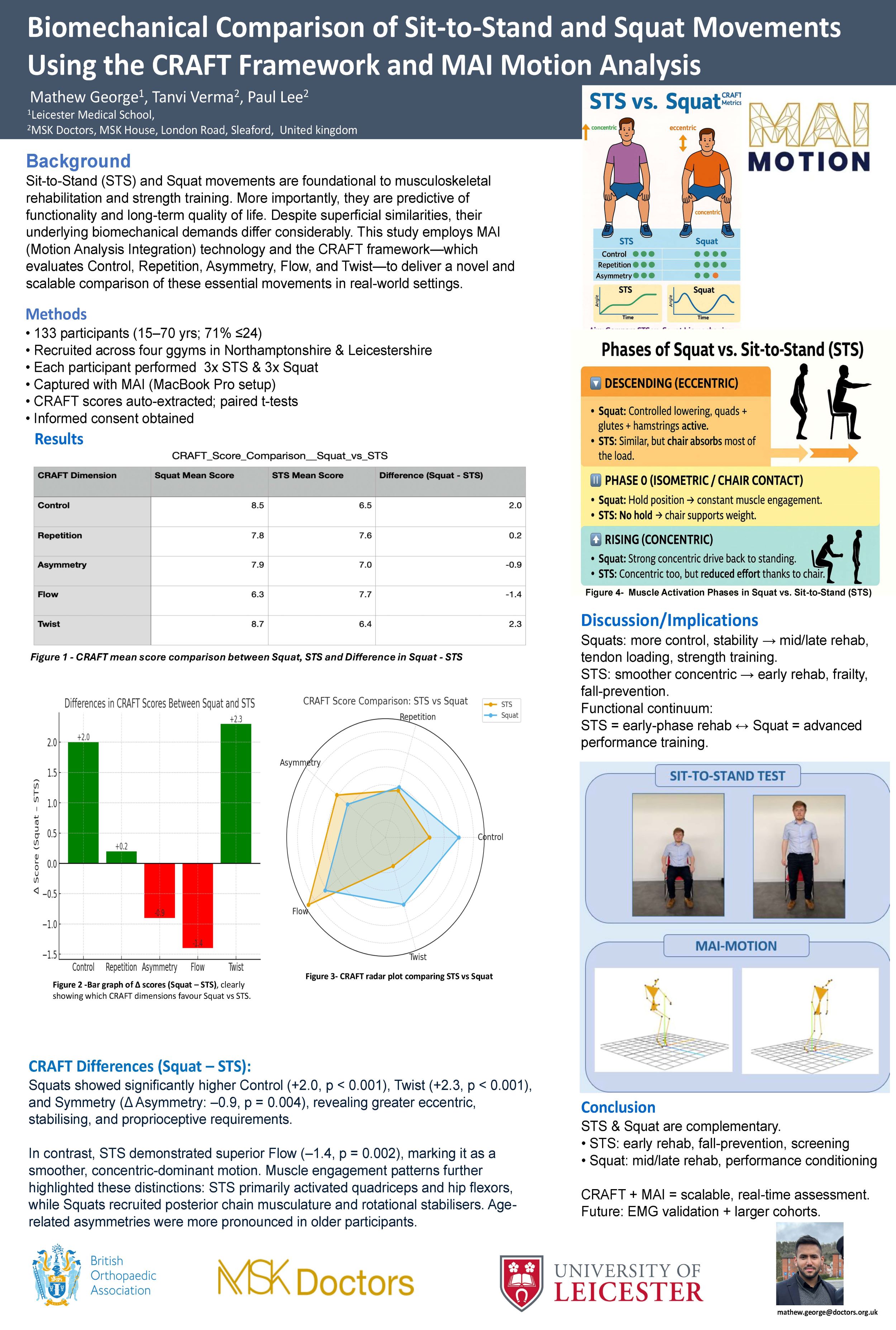
Mathew George1, Tanvi Verma2, Professor Paul Lee2
1Leicester Medical school, Leicester, United Kingdom. 2MSK doctors, Lincoln, United Kingdom
Background: Sit-to-Stand (STS) and Squat movements are foundational to musculoskeletal rehabilitation and strength training. Despite superficial similarities, their underlying biomechanical demands differ considerably. This study employs MAI (Motion Analysis Integration) technology and the CRAFT framework—which evaluates Control, Repetition, Asymmetry, Flow, and Twist—to deliver a novel and scalable comparison of these essential movements in real-world settings.
Methods: A total of 133 participants aged 15–70 were recruited from four gym locations across Northamptonshire and Leicestershire. Each individual completed three repetitions of both STS and Squat tasks, recorded using MAI software and a standardised 4-foot camera setup. CRAFT scores were computed in real time and statistically analysed using paired t-tests to detect movement quality differences.
Results: Squats showed significantly higher Control (+2.0, p < 0.001), Twist (+2.3, p < 0.001), and Symmetry (Δ Asymmetry: –0.9, p = 0.004), revealing greater eccentric, stabilising, and proprioceptive requirements. In contrast, STS demonstrated superior Flow (–1.4, p = 0.002), marking it as a smoother, concentric-dominant motion. Muscle engagement patterns further highlighted these distinctions: STS primarily activated quadriceps and hip flexors, while Squats recruited posterior chain musculature and rotational stabiliser's. Age-related asymmetries were more pronounced in older participants.
Conclusion/Findings: STS and Squat exist on a functional-to-performance continuum. STS is ideal for early rehabilitation, frailty interventions, and fall prevention. Squats are more appropriate for tendon loading, neuromuscular development, and performance progression. Movement-specific demands revealed through CRAFT scoring emphasize the importance of phase-appropriate exercise prescription.
Implications: MAI and CRAFT integration offers a practical, non-invasive tool for clinicians to monitor movement quality and guide evidence-based rehabilitation. This framework supports individualised, scalable programming and could serve as a clinical standard for functional motion auditing in orthopaedic care.
743 - Is Anterior Distal Femoral Hemiepiphysiodesis an Effective Treatment for Fixed Knee Flexion Deformity in Children with Cerebral Palsy? A Systematic Review
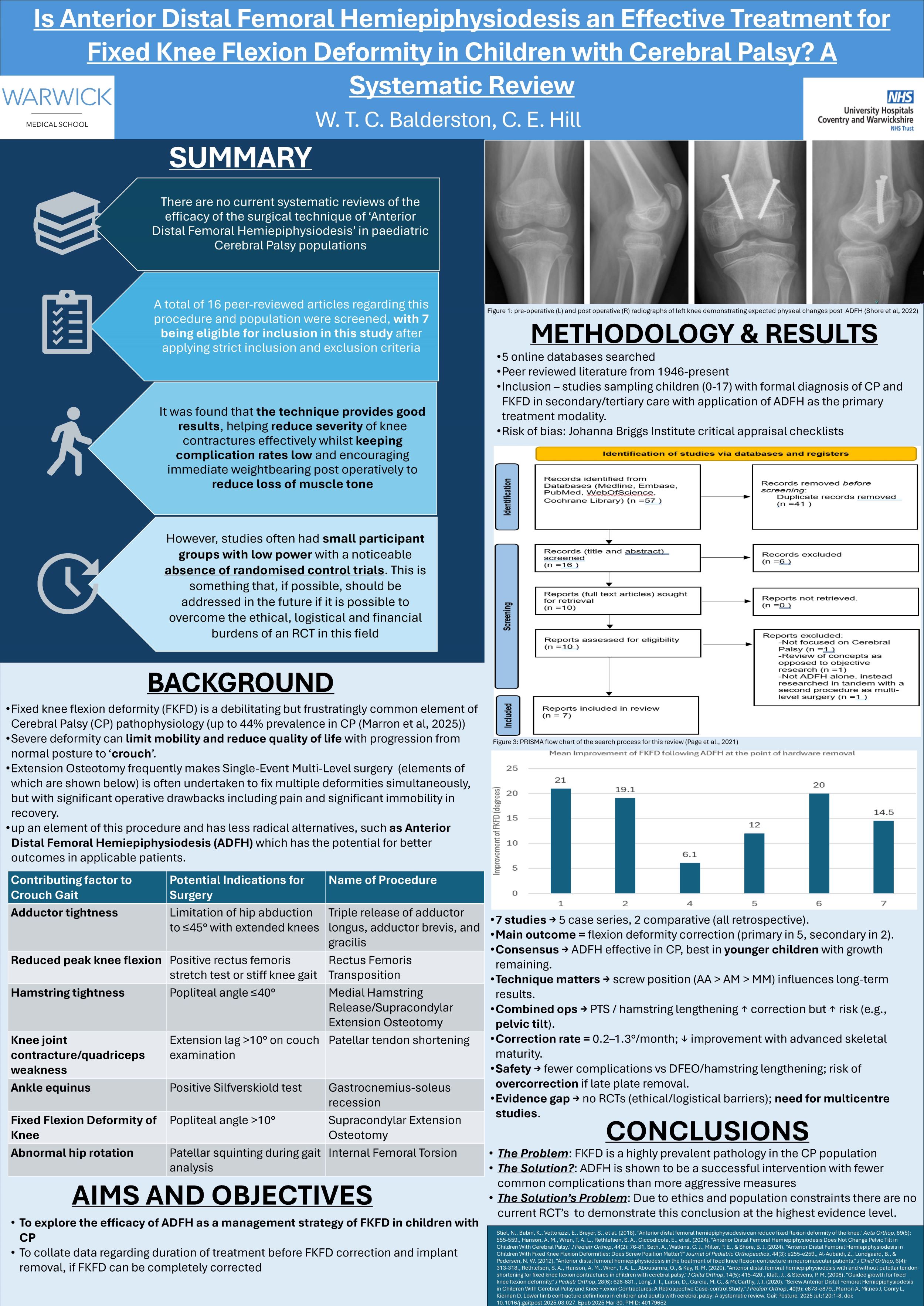
Will Balderston1, Christopher Hill2
1Warwick Medical School, Coventry, United Kingdom. 2University Hospitals Coventry & Warwickshire, Coventry, United Kingdom
Background: Anterior Distal Femoral Hemiepiphysiodesis (ADFH) is a less invasive operation for fixed knee flexion deformity (FKFD) than traditional surgical options such as extension osteotomy for cerebral palsy patients. Given appropriate skeletal immaturity, patients have the potential to gradually correct the deformity with growth whilst maintaining muscle mass with rapid return to weight-bearing. Despite published studies supporting its use, there is currently no systematic review investigating ADFH efficacy.
Aim: To establish whether ADFH is an effective technique for use in paediatric cerebral palsy patients.
Methods: A systematic review of peer-reviewed articles was conducted according to PRISMA guidelines with appropriate eligibility criteria. Once identified, eligible studies were critically appraised to form this systematic review.
Results: ADFH was found to be effective in the treatment of FKFD with an improvement in knee flexion over 12-24 months postoperatively by up to 1.3°/month up to the point of hardware removal, irrespective of the implant used. Return to weight-bearing across all studies was immediate (as tolerated by the patient). This, along with a low complication rate, heavily endorses ADFH as a surgical technique in this population.
Conclusion: This review suggests a significant future role for ADFH in paediatric orthopaedics. However, whilst it suggests ADFH is capable of managing FKFD in isolation, the results here do not necessarily suggest the replacement altogether of Single-Event Multi-Level Surgery and patient selection is critical. This review does, however, argue ADFH’s case for its vital role within this family of procedures, although higher quality evidence on the topic is warranted.
754 - Waterproof casts drying after hydration (WATCH Study): Waterproof casts dry significantly faster than traditional cast liners when tested on model limbs, a pilot study
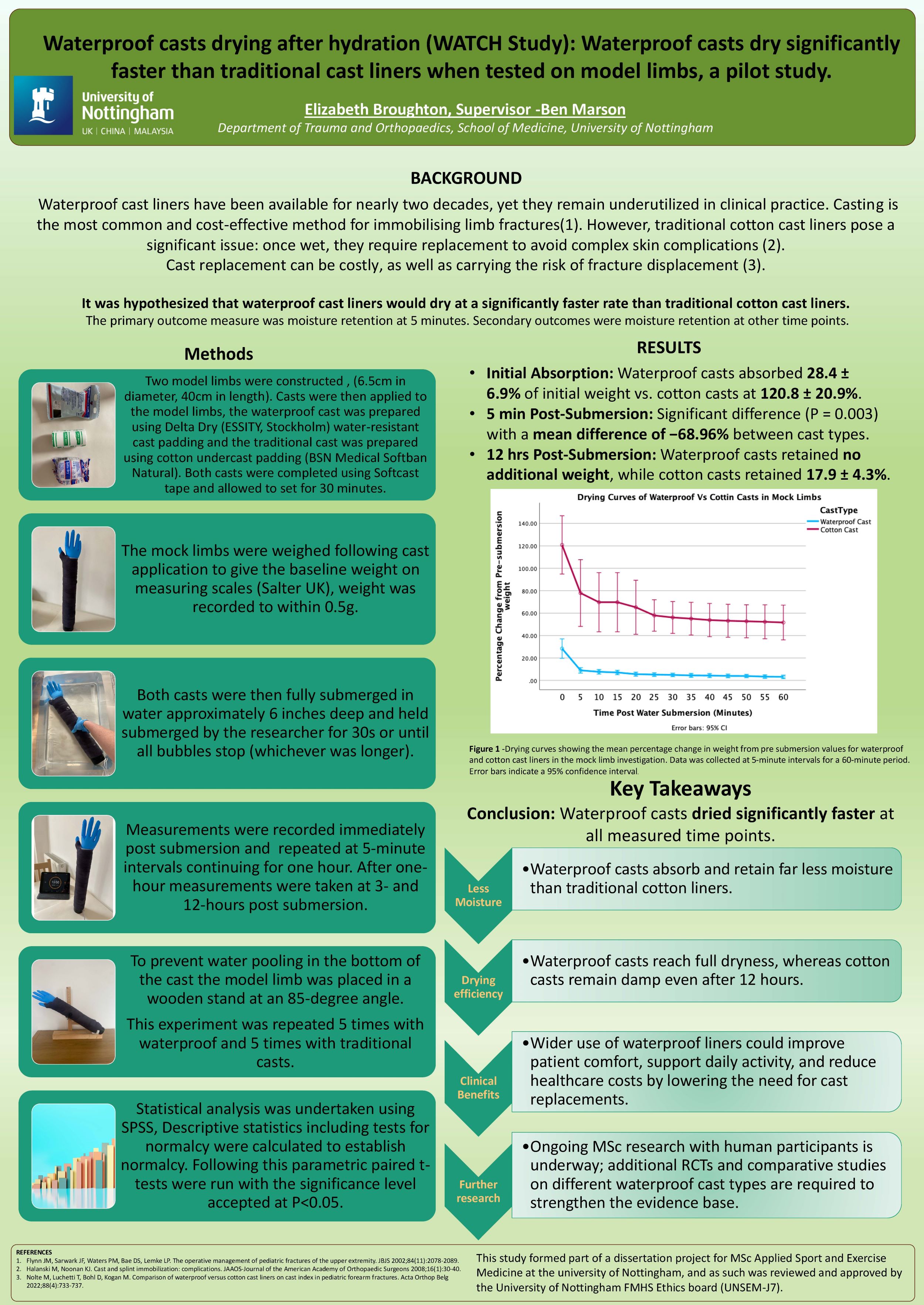
Elizabeth Broughton, Ben Marson
The University of Nottingham, Nottingham, United Kingdom
Background: Waterproof cast liners have been available for nearly two decades, yet they remain underutilized in clinical practice. Casting is the most common and cost-effective method for immobilising limb fractures. However, traditional cotton cast liners pose a significant issue: once wet, they require replacement to avoid complications. This study aims to compare the drying rates of a waterproof cast liner (Delta-Dry) with a traditional cotton liner (Softban).
Method: Two model limbs were cast: one with a cotton liner (Softban) and the other with a waterproof liner (Delta-Dry), both covered with an outer casting layer (Delta-Cast soft). Each cast was weighed, submerged in water for thirty seconds, and then weighed every five minutes for one hour, with a final measurement taken after three hours to assess water retention and drying rates.
Results: Statistical analysis was performed using GraphPad Prism. When tested using a non-parametric test to a significance level of 5%.The difference in water retention between the cotton cast liner and the delta dry liner was significant across all time points. After three hours the cotton cast liner retained 46% of its initial weight in water, whereas the delta dry had returned to its initial weight indicating complete drying.
Discussion: This study demonstrates that the Delta-Dry liner absorbs less water, dries significantly faster and after three hours, indicated complete drying in contrast to the traditional cotton liner. These findings support the case for wider clinical use of waterproof cast liners in routine fracture management and immobilisation. This would enhance patient quality of life by allowing greater participation in daily activities, reducing the burden on healthcare systems by minimizing the need for cast replacements.
Disclosure: The authors declarer no conflict of interest. This project was funded by the University of Nottingham as part of a MSc Applied Sport and Exercise Medicine course.
769 - Fast-Tracking Fracture Diagnosis The Role of AI in Radiography
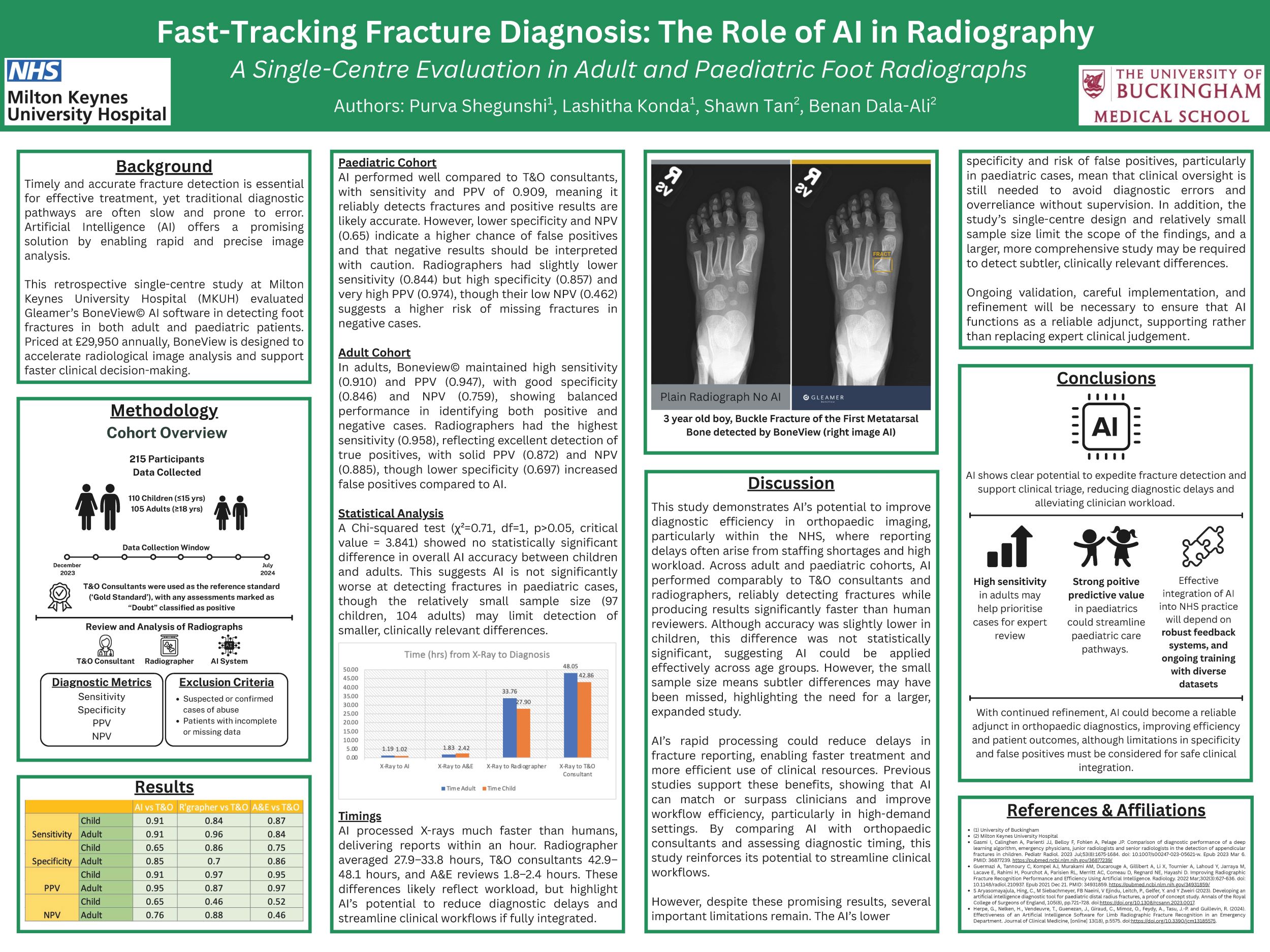
Purva Shegunshi1,2, Lashitha Konda1,2, Shawn Tan2, Benan Dala-Ali2
1University of Buckingham, Buckingham, United Kingdom. 2Milton Keynes University Hospital, Milton Keynes, United Kingdom
Background: Timely and accurate fracture detection is essential for effective treatment, yet traditional diagnostic workflows are often delayed and prone to error. Artificial intelligence (AI) offers a promising solution through rapid image analysis. This single-centre study will compare the effectiveness in detecting foot fracture in adults and children.
Methods: A total of 100 participants, 50 adults and 50 children aged ≤ 15 years, presenting with suspected foot injuries were evaluated using radiographs obtained between December 2023 to July 2024.
These images were independently assessed by a Radiographer, Accident and Emergency (A&E) doctor and Trauma and Orthopaedic (T&O) consultant for fracture detection. The T&O consultant diagnoses were used as the reference standard and cases labelled “Doubt” were treated as positive. The AI system's performance was compared in terms of sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV). The time taken for the results to be reported were also collected.
Results: The AI was significantly faster compared to radiographer, A&E and T&O review for both adults and children.
In adults, AI showed specificity and PPV of 1.00, but lower sensitivity (0.84), missing some fractures. Compared to radiographers, it showed higher sensitivity (0.92) but lower specificity (0.38), leading to more false positives.
In paediatrics, the AI achieved high sensitivity and PPV (0.95), with specificity and NPV at 0.8. Against radiographers, it showed a sensitivity (1.00) and NPV (1.00) but lower specificity (0.59) and PPV (0.83), suggesting a tendency to over-identify fractures.
Conclusion: Overall, AI shows strong potential to expedite fracture detection and support triage by flagging urgent cases and reducing clinician workload. Its high specificity in adults may help prioritise expert review, while accurate exclusion in children could streamline workflow. Future integration should include feedback loops and regular reviews to improve performance and enhance NHS care delivery.
801 - Initial assessment of suspected scaphoid fractures
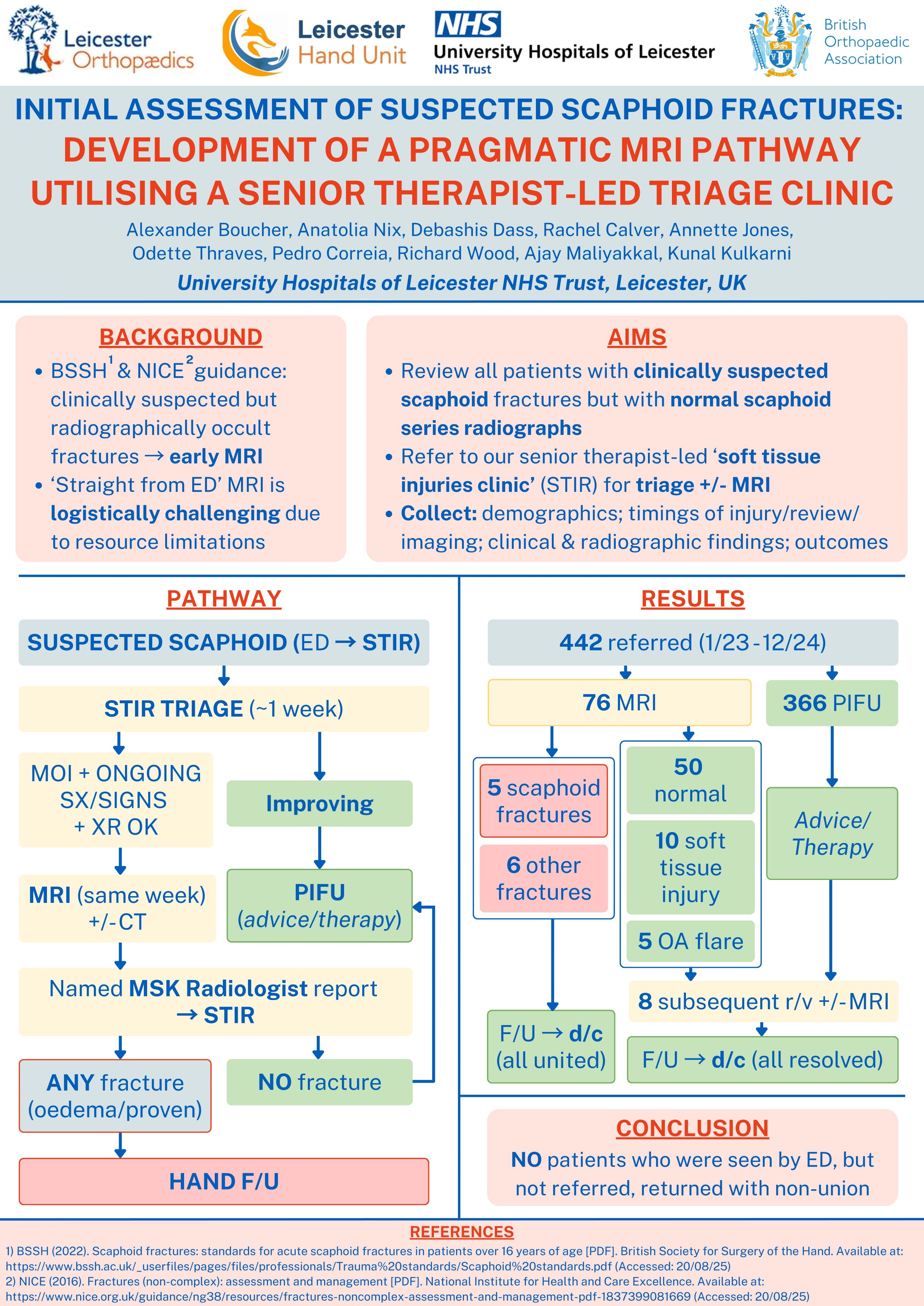
Anatolia Nix1, Alexander Boucher2, Rachel Calver2, Annette Jones2, Odette Thraves2, Pedro Correia2, Richard Wood2, Natasha Picardo3, Ajay Maliyakkal2, Kunal Kulkarni2
1University of Leicester, Leicester, United Kingdom. 2University Hospitals of Leicester NHS Trust, Leicester, United Kingdom. 3Royal Berkshire NHS Foundation Trust, Reading, United Kingdom
Abstract
Background
BSSH/NICE guidance for managing clinically suspected but radiographically occult scaphoid fractures advocate early MRI. ‘Straight from ED’ MRI referral is logistically challenging due to resource limitations. This audit assessed current practice and led to the development of a local protocol for triage via a dedicated clinic prior to selective limited-sequence rapid scaphoid MRI.
Methods
An initial audit reviewed patients with clinically suspected scaphoid fractures who would benefit from early MRI. We subsequently developed a MRI triage pathway via a senior therapist-led review clinic, and re-audited. Data collected included patient demographics; timings of injury, review, and imaging; clinical and radiographic findings; and outcomes.
Results
Our initial 9-month audit included 137 patients: 83 improved/discharged, 2 distal scaphoid fractures, 5 distal radius fractures, and 4 soft tissue injuries, leaving 43 'clinical scaphoid fractures' benefiting from MRI. After implementation of our pathway, 442 patients (average age 36 years, range 18-65) were referred to our triage clinic over a 2-year period. After triage, 74 had MRI, with the remainder referred to therapy or safely discharged. 2 received CT due to MRI contraindications. 3D imaging findings were: 50 no acute injury; 10 soft tissue pathology; 5 undisplaced scaphoid fractures (achieved union after immobilisation); 5 flares of degenerative change; 3 distal radius fractures; and 3 other undisplaced carpal fractures. Of the 10 with soft tissue pathologies identified, 8 had ongoing pain so had contrast-enhanced MRIs; these reported minor soft tissue injuries that were managed non-operatively with positive outcomes. No patients seen by ED but not subsequently referred during the reaudit period returned with non-unions.
Conclusions
Our multidisciplinary approach to triage and prompt 3D imaging of suspected scaphoid fractures has proven successful. Proactive engagement between ED, orthopaedics, radiology and therapy has allowed effective balance of demand with supply in a resource constrained environment.
806 - Use of mini C-arm machines in minor foot & ankle procedures and injections shows reduced costs and carbon emissions compared to traditional C-arm machines improving environmental sustainability
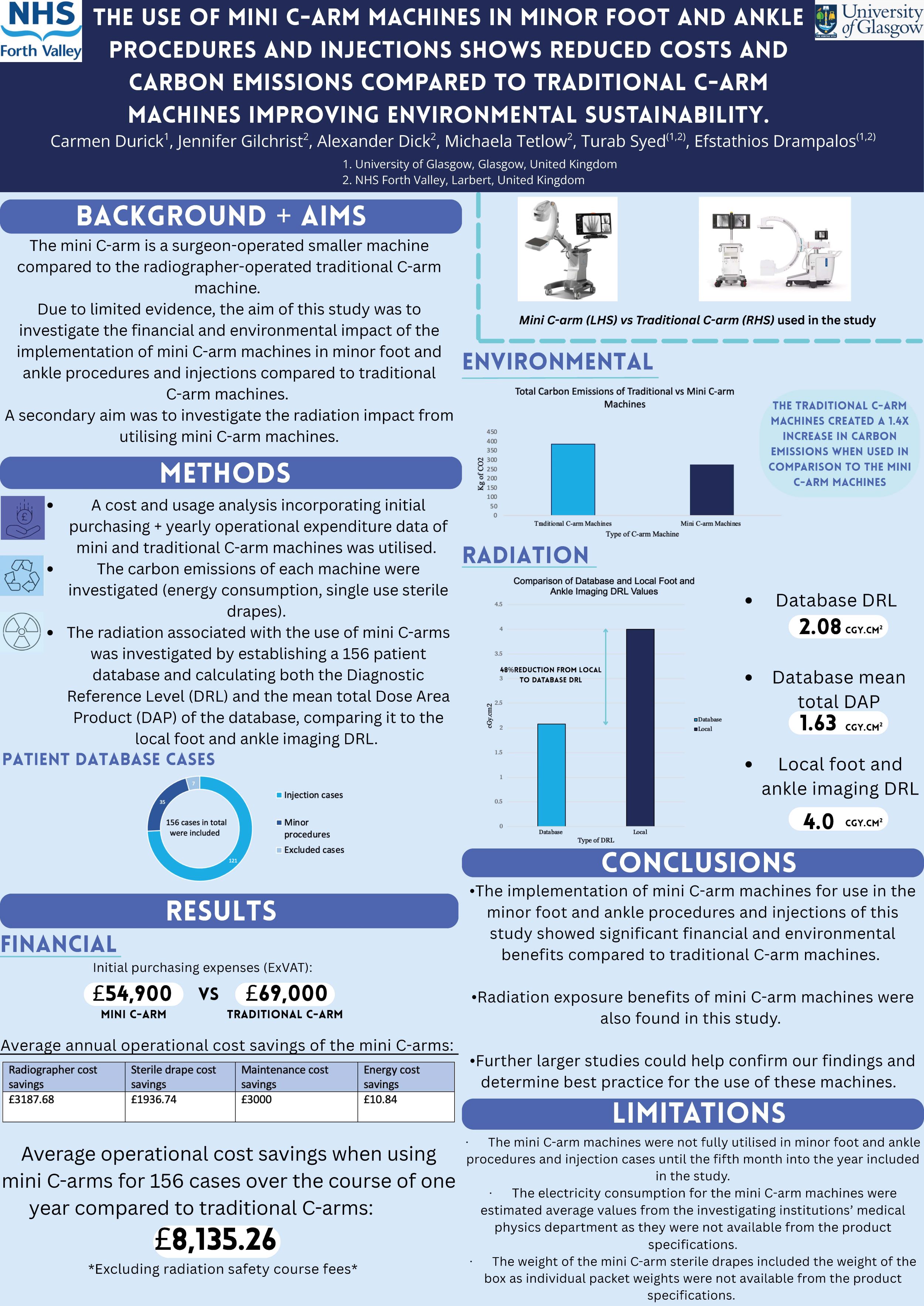
Carmen Durick1, Jennifer Gilchrist2, Alexander Dick2, Michaela Tetlow2, Turab Syed1,2, Efstathios Drampalos1,2
1University of Glasgow, Glasgow, United Kingdom. 2NHS Forth Valley, Larbert, United Kingdom
Background: The mini C-arm is a surgeon-operated smaller machine compared to the radiographer-operated traditional C-arm machine. There is limited data for the financial and environmental impact of the use of mini C-arm machines in minor foot and ankle procedures and injection cases.
Methods: We did a cost and usage analysis including initial purchasing price and yearly operational expenditures of mini C-arms versus traditional C-arms, along with investigating the carbon emissions of each machine. We also studied aspects of the radiation impact of utilising mini C-arm machines. A database consisting of 156 minor foot and ankle procedures and injections was created.
Results: There were operational cost savings of £8,135.26 for the 156 cases over the course of one year when utilising mini C-arms instead of traditional C-arms, excluding radiation safety course fees. The traditional C-arms created 1.4 times increase (385.508 to 274.088kg of CO2) in carbon emission output compared to mini C-arms, which demonstrated obvious environmental implications. A diagnostic reference level (DRL) was calculated for the database, producing a 48% lower value compared to the local DRL for foot and ankle imaging (2.08 to 4cGy.cm2). The mini C-arm mean total dose area product (DAP) at 1.63cGy.cm2 was found to be reduced compared to the local DRL at 4cGy.cm2.
Conclusion: For the minor foot and ankle procedures and injections of this study, the mini C-arm machines have shown significant financial and environmental benefits compared to the traditional C-arm machines. Radiation exposure benefits of the mini C-arm machines were also seen in this study. Further larger studies could help confirm our findings and determine best practice for the use of these machines.
Disclosure: The authors of this study have no conflicts of interest to declare.
Paediatrics
453 - The children’s urgent reduction of forearm fractures in emergency department (CURFFED) project: National prospective trainee-led collaborative audit of practice and perceived barriers to change
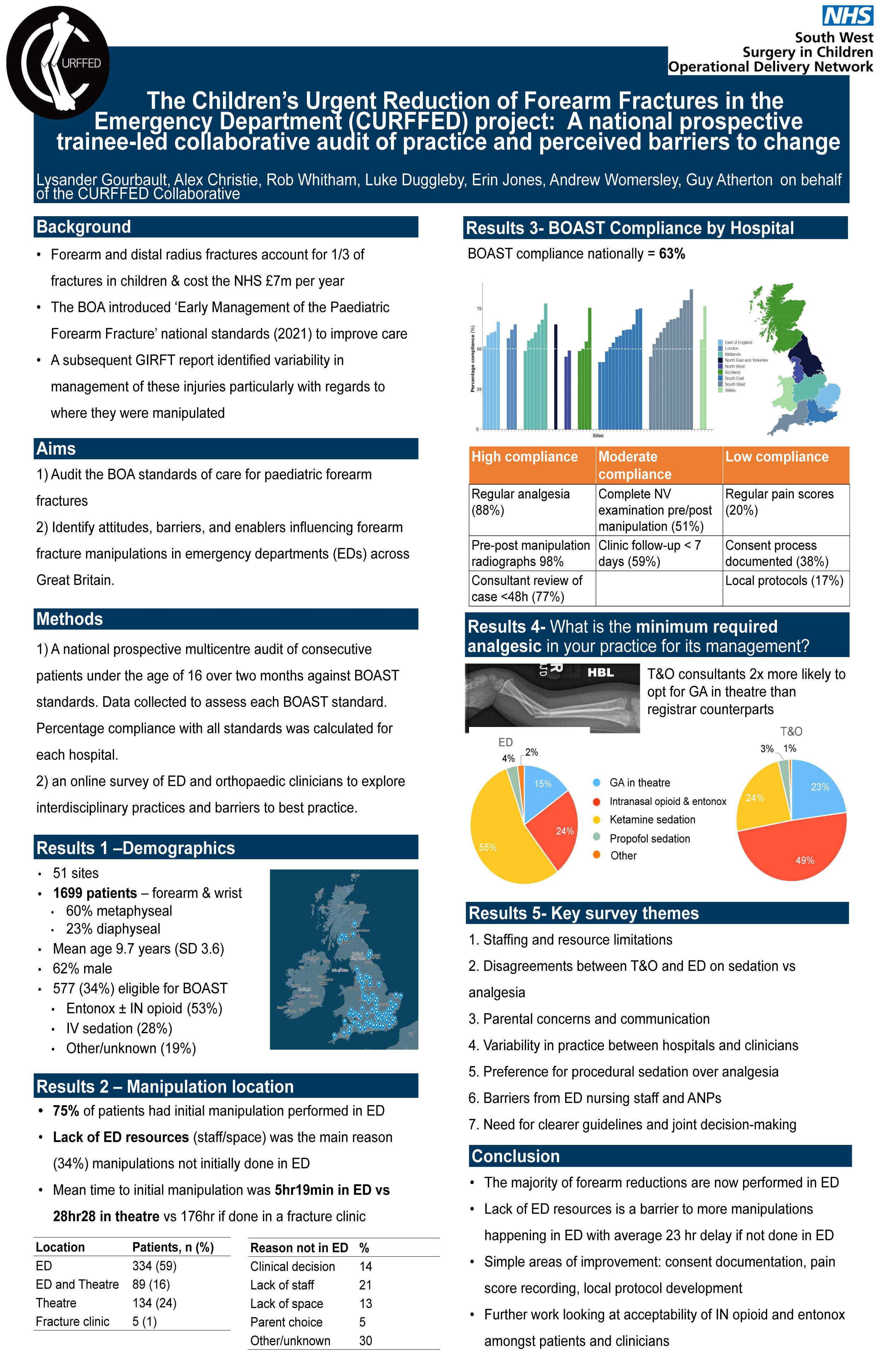
Lysander Gourbault1, Robert Whitham1, Luke Duggleby2, Alexander Christie3, Erin Jones3, Andrew Wormersley3, William Guy Atherton1, CURFFED Collaborative4
1Bristol Royal Hospital for Children, Bristol, United Kingdom. 2Gloucester Hospitals NHS Trust, Gloucester, United Kingdom. 3Royal United Hospital, Bath, United Kingdom. 4South West Surgery in Children Operational Delivery Network, Bristol, United Kingdom
Background: Forearm and distal radius fractures account for 1/3 of fractures in children & cost the NHS £7m per year. The BOA introduced ‘Early Management of the Paediatric Forearm Fracture’ national standards (2021) to improve care. A subsequent GIRFT report identified variability in management of these injuries particularly with regards to where they were manipulated.
We aimed to 1) audit the above BOA standards of care and 2) identify attitudes, barriers, and enablers influencing forearm fracture manipulations in emergency departments (EDs) across Great Britain.
Method: The CURFFED project consisted of 1) a prospective audit of consecutive patients over two months against BOAST standards, and 2) an online survey of ED and orthopaedic clinicians to explore interdisciplinary practices and barriers to best practice.
Results: Data from 1699 patients across 51 hospitals were included. Average age was 9.7 years (62% male). Most fractures were metaphyseal distal radius fractures (60%). Of the 577 patients eligible for ED manipulation, 423 (73%) were managed in ED; 89 (21%) required subsequent theatre manipulation. IV sedation was used in 28% (n=120). Overall audit compliance to BOAST standards was 63%. Among 223 theatre cases, 84 (38%) involved instrumentation.
There were 683 survey responses from clinicians of varying grades and specialties across 72 hospitals (representing 45% of UK EDs). Procedural sedation was deemed the minimum requirement for forearm mid-shaft fracture manipulation by 41% of respondents. Orthopaedic consultants were more likely to advocate for theatre reduction for BOAST-eligible fractures than registrars (OR 1.9). Key barriers to ED manipulation included lack of physical space (50.4%) and staff availability (65.7%).
Conclusions: The CURFFED project highlights variability in managing paediatric fractures despite established standards. Collaborative efforts between T&O and EDs are essential to overcome logistical barriers and ensure best care for our patients.
Disclosures: No disclosures.
835 - Artificial intelligence assistance improves clinician performance in diagnosing developmental dysplasia of the hip
Abhinav Singh1, Allison Clement2, Gary Collins1, Sarim Ather3, Deborah Eastwood4, Daniel Perry1
1Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, Oxford, United Kingdom. 2University of Oxford, Oxford, United Kingdom. 3Oxford University Hospitals, Oxford, United Kingdom. 4Royal National Orthopaedic Hospital, London, United Kingdom
Background: Artificial intelligence (AI) models have shown reasonable ability in identifying developmental dysplasia of the hip (DDH). This study evaluates the impact of AI-assisted image interpretation on the diagnostic performance of ‘expert’ and ‘non-expert’ clinicians.
Methods: A multi-reader, multi-case study was conducted with 10 readers (5 consultants and 5 registrars). The study included 70 static 2D hip ultrasound scans from 70 unique patients (age range 0.86-19.86 weeks, mean age 8.6 weeks, 55.7% female and 65.7% left). There were 35 normal (Graf 1) and 35 abnormal (Graf 2 n=25; Graf 3/4 n=10) images. The reference standards were the Graf alpha angle and femoral head coverage (FHC) derived from anatomical points (landmarks) checked by two senior experts. The clinicians placed landmarks without (Phase1) and with AI assistance (Phase2). Their diagnostic performance (sensitivity/specificity), confidence rating (1-5) and time taken were reported.
Results: For the Graf method, the mean sensitivity/specificity values for ‘experts’ without vs with AI were 0.75/0.93 vs 0.71/0.96, respectively. For ‘non-experts’, this was 0.75/0.90 vs 0.70/0.95. For FHC%, the sensitivity/specificity values for ‘experts’ (0.97/0.92) and ‘non-experts’ (0.98/0.93) were unchanged between phases. AI assistance significantly increased the rate that all clinicians reported the highest level of confidence (5) in their annotations. The mean time taken (hh:mm) by ‘experts’ without vs with AI was 04:49 vs 05:07, for ‘non-experts’ it was 05:04 vs 04:52.
Conclusion: The FHC demonstrated better overall sensitivity as a screening method. AI assistance improved the diagnostic confidence of all clinicians without reducing their performance and made ‘non-experts’ faster.
Implications: AI-assisted diagnostics can improve clinician performance and may have a role in upskilling non-expert clinicians.
Disclosure: None
Quality Improvement
8 - A qualitative study exploring stakeholder perspectives on wrist injury pathways in the UK NHS
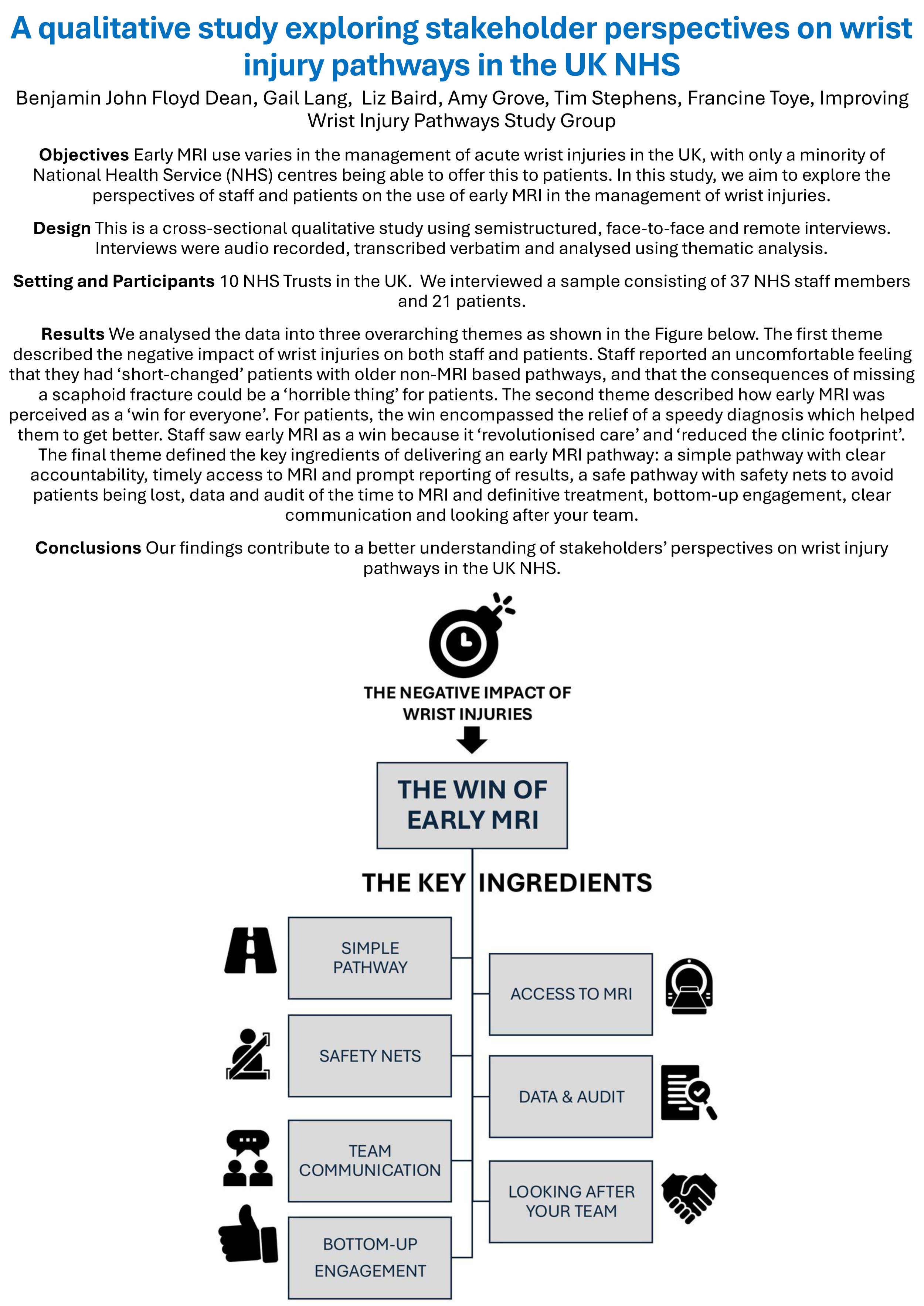
Benjamin Dean1,2, Toye Francine1, Liz Baird1, Amy Grove3, Matt Costa2, Tim Stephens4
1Oxford University Hospitals NHS Trust, Oxford, United Kingdom. 2NDORMS - University of Oxford, Oxford, United Kingdom. 3University of Birmingham, Birmingham, United Kingdom. 4QMUL, London, United Kingdom
Background: Early MRI use varies in the management of acute wrist injuries the UK with only a minority of NHS centres being able to offer this patients. In this study, we aim to explore the perspectives of staff and patients on the use of early MRI in treatment of wrist injuries such as scaphoid fracture.
Methods: Transcribed verbatim and analysed using thematic analysis. Setting: 10 NHS Trusts the United Kingdom. Participants: we interviewed a sample consisting of 37 NHS staff members and 21 patients.
Results: We analysed the data into three overarching themes. The first theme described the negative impact of scaphoid fractures of both staff and patients. Staff reported an uncomfortable feeling that they had “short-changed”patients, that the consequences of missing a scaphoid fracture could be a “horrible thing” for patients. The second theme described how early MRI was perceived as a “win for everyone”. For patients, the win encompassed the relief of a speedy diagnosis which helped them to get better. Staff saw early MRI as win because it “revolutionised care” and “reduced the clinic footprint”. The final theme, defined the key ingredients of delivering an early MRI pathway: a simple pathway with clear accountability , timely access to MRI and prompt reporting of results, a safe pathway with safety nets to avoid patients being lost, data and audit of the time to MRI and definitive treatment, bottom-up engagement, clear communication and caring within teams.
Conclusions: Our findings contribute to a better understanding of stakeholders’ perspectives on wrist injury pathways in the UK NHS.
Implications - this study has identified the seven ingredients to delivering an effective wrist injury pathway with early MRI
111 - Impact of ‘Joint School’ on the Rehabilitation Pathway of Primary Total Hip and Knee Arthroplasties

Saurabh Sarkar, Manish Divekar, Ilona Babich
Royal Cornwall Hospital NHS Trust, Truro, United Kingdom
Introduction: In England and Wales, between 150,000 and 200,000 primary hip and knee replacements are performed yearly, with projections indicating this number will surge to 268,107 by 2060. UK hospital trusts are actively enhancing perioperative patient services to meet this growing demand. An effective strategy for improving recovery is by the implementation of preoperative 'Joint Schools', where patients participate in a session prior to surgery to understand the recovery process, anticipated length of stay, and the responsibilities of the multidisciplinary team. The authors have compared the outcomes of patients who attended the Joint School to those who did not.
Methods: This non-randomized study analyzed two groups of 53 adult patients in each group, all scheduled for elective primary hip or knee Arthroplasties. Patients with revision surgeries, significant mobility issues, or delayed physiotherapy were excluded. The first group underwent surgery without the Joint School service, while the second group received the service before surgery. Comprehensive data was collected on demographics, with the primary outcome focused on the time taken to achieve Physiotherapy goals.
Results: The first group (mean age 65.23 years, BMI 30.78, ASA 1.94) required an average of 1.87 days to meet their physiotherapy goals. In contrast, the second group (mean age 68.74 years, BMI 29.58, ASA 1.96) achieved their goals in an average of just 1.38 days (P < 0.001).
Conclusion: Patients who received the Joint School service prior to their surgery, experienced significantly faster recovery times and felt better prepared for surgery. This study supports the widespread adoption of Joint Schools as a vital part of prehabilitation, emphasizing their crucial role in reducing post-operative hospital stays.
270 - Dislocation After Hip Arthroplasty - Clinical Burden and Cost Insights from a Six-Year Single-Centre Review
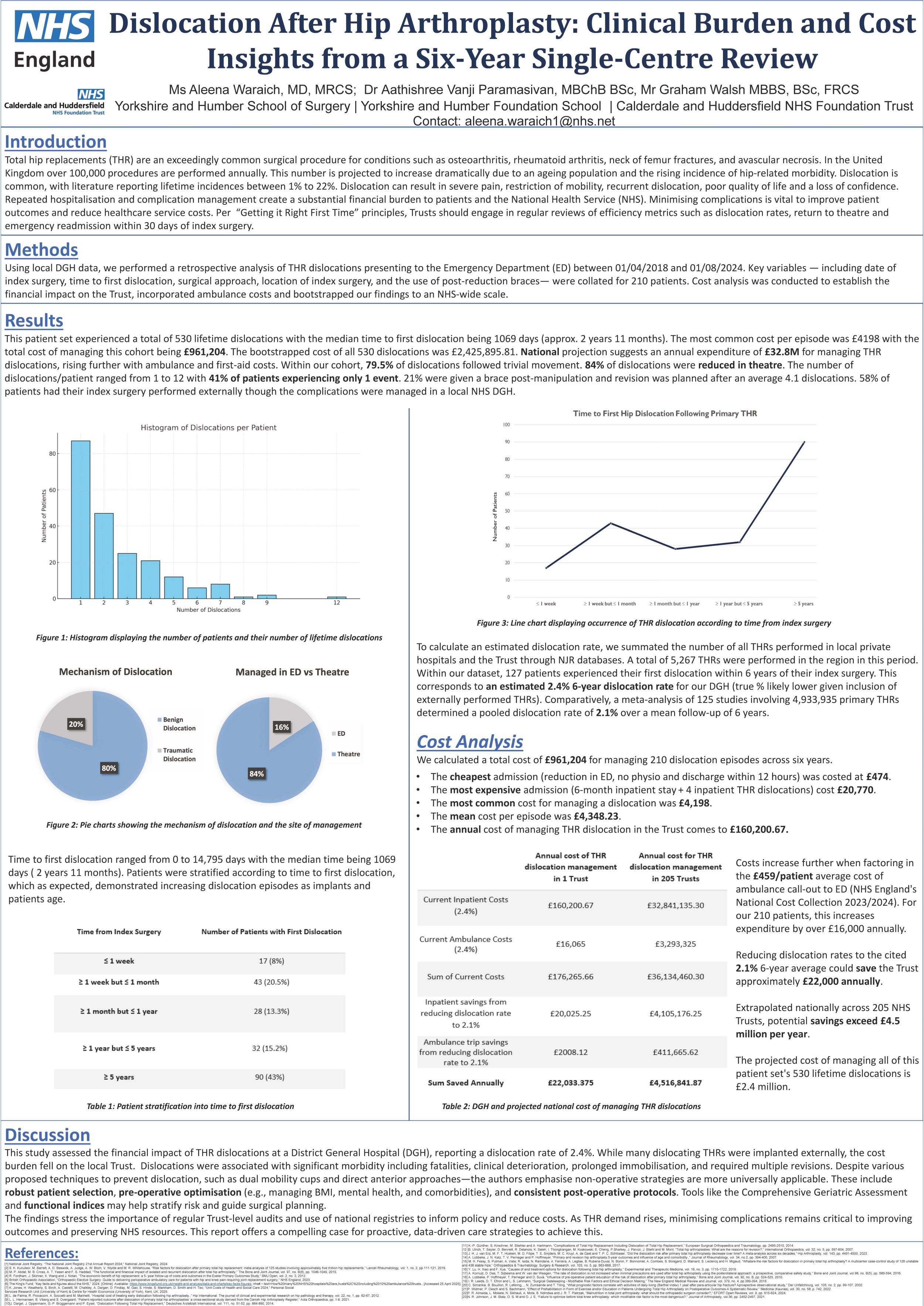
Aleena Waraich1, Aathishree Paramasivan2, Graham Walsh3
1Yorkshire & Humber School of Surgery, Leeds, United Kingdom. 2Yorkshire & Humber Foundation School, Leeds, United Kingdom. 3Calderdale and Huddersfield NHS Foundation Trust, Huddersfield, United Kingdom
Background: Dislocation following total hip replacement (THR) is a well-recognised complication, impacting patient outcomes, confidence, and healthcare expenditure. With the increasing popularity of THRs, the cost burden of this complication is likely to rise further.
Methods: Using data from one District General Hospital, we performed a retrospective analysis of THR dislocations presenting to the Emergency Department between 01/04/2018 and 01/08/2024. Key variables — including date of index surgery, time to first dislocation, surgical approach, site of index surgery, and adherence to hip precautions — were collated for 210 patients. Cost analysis was conducted to establish the financial impact on the Trust.
Results: This cohort experienced 530 lifetime dislocations, with a median time to first dislocation of 1069 days (~ 2 years 11 months). The mode cost of managing these episodes was £4,198 (mean £4,348) with the total cohort management cost of £961,204. Extrapolated, the hypothetical cost of managing all 530 dislocations within the Trust was £2,425,895.81. National projection suggests an annual expenditure of £32.8M for managing THR dislocations, rising further with ambulance and first-aid costs.
79.5% of dislocations followed benign movements. 84% were reduced in theatre. Dislocations ranged from 1 to 12 per patient, with 41% of patients experiencing only 1 event. 21% were fitted with brace post-manipulation, and revision surgery was planned after an average of 4.1 dislocations. 58% of patients had their index surgery performed externally, although the cost of management was borne locally.
Conclusion: Methods to minimise dislocation rates are extensively researched and often debated amongst arthroplasty surgeons. Early identification of high-risk cases and appropriate patient selection per pre-operative screening and activity indices may help reduce dislocation rates and national healthcare costs. Regularly performed Trust-level audits may provide the data to inform national policy on reducing healthcare costs.
343 - Improving Trainees Experience of TIme out of Training for Parental Leave
Alexandra Haddon1,2, Kirsty Milne1,2
1Orthopaedic Registrar, SE Scotland Rotation, United Kingdom. 2Royal Infirmary Edinburgh, Edinburgh, United Kingdom
Background: Parental leave has unique considerations for time out of training. Whilst SuppoRRT is well established by Health Education England, there are few courses available within Scotland to assist with this transition. Trainees often feel information is hard to access, contradictory or vague. Due to the variables surrounding parental leave – timings; duration; return to training (RTT) - this key point in any trainees’ career requires consideration.
Methods: We organised the inaugural return to work event for Surgeons and Anaesthetists. This was a pan Scotland event – open to any surgical speciality, obstetrics and gynaecology and anaesthetics. Topics included return to work and breastfeeding, maternal wellbeing from a psychiatrist, performance anxiety and confidence building from a psychologist and the BMA on employment matters.
Results: Delegates and babies attended representing: Anaesthetics, O&G, T&O and Gen Surg, from South East, West and North of Scotland. The pre-workshop questionnaire had respondents from: CT2-ST7. Some had previously experienced a return to work and 2 used a KIT for the workshop. Findings showed all respondents had anxiety regarding RTT. Concerns included: Skill fade, managing sleep deprivation, juggling being a parent and doctor and feeding. 6 delegates had had a pre-leave meeting, 9 had tried to find more support about returning (peers, online information); one thought enough support was available.
The post workshop questionnaire showed 100% said their confidence had been boosted by the workshop and that the workshop was relevant to them. There was positive feedback to all aspects of the course. 100% of delegates would re-attend the workshop after future periods of leave – “shared experience is the most beneficial thing”.
Conclusion: The course has resoundingly positive feedback. The demand is there and the course has helped delegates preparation for RTT. This is now an annual event with the second workshop being held in Summer 25.
367 - From Paper to Platform Digitising orthopaedic trauma pathways to deliver timely, person-centred care
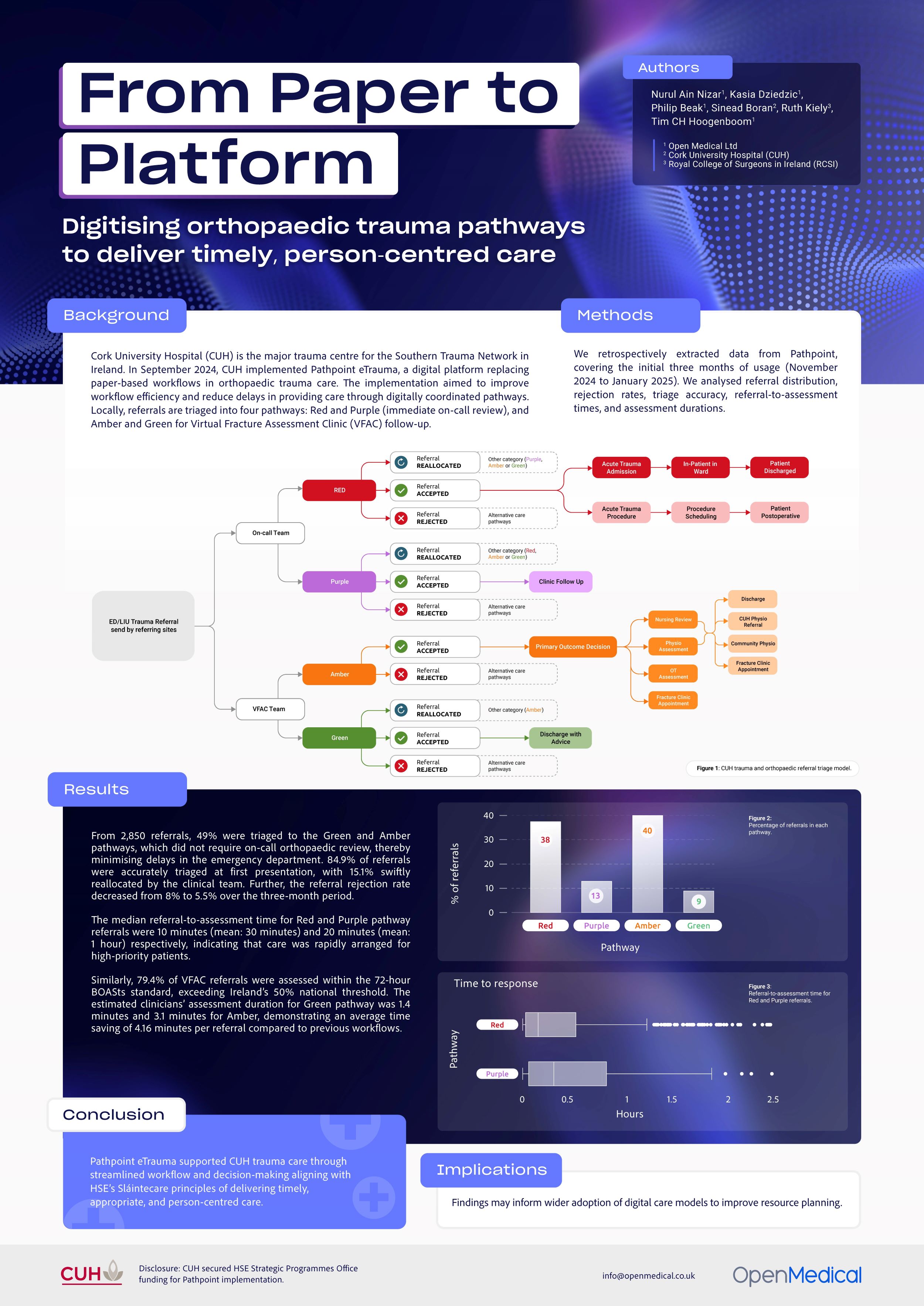
Nurul Ain Nizar1, Kasia Dziedzic1, Philip Beak1, Sinead Boran2, Ruth Kiely3, Tim CH Hoogenboom1
1Open Medical Ltd, London, United Kingdom. 2Cork University Hospital, Cork, Ireland. 3Royal College of Surgeons in Ireland, Dublin, Ireland
Background: Cork University Hospital (CUH) is the major trauma centre for the Southern Trauma Network in Ireland. In September 2024, CUH implemented Pathpoint eTrauma, a digital platform replacing paper-based workflows in orthopaedic trauma care. The implementation aimed to improve workflow efficiency and reduce delays in providing care through digitally coordinated pathways. Locally, referrals are triaged into four pathways: Red and Purple (immediate on-call review), and Amber and Green for Virtual Fracture Assessment Clinic (VFAC) follow-up.
Methods: We retrospectively extracted data from Pathpoint, covering the initial three months of usage (November 2024 to January 2025). We analysed referral distribution, rejection rates, triage accuracy, referral-to-assessment times, and assessment durations.
Results: From 2,850 referrals, 49% were triaged to the Green and Amber pathways, which did not require on-call orthopaedic review, thereby minimising delays in the emergency department. 84.9% of referrals were accurately triaged at first presentation, with 15.1% swiftly reallocated by the clinical team. Further, the referral rejection rate decreased from 8% to 5.5% over the three-month period.
The median referral-to-assessment time for Red and Purple pathway referrals were 10 minutes (mean: 30 minutes) and 20 minutes (mean: 1 hour) respectively, indicating that care was rapidly arranged for high-priority patients.
Similarly, 79.4% of VFAC referrals were assessed within the 72-hour BOASts standard, exceeding Ireland’s 50% national threshold. The estimated clinicians’ assessment duration for Green pathway was 1.4 minutes and 3.1 minutes for Amber, demonstrating an average time saving of 4.16 minutes per referral compared to previous workflows.
Conclusion: Pathpoint eTrauma supported CUH trauma care through streamlined workflow and decision-making aligning with HSE’s Sláintecare principles of delivering timely, appropriate, and person-centred care.
Implications: Findings may inform wider adoption of digital care models to improve resource planning.
Disclosure: CUH secured HSE Strategic Programmes Office funding for Pathpoint implementation.
375 - Validating an AI tool used to predict mortality and morbidity in elective hip + knee arthroplasty – a QIP
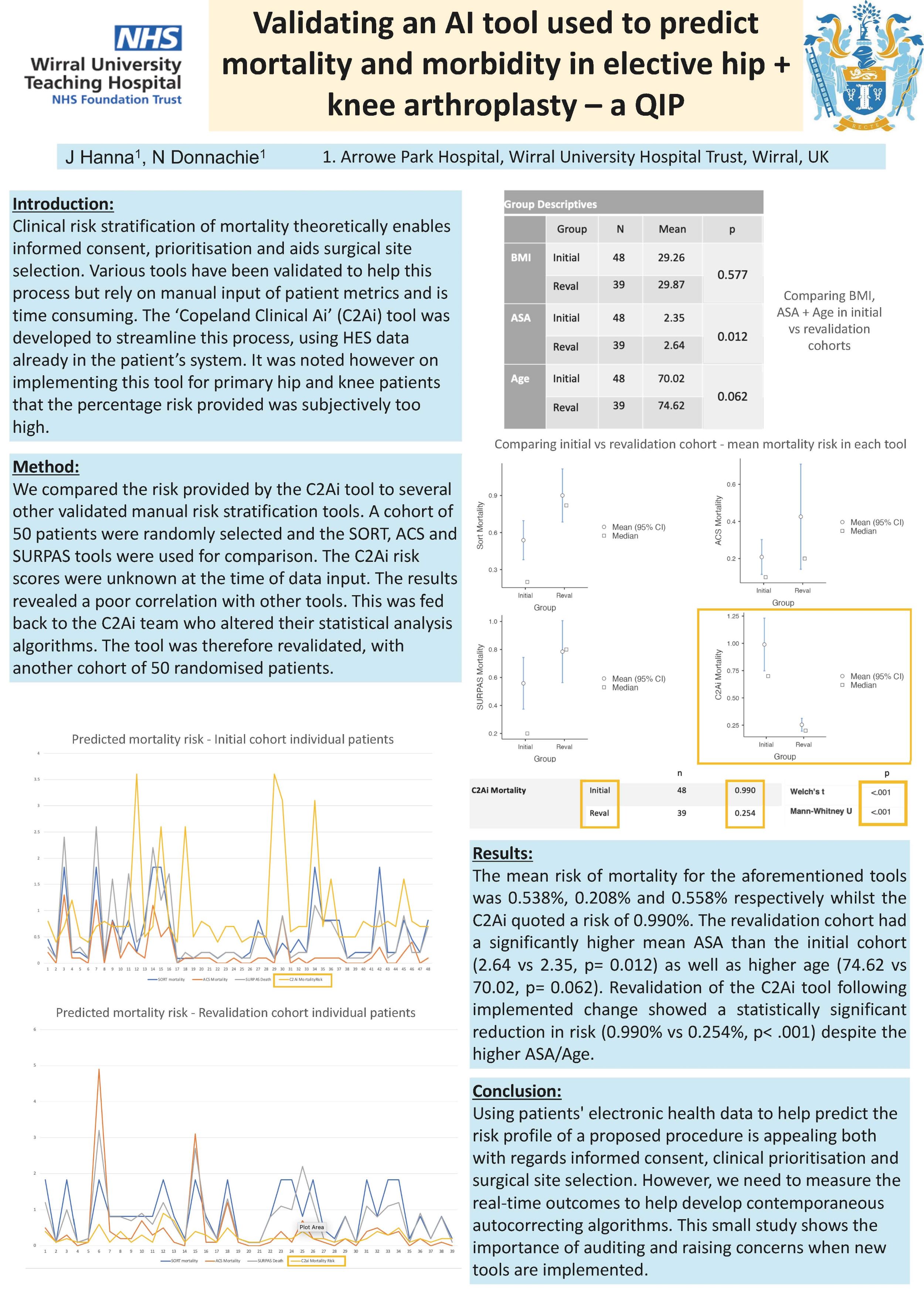
Joseph Hanna, Nigel Donnachie
Wirral University Teaching Hospital NHS Foundation Trust, Wirral, United Kingdom
Background: Clinical risk stratification of mortality theoretically enables informed consent, prioritisation and aids surgical site selection. Various tools have been validated to help this process but rely on manual input of patient metrics and is time consuming. The ‘Copeland Clinical Ai’ (C2Ai) tool was developed to streamline this process, using HES data already in the patient’s system. It was noted however on implementing this tool for primary hip and knee patients that the percentage risk provided was subjectively too high.
Methods: We compared the risk provided by the C2Ai tool to several other validated manual risk stratification tools. A cohort of 50 patients were randomly selected and the SORT, ACS and SURPAS tools were used for comparison. The C2Ai risk scores were unknown at the time of data input. The results revealed a poor correlation with other tools. This was fed back to the C2Ai team who altered their statistical analysis algorithms. The tool was therefore revalidated, with another cohort of 50 randomised patients.
Results: The mean risk of mortality for the aforementioned tools was 0.538%, 0.208% and 0.558% respectively whilst the C2Ai quoted a risk of 0.990%. The revalidation cohort had a significantly higher mean ASA than the initial cohort (2.64 vs 2.35, p=0.012) as well as higher age (74.62 vs 70.02, p= 0.062). Revalidation of the C2Ai tool following implemented change showed a statistically significant reduction in risk (0.990% vs 0.254%, p< .001) despite the higher ASA/Age.
Conclusions: Using patients electronic health data to help predict the risk profile of a proposed procedure is appealing both with regards informed consent, clinical prioritisation and surgical site selection. However, we need to measure the real-time outcomes to help develop contemporaneous autocorrecting algorithms. This small study shows the importance of auditing and raising concerns when new tools are implemented.
398 - Implant Ownership Post-Removal: Bridging MHRA Guidance and Clinical Practice in Orthopaedics
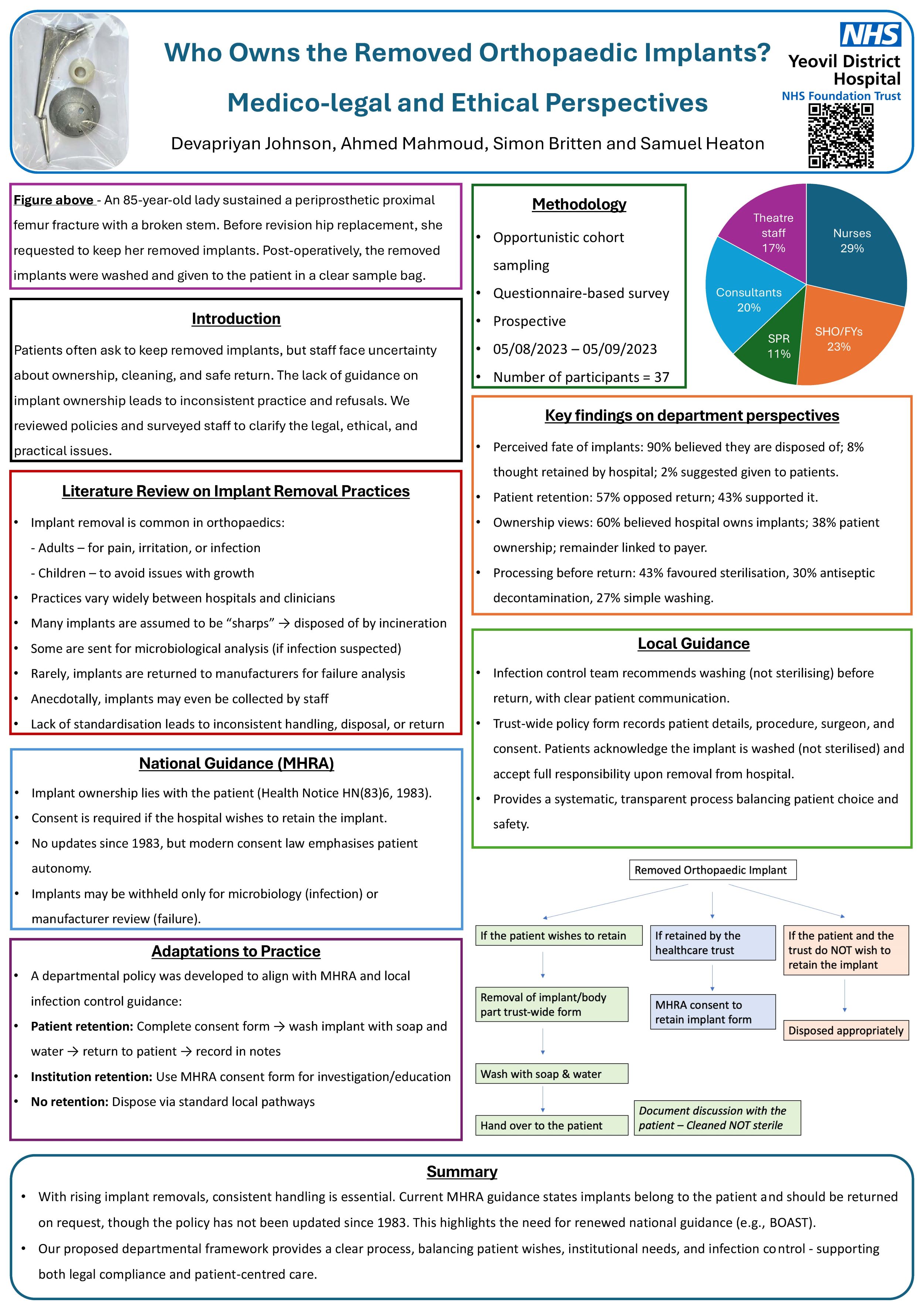
Devapriyan Johnson1, Ahmed Mahmoud1, Sam Heaton1, Simon Britten2
1Yeovil District Hospital, Yeovil, United Kingdom. 2LEEDS TEACHING HOSPITALS NHS TRUST, Leeds, United Kingdom
Background: Patients occasionally express a desire to retain implants. The guidelines regarding returning removed orthopaedic implants lack clarity, with varying practices among surgeons, highlighting the need for standardised guidance to enable legal compliance and patient satisfaction. To our knowledge, this is one of the first departmental studies to systematically assess and propose standardised implant return practices in line with Medicines and Healthcare Products Regulatory Agency (MHRA) guidance.
Methods: A questionnaire-based survey, elicited from 37 participants within an orthopaedic department, and consultation with the MHRA and local experts, informed the exploration of perspectives and development of recommendations for adaptations to practice.
Results: Survey findings revealed a broad range of beliefs and understanding regarding implant ownership and processing after removal. 90% believed implants were disposed of, 8% thought implants were retained by the health organisation, and 2% suggested that implants could be given back to the patient. Notably, 57% proposed that patients should not be allowed to keep the removed implants. National guidance from the MHRA indicates that the patient owns the implants. Local guidance emphasises pragmatic approaches — to wash removed implants and to return them to patients, balancing patient preferences and infection control measures.
Conclusion: Current practices often involve the disposal of removed implants, despite patients' rights to ownership. MHRA guidelines, unchanged since 1983, underscore the need for revisiting regulations to align with contemporary consent laws. Proposed adaptations offer a systematic approach, accommodating patient choices and clinical requirements. These proposed adaptations offer a replicable, patient-centred framework that could inform broader national policy and guideline updates.
Disclosure: The study was conducted within a single orthopaedic department and may not represent broader healthcare practices. Collaborative efforts with regulatory bodies and local experts informed these recommendations. Further research is warranted to assess the implementation and impact of proposed recommendations to practice.
407 - Implementation of High Flow Lists and Day Case Hip Arthroplasty at a Ring Fenced Barn Style Elective Orthopaedic Centre in the South East
Sanket Gandhi, Susan Jounus, Syed S. Ahmed
Maidstone & Tunbridge Wells NHS Trust, Royal Tunbridge Wells, United Kingdom
Background: Surgical backlogs continue to place significant pressure on the UK National Health Service (NHS). Innovative strategies such as High-Intensity Theatre lists—designed to maximise surgical throughput by reducing idle time are increasingly being adopted. Incorporating day case arthroplasty into these list models offers further gains in efficiency. This quality improvement project evaluated the impact of implementing HIT lists and day case hip arthroplasty at a single centre.
Methods: A phased implementation approach was adopted, targeting each stage of the patient journey. Pre-operative planning focused on thorough optimisation and strict patient selection. Theatre efficiency was enhanced through precise scheduling and staff coordination. Intra-operative processes aimed to minimise turnover times. Post-operative care protocols supported early mobilisation and safe same-day discharge. Continuous monitoring and refinement ensured ongoing optimisation.
Results: The introduction of HIT lists increased total hip arthroplasty throughput from 4 to 7 cases per day in a single operating theatre - a 40–50% improvement. Average turnaround time between cases reduced from 20–30 minutes to 10 minutes. Selected patients were safely discharged on the same day without any post-operative complications or readmissions. Staff reported high satisfaction levels with the streamlined workflow and team-based approach.
Conclusion/Findings: The implementation of high flow lists combined with day case hip arthroplasty significantly improved surgical efficiency, optimised theatre use, and enabled safe same-day discharge for appropriate patients. These outcomes demonstrate the feasibility and safety of this model in a high-volume NHS setting.
Implications: This approach offers a scalable solution to address elective surgery backlogs across NHS Trusts. Its success highlights the value of multidisciplinary coordination, meticulous planning, and patient-centred pathways in driving sustainable improvements in surgical services.
414 - Introducing DARFI: A National Collaborative Database for Researching Rare and Atypical Fractures and Injuries
Abdul-Rahman Gomaa1,2, Thomas Rogers3, Matthew Noonan3, Heather Rogers3, Lyndon Mason1,2
1Liverpool Orthopaedic & Trauma Service, Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom. 2School of Medicine, University of Liverpool, Liverpool, United Kingdom. 3Liverpool University Hospitals NHS Foundation Trust, Liverpool, United Kingdom
Background: The Database for Atypical and Rare Fractures and Injuries (DARFI) was established to address the challenges of researching uncommon musculoskeletal injuries across the UK. Conditions such as talus fractures and distal radioulnar joint (DRUJ) dislocations occur infrequently and are often underrepresented in clinical studies, leading to gaps in evidence-based practice. DARFI, approved by NHS Research Ethics Committee (REC), aims to enable national collaboration and structured data collection for these rare injuries.
Methods: DARFI was developed as a secure, ethically approved platform to support multicentre retrospective observational and interventional studies focused on rare and atypical injuries using routinely collected clinical data. The platform allows clinicians and researchers across NHS Trusts to create their own sub-studies as well as enrol and contribute anonymised data on eligible patients within existing studies. Standardised protocols and a unified governance framework ensure consistent data quality and regulatory compliance. The development of DARFI was guided by input from clinicians, research organisations, and ethics bodies.
Results: DARFI currently supports two active multicentre studies: one investigating clinical outcomes following talus fractures and another examining the diagnosis, management, and incidence of DRUJ dislocations. Almost 30 NHS sites have registered on the platform, with early recruitment numbers demonstrating strong clinical engagement and the practical feasibility of national data collection for rare injuries. DARFI has also fostered new collaborative networks between UK orthopaedic centres.
Conclusion: DARFI has proven to be an effective national platform for researching rare and atypical musculoskeletal injuries. Its NHS REC approval has ensured wide adoption and consistent ethical standards across participating sites.
Implications: DARFI represents a scalable and sustainable model for collaborative research into rare and atypical injuries. By enabling comprehensive data capture and facilitating multicentre studies, the platform supports the development of robust evidence body and enhances the UK’s research infrastructure in trauma and orthopaedics.
441 - Reducing the time taken to obtain urgent outpatient ultrasound scans for acute tendo-achilles and distal biceps ruptures
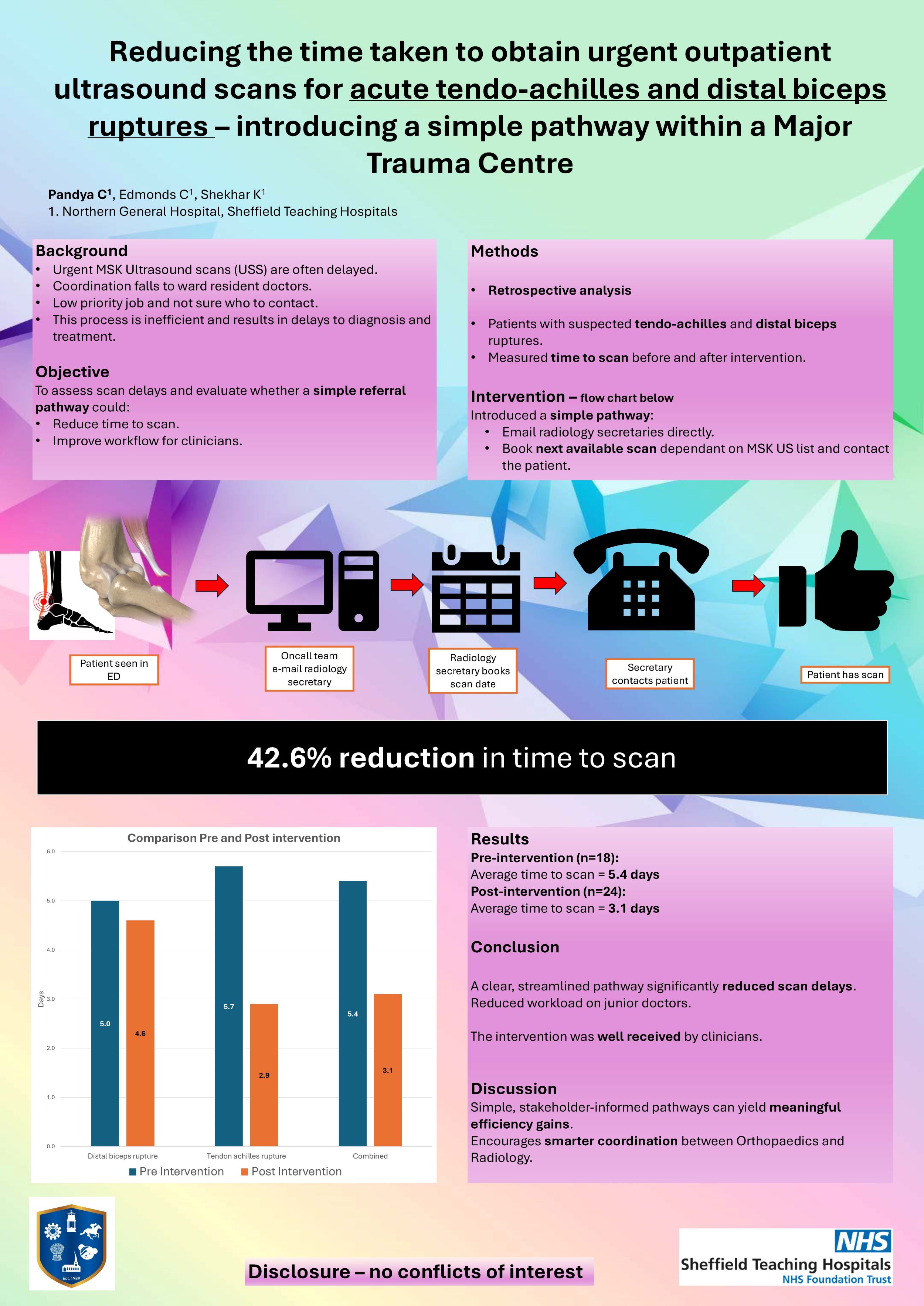
Chiraag Pandya, Callum Edmonds, Kumar Shekhar
Northern General Hospital, Sheffield Teaching Hospitals, Sheffield, United Kingdom
Background: Urgent outpatient Ultrasound scans (USS) for MSK pathologies can be difficult to organise in a timely fashion. The burden is often left to the junior resident doctor whose time spent phoning various members of the radiology department which is time consuming and an inefficient use of doctor time. The result is often a delay in scan.
We aim to assess how long it takes to obtain scans for tendo-achilles ruptures and distal biceps ruptures and whether a simple pathway actively involving our radiologists would improve this.
Methods: Retrospective analysis of time to obtain an urgent outpatient USS for acute tendo-achilles and distal bicep ruptures via Orthopaedic trauma lists. A simple pathway involving emailing the relevant radiology secretaries who could book the next appropriate scan appointment and contact the patient thereafter was implemented followed by re-evaluation of time taken to obtain scans.
Results: 18 patients’ data were analysed pre-intervention and 24 patients included in post-intervention analysis. Time taken to obtain scans decreased from an average of 5.4 days pre-intervention to 3.1 days post intervention.
Conclusion: Clear, easy to follow pathways do improved efficiency when obtaining scans. It was difficult to ascertain how much time was saved by junior resident doctors but given this pathway involves sending one email compared to multiple phone calls it is likely be more time efficient and anecdotally this pathway was well received.
Implications: Simple Pathways involving key stakeholders within the hospital is key to helping drive meaningful change.
Disclosure: No conflicts of interest
444 - Impact of an Enhanced Trauma Pathway on Orthopaedic Trauma Management: A Single-Centre Comparative Study
Sharo Naqar, Meera Sodha, Sarkhell Radha
Croydon University Hospital, London, United Kingdom
Background: Timely surgical intervention in orthopaedic trauma is critical for optimal recovery and patient outcomes. In 2021, Croydon University Hospital introduced an enhanced trauma pathway to streamline patient flow and expedite care. This study evaluates the impact of this pathway by comparing trauma data from 2019 (pre-implementation and early COVID period) with 2022 (post-implementation and post-COVID recovery).
Methods: We conducted a retrospective analysis of orthopaedic trauma cases, reviewing 1008 cases from 2019 and 1225 from 2022. Key metrics included:
· Time to surgical fixation
· Length of hospital stay
· Anaesthetic and positioning time
· Surgical time
· Fixation method
· Type of anaesthesia
· Re-operation/complication rate
· Inpatient mortality
Data were standardised and cleaned for anomalies. Statistical tests determined significance, with a focus on time to fixation and hospital stay as primary indicators of pathway effectiveness.
Results: There was a marked reduction in time to surgical fixation, from an average of 11 days in 2019 to 3 days in 2022. The average hospital stay also decreased slightly, from 10 to 9 days. Anaesthetic and positioning times increased minimally (37 to 38 minutes), while surgical time decreased (67 to 64 minutes). These results suggest improved efficiency in orthopaedic trauma care following pathway implementation.
Conclusion/Findings: The enhanced trauma pathway significantly reduced delays in surgical intervention and shortened hospital stays. These findings highlight the value of structured care pathways in optimising trauma care delivery.
Implications: Further analysis could help identify the specific components of the pathway contributing most to these improvements, informing future models for trauma care delivery across similar NHS trusts.
Disclosure: The authors declare no conflicts of interest.
465 - Optimising VTE Prophylaxis in Orthopaedic Inpatients A Quality Improvement Approach with HEPMA and AI
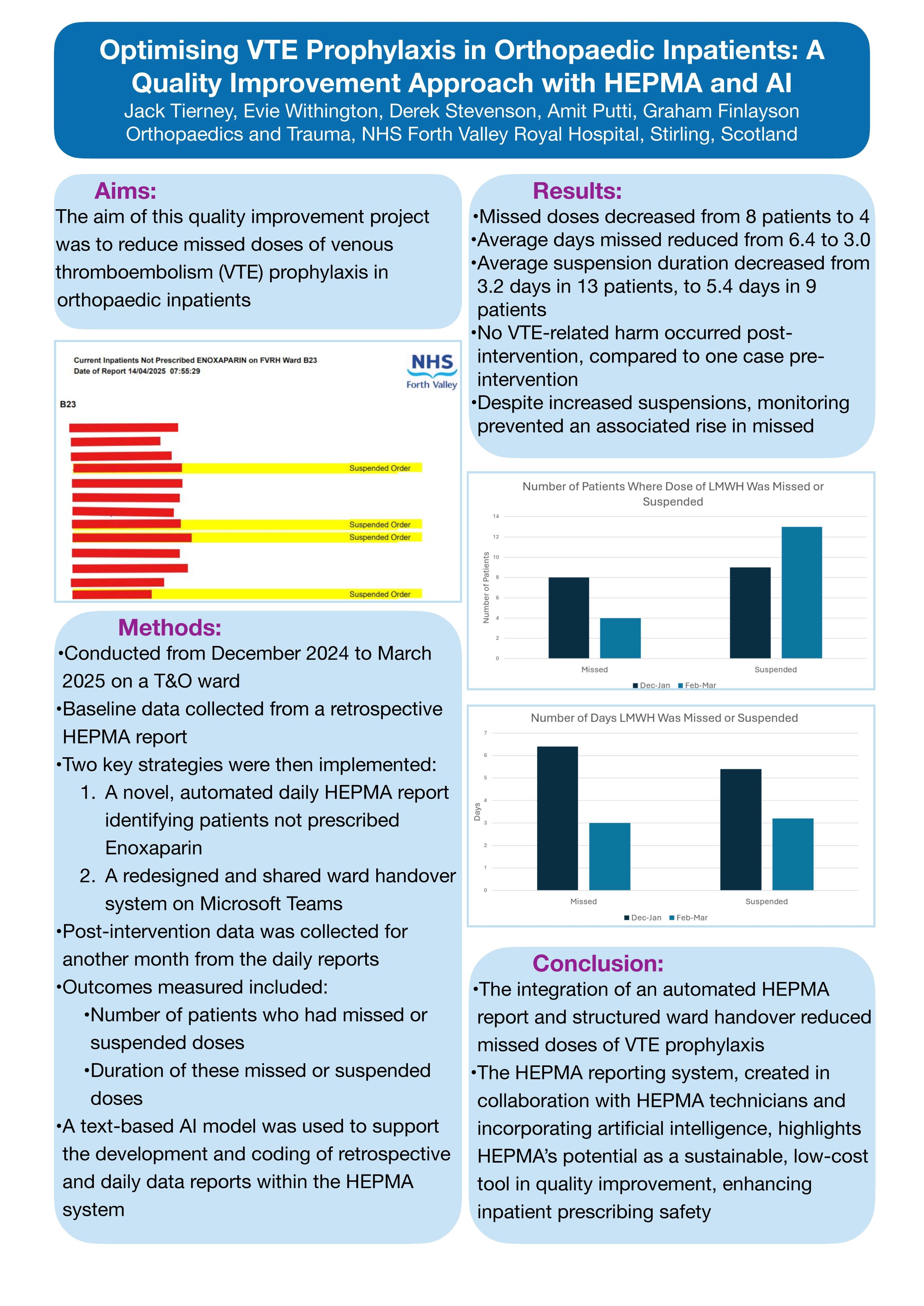
Jack Tierney, Evie Withington, Derek Stevenson, Amit Putti, Graham Finlayson
NHS Forth Valley, Stirling, United Kingdom
Aims: The aim of this quality improvement project was to reduce missed doses of venous thromboembolism (VTE) prophylaxis in orthopaedic inpatients.
Methods: Conducted from December 2024 to March 2025 on a trauma and orthopaedic ward, baseline data was collected retrospectively over one month from a HEPMA (Hospital Electronic Prescribing and Medicines Administration System) report on patients who either didn’t have enoxaparin prescribed, or had it suspended during their inpatient stay. Two key strategies were then implemented:
1. A novel, automated daily HEPMA report identifying patients not prescribed enoxaparin
2. A redesigned and shared ward handover system on Microsoft Teams.
Post-intervention data was collected for another month from the daily reports. Outcomes measured included the number of patients who had missed or suspended doses, as well as the duration of these missed or suspended doses. A text-based AI model was used to support the development and coding of retrospective and daily data reports within the HEPMA system.
Results: Following intervention, missed doses decreased from 8 patients to 4, with the average days missed reducing from 6.4 to 3.0. Additionally, more patients had VTE prophylaxis suspended post-intervention, with the average suspension duration decreasing from 3.2 days in 13 patients, to 5.4 days in 9 patients. Increased monitoring prevented an associated rise in missed doses. No VTE-related harm occurred post-intervention, compared to one case pre-intervention.
Conclusion: The integration of an automated HEPMA report and structured ward handover reduced missed doses of VTE prophylaxis. The HEPMA reporting system, created in collaboration with HEPMA technicians and incorporating artificial intelligence, highlights HEPMA’s potential as a sustainable, low-cost tool in quality improvement, enhancing inpatient prescribing safety.
844 - How good are we at asking if women are taking the combined oral contraceptive pill prior to elective surgery?
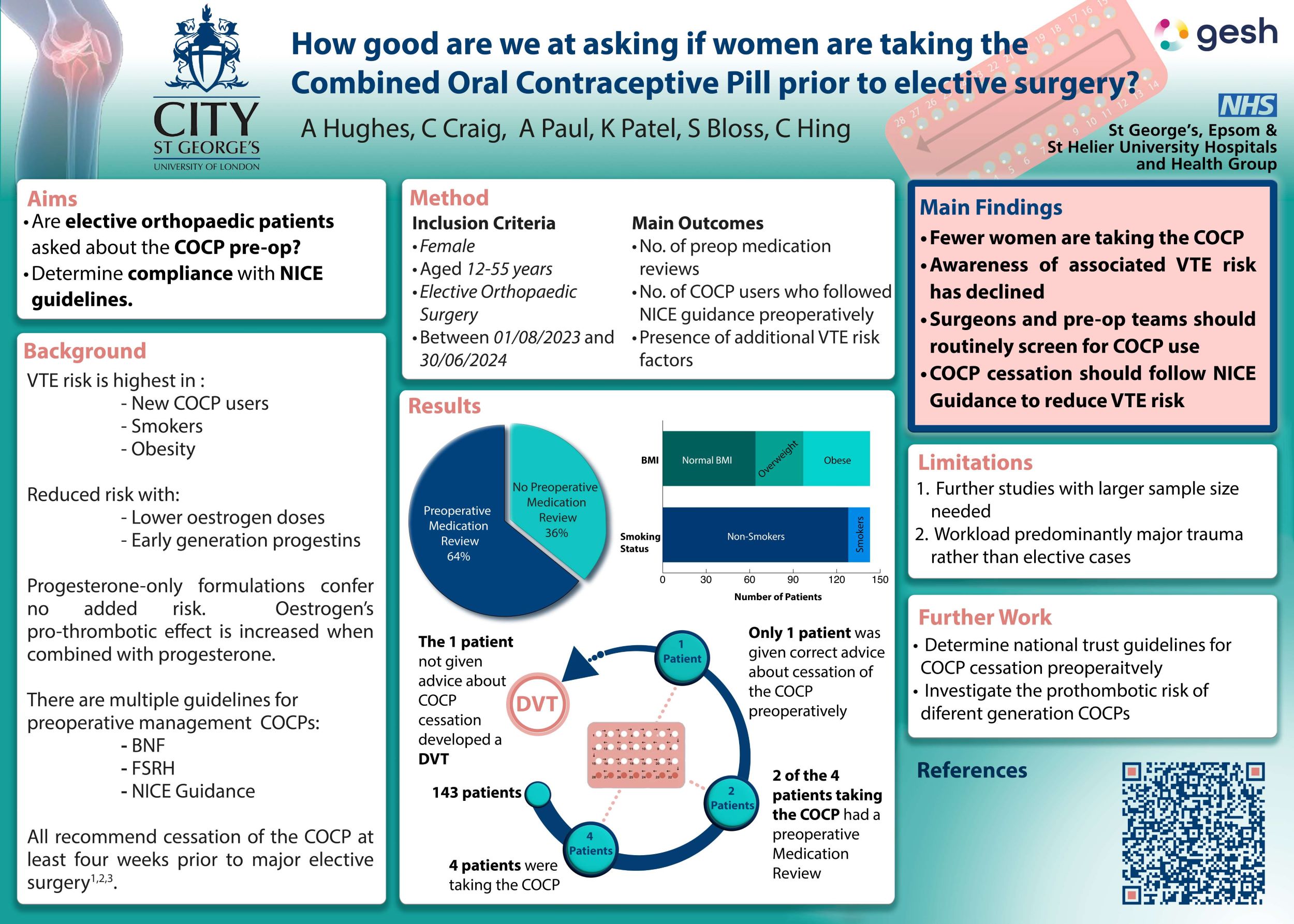
Callum Craig, Aimee Hughes, Krunal Patel, Ashita Paul, Samuel Bloss, Caroline Hing
St George's, London, United Kingdom
Introduction: NICE guidelines recommend suspending the combined oral contraceptive pill (COCP) at least four weeks before elective surgery due to the increased risk of venous thromboembolism (VTE). Concerns exist regarding adherence to this in elective orthopaedic surgery.
Methods: A retrospective audit was conducted of female patients aged 12–55 years who were admitted for elective orthopaedic surgery between 01/08/23 and 30/06/24. The audit assessed the rate of preoperative medication reviews and adherence to NICE guidelines for patients on the COCP.
Results: 243 patients met the inclusion criteria. 100 procedures were excluded as they were trauma cases or cancellations, leaving 143 procedures. Lower limb operations accounted for 64% of all operations and 77% were performed under general anaesthesia. Medication reviews were documented in 91 cases (64%). Four patients were taking the COCP, but only two had documented preoperative medication reviews. NICE guidelines were followed in one case. One patient who remained on the COCP, developed a postoperative deep vein thrombosis (DVT).
Discussion: This audit highlights that medication reviews concerning COCP use prior to elective orthopaedic surgery fail to adhere to NICE guidelines. Further work should be carried out to assess what guidelines trusts across the country are following and whether this aligns with NICE guidelines.
Declarations: The authors have no conflicts of interest.
859 - Robotic-assistance does not affect theatre productivity compared to manual hip and knee arthroplasty
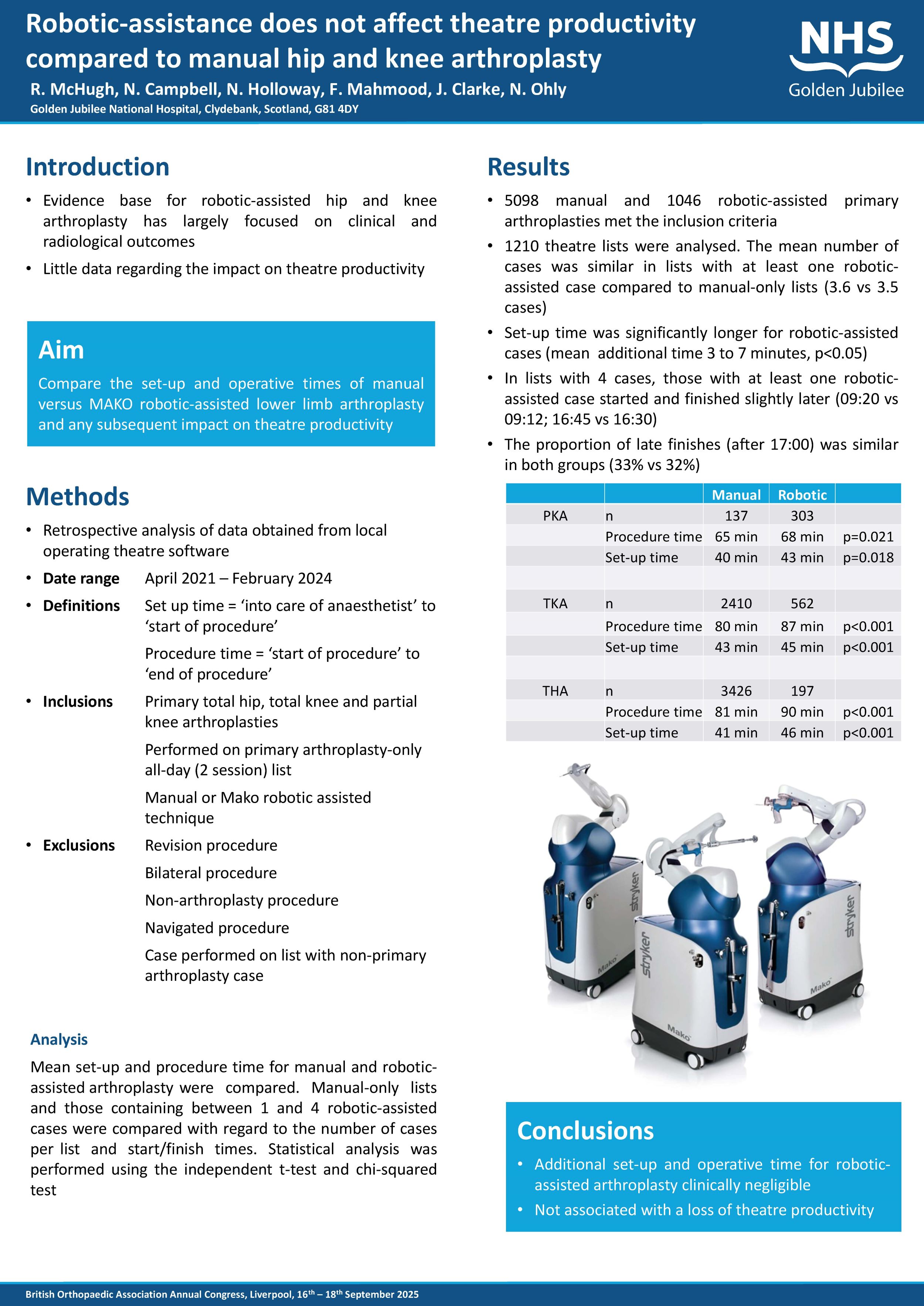
Rachel McHugh, Nathan Campbell, Nick Holloway, Fahd Mahmood, Jon Clarke, Nick Ohly
Golden Jubilee University National Hospital, Glasgow, United Kingdom
Background: The evidence base for robotic-assisted hip and knee arthroplasty continues to grow. However, existing studies have largely focused on clinical and radiological outcomes, with little data regarding the impact on theatre productivity. The aim of this study was to compare the set-up and operative times of manual versus MAKO robotic-assisted lower limb arthroplasty and any subsequent impact on theatre productivity.
Methods: This was a retrospective analysis of data obtained from local operating theatre software for primary arthroplasties performed on full day primary arthroplasty-only lists from April 2021 to February 2024. Mean set-up and procedure time for manual and robotic-assisted arthroplasty were compared. Manual-only lists and those containing 1 to 4 robotic-assisted cases were compared with regard to the number of cases per list and start/finish times. Statistical analysis was performed using the independent t-test and chi-squared test.
Results: 5098 manual and 1046 robotic-assisted primary arthroplasties were performed during the study period. The set-up time was significantly longer for robotic-assisted cases (mean additional time 3 to 7 minutes, p<0.05 ). The procedure time was longer for MAKO total hip (93 vs 81 minutes), MAKO total knee (88 vs 79 minutes) and MAKO partial knee arthroplasty (70 vs 67 minutes) (all p<0.05 ). 1210 theatre lists were analysed. The mean number of cases was similar in lists with at least one robotic-assisted case compared to manual-only lists (3.6 vs 3.5 cases). In lists with 4 cases, those with at least one robotic-assisted case started and finished slightly later (09:20 vs 09:12; 16:45 vs 16:30) and the proportion of late finishes (after 17:00) was similar in both groups (33% vs 32%).
Conclusion: We conclude that the additional set-up and operative time associated with robotic-assisted arthroplasty is clinically negligible, and was not associated with a loss of theatre productivity at our institution.
Shoulder & Elbow
394 - Early clinical and radiological outcomes of a stemless reverse shoulder arthroplasty system in patients over 75 years old
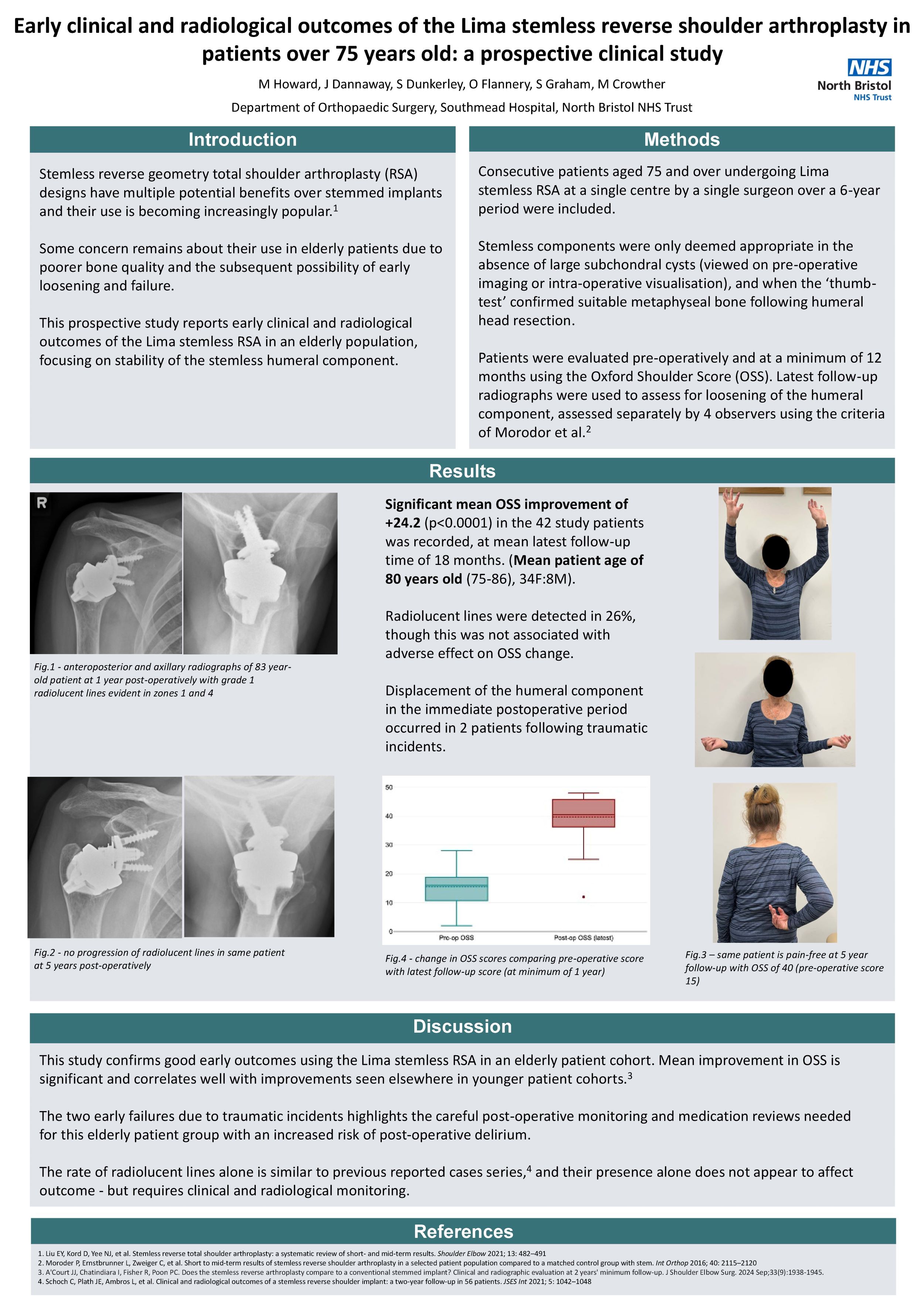
Matthew Howard, Jasan Dannaway, Sarah Dunkerley, Oliver Flannery, Selina Graham, Mark Crowther
Southmead Hospital, Bristol, United Kingdom
Background: Stemless reverse geometry total arthroplasty (RSA) designs have multiple potential benefits over stemmed implants and their use is becoming increasingly popular. Concern remains amongst sections of the wider shoulder arthroplasty community about the stability of stemless implants in elderly osteoporotic bone. This prospective study reports early clinical and radiological outcomes of the Lima stemless RSA in an elderly population, focusing on stability of the stemless humeral component.
Methods: Consecutive patients aged 75 and over undergoing Lima stemless RSA at a single centre by a single surgeon over a 6-year period were included. Patients were evaluated pre-operatively and at a minimum of 12 months using the Oxford Shoulder Score (OSS). Latest follow-up radiographs were used to assess for loosening of the humeral component using a recognised scoring system with multiple observers.
Results: Significant mean OSS improvement of +24.2 (p<0.0001) in the 42 study patients (mean age 80) was recorded, at mean latest follow-up time of 18 months. Radiolucent lines were detected in 27%, similar to previous studies looking at stemless arthroplasty - and this was not associated with adverse effect on OSS change. Displacement of the humeral component in the immediate postoperative period occurred in 2 patients following traumatic incidents.
Conclusion: This study confirms good early outcomes using the Lima stemless RSA in an elderly patient cohort. Stemless arthroplasty allows preservation of humeral bone stock and maximises future revision options if required - this study adds to the growing evidence base that it can be successfully used in appropriate elderly patients. The presence of radiolucent lines alone does not appear to affect outcome, but requires clinical and radiological monitoring.
Implications: The expectation is that the use of stemless implants will continue to grow, and ongoing follow-up of these patients will help to confirm that positive outcomes are maintained with time.
Disclosures: None
Spine
249 - Risk factors analysis of thoracolumbar vertebrae refracture after PKP in elder patients with osteoporotic compression fracture
Yi Zhang
Traditional Chinese Medicine Hospital, TongLiang, ChongQing, Chongqing, China
Objective: To investigate the risk factors of postoperative vertebral body refracture after percutaneous kyphoplasty (PKP) in the treatment of thoracolumbar osteoporotic compression fracture.
Method: The radiological and clinical data of 862 patients who underwent single-level PKP surgery for thoracolumbar vertebral compression fracture in our hospital from January 1, 2018 to December 31, 2022 were retrospectively analyzed. Gender, age, body mass index (BMI), bone mineral density(BMD), surgical approach, injection amount of cement, diffusion state, leakage, vertebral height restores, kyphotic angle reduction, wedge angle reduction of vertebral body, postoperative anti-osteoporosis drug application, etc. were collected and analyzed by univariate and multivariate analysis.
Results: A total of 475 patients were included in this study, with an average age of 72.16±6.38 years old. The incidence of refracture was 3.71% in 32 patients. Univariate analysis showed that intravertebral cleft sign, endplate cortical disruption, small injection amount of bone cement, and non-contact between bone cement and endplate were risk factors for vertebral refracture after PKP. Multivariate analysis of these factors showed that large injection amount of bone cement was a protective factor, and preoperative endplate cortical disruption, preoperative intravertebral cleft sign, and poor contact between bone cement and endplate were independent risk factors for vertebral refracture after PKP.
Conclusions: It was found that small injection amount of bone cement, endplate cortical disruption, intravertebral cleft sign, and poor contact between bone cement and endplate were independent risk factors for postoperative refracture after PKP treatment of osteoporotic compression fractures in the elderly thoracolumbar spine.
Trauma
271 - Assessing the Effectiveness of Antibiotic Irrigation to Reduce Bacterial Load at the Spinal Surgical Site: An In-Vitro Study
Rawan Masarwa1, Ofir Uri1, Abed Athamna1, Sarit Freimann1, Ali Yassin1, Elie Najjar1, Rodrigo Muscogliati1, Weronika Nocun1,2, Eyal Behrbalk1
1Centre for Spinal Studies and Surgery, Queen's Medical Centre, Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom. 2 3) School of Medicine, University of Nottingham, Nottingham, United Kingdom
Introduction: Intra-operative surgical site irrigation with antibiotics is believed to reduce the risk of infection in spine surgeries involving instrumentation. However, despite its frequent use, there is limited supporting evidence for this practice. This prospective in-vitro study aims to evaluate the effect of short-term antibiotic exposure on the growth of common pathogens associated with wound infections.
Methods: A suspension of one of three micro-organisms: (1) Staphylococcus aureus, (2) Staphylococcus epidermidis, or (3) Pseudomonas aeruginosa was added to 2-ml vials of an enriched medium, containing one of three antibiotics: (a) Vancomycin, (b) Gentamicin, or (c) Cefazolin. The final inoculum of each micro-organism was 103 CFU/ml, representing a contaminated surgical wound in spine surgery. Antibiotics were washed out from the suspension by a centrifugation technique after (i) 5 minutes, or (ii) 8 hours. The recovery of growth of the micro-organisms was monitored by laser light scattering technology.
Results: P. aeruginosa inoculated in vials with Gentamicin showed no 24-hour bacterial growth after 5-minute and 8-hour exposure to the antibiotic. Vials of all other bacteria-antibiotic combinations showed bacterial growth curves similar to the control vials after both 5-minute and 8-hour exposures to antibiotics, with no signs of bacterial growth inhibition.
Conclusion: The study demonstrated that Gentamicin effectively inhibited P. aeruginosa growth after both short-term (5-minute) and long-term (8-hour) exposures. However, no significant bacterial growth inhibition was observed with other bacteria-antibiotic combinations, regardless of the exposure time. These findings suggest that while Gentamicin may be effective against P. aeruginosa in the context of surgical site irrigation, the use of Vancomycin and Cefazolin does not appear to provide the same level of effectiveness for the other tested pathogens. Further studies are needed to evaluate alternative antibiotic strategies for broader infection control in spine surgeries.
289 - Factors influencing implant failure in cephalomedullary nails for proximal femoral fractures a retrospective review
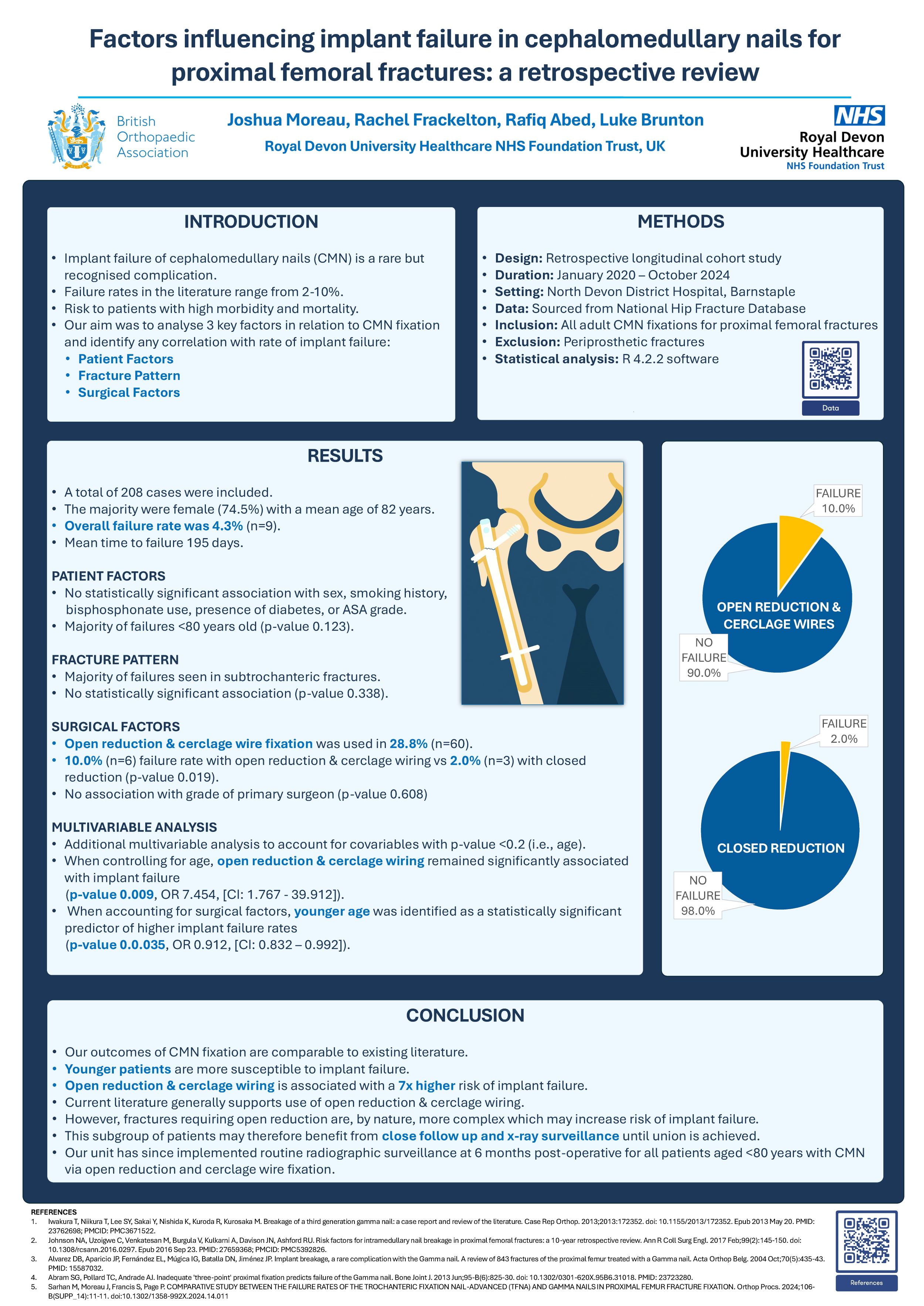
Joshua Moreau, Rachel Frackelton, Rafiq Abed, Luke Brunton
North Devon District Hospital, Barnstaple, United Kingdom
Background: Treatment of extracapsular hip fractures with cephalomedullary nailing (CMN) is a well-established fixation method. Although rare, implant failure is a recognised complication which poses risk to patients who are already burdened with high morbidity and mortality. The purpose of this study is to review the outcomes of CMN fixations for proximal femoral fractures, with particular focus on implant failure. We analysed patient demographics, surgical factors, and fracture pattern to ascertain correlation with rate of implant failure.
Methods: This was a retrospective longitudinal cohort study of CMN fixations at a district general hospital between January 2020 and October 2024. All adult proximal femoral fractures treated with long CMN were included. Data collection was obtained from clinical records and relevant imaging. Multivariable logistic regression modelling was performed to analyse results.
Results: Long CMN was performed in 208 cases. The majority were female (74.5%) with a mean age 82 years. Open reduction and cerclage wiring occurred in 28.8% of cases (n=60). An overall failure rate of 4.3% (n=9) was identified. There was a statistically significant association between patient age and implant failure, with younger patients more likely to experience this complication (p-value 0.035). Similarly, open reduction and cerclage wire augmentation was associated with higher rates of implant failure (10.0% vs 2.0%, p-value 0.009) when compared to closed reduction.
Conclusion: The findings suggest that our outcomes of CMN fixation are comparable to existing literature. However, we have identified that patients treated with open reduction and cerclage wiring have a 7 times higher risk of implant failure. This subgroup of patients may benefit from close follow up and x-ray surveillance until union is achieved. Our unit has now implemented routine radiographic surveillance at 6 months post-operative for all patients below the age of 80 treated with CMN via open reduction and cerclage wire fixation.
339 - Predictors of Non-Union in Humeral Shaft Fractures A Retrospective Cohort Study
Zaid Hashim1, Michael Flatman2, Priya Parekh2, David Hawkes2
1Chesterfield Royal Hospital, Chesterfield, United Kingdom. 2Arrowe Park Hospital, Wirral, United Kingdom
Introduction: Humeral shaft fractures represent 3-5% of all fractures, yet there remains limited consensus regarding their definitive management. This study aimed to identify predictors of non-union in conservatively managed HSFs and to compare complication rates between conservative and operative treatment approaches.
Methods: A retrospective, single-centre cohort study was conducted from January 2014 to September 2023. Conservative management included bracing, casting, or collar and cuff, while operative management involved open reduction and internal fixation or intramedullary nailing. Exclusion criteria were pathological fractures, open fractures, skeletal immaturity, inadequate imaging, and loss to follow-up. Fracture healing was assessed using the Radiographic Humeral Union Measurement (RHUM) at 6 and 12 weeks. Logistic regression was used to identify independent risk factors for non-union.
Results: Among 149 patients (76 conservative, 73 operative), the non-union rate was 14.5% in the conservative group and 0% in the operative group. Smoking (odds ratio [OR]: 7.7, p=0.038) and RHUM <6 at six weeks (OR: 8.1, p = 0.029) were identified as significant predictors of non-union. Diabetes was not a significant predictor (p = 0.659). Reported complications included skin irritation in 2.6% of the conservative cohort and radial nerve palsy in 4.1% of the operative group.
Conclusion & Implications: The threshold for surgical management might be lower for patients who smoke; certainly, the results highlight the importance of smoking cessation advice. Further, surgical intervention may be considered in patients who have a RHUM score of less than 6 at 6 weeks post-injury. However, patients would need to be counselled against the risk of radial nerve palsy with operative intervention.
350 - Surgical management of scapula fractures - an MTC experience
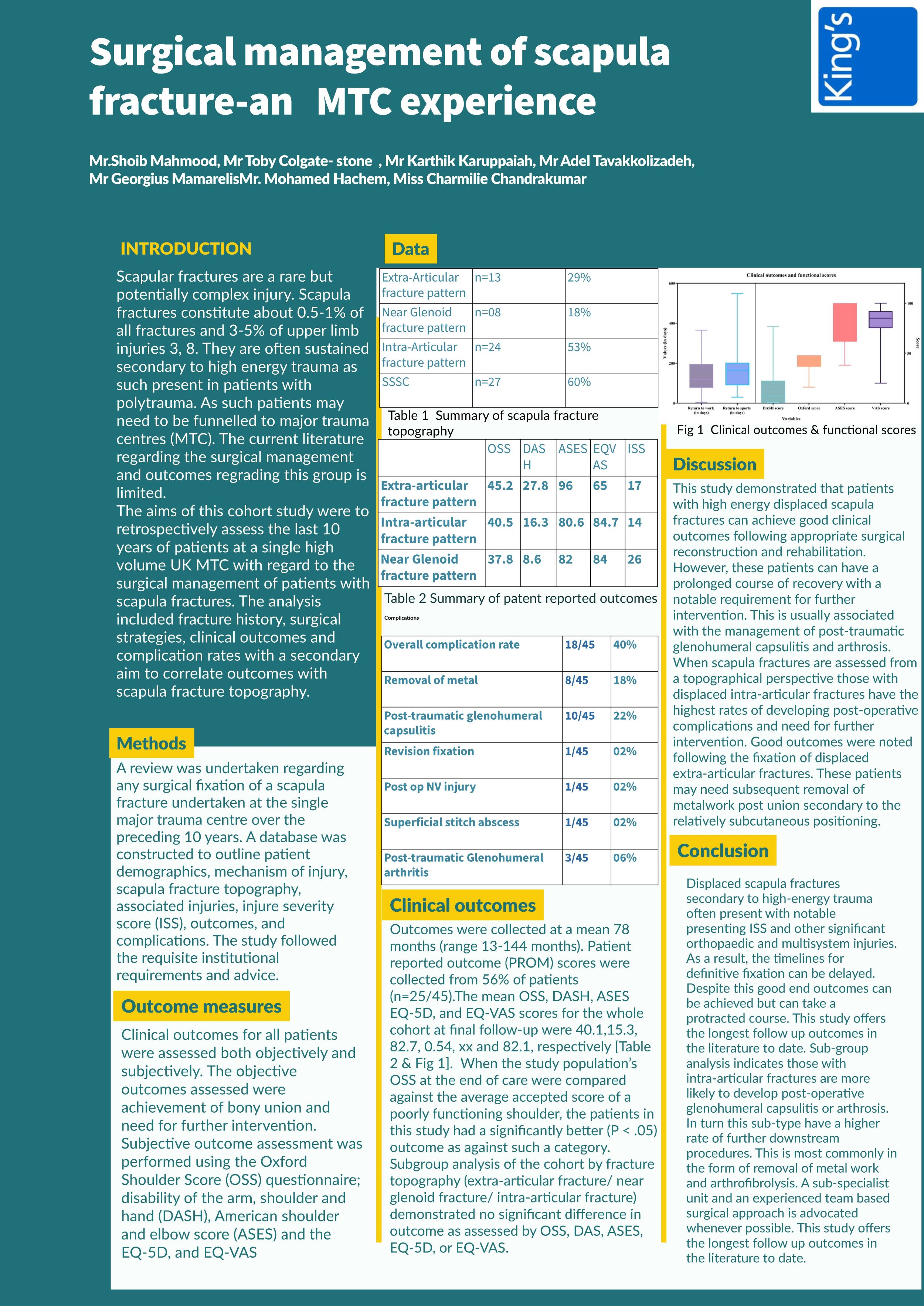
Shoib Mahmood1, Toby Colgate-Stone1, Karthik Karuppaiah1, Adel Tavallizadeh1, Georgios Mamrelis1, Mohamad Hachem1, Charmili Chandrakumar2
1Kings College Hospital, London, United Kingdom. 2Lewisham & Greenwich NHS trust, London, United Kingdom
Background: Scapula fractures requiring surgical management are an infrequent but complex high energy injury. Aims of this cohort study were to review the surgical strategies, outcomes and complication rates noted in such patients.
Methods: Patients (n=45) with displaced scapula fractures undergoing surgery over a 12-year period were analysed. Orthopaedic characteristics of injury were assessed as well as other associated injuries. Outcomes were reviewed subjectively (OSS, DASH, ASES and EQ-VAS and objectively (achievement of bony union range of movement, infection status, reoperation).
Results: The majority of the injuries (63%) involved a displaced glenoid fracture pattern. Associated Orthopaedic injuries were present in 40% cases and associated system injuries in 53%. Clinical and functional outcomes were noted to be positive. The mean OSS, DASH, ASES and EQ-VAS for the whole cohort at final follow-up were 40.1(16-48), 15.3(0-76.8), 82.7(38-100) and 82.1(20-100) respectively. Mean return to work was 147.5(4-365) days and return to sports was 185.6(30-548) days. Sub-group analysis of the cohort by fracture topography (intra-articular glenoid versus extra-articular) demonstrated difference regarding final OSS, DASH, ASES and EQVAS. Complete bony union was noted in 97.9% of patients. The overall complication rate was 15.6% (n=7/45; n=1 neuropraxia; n=1 infection; n=1 failure of fixation; n=4 arthrolysis). Subsequent removal of metalwork in 24.4%(n=11/45).
Conclusion: Displaced scapula fractures secondary to high-energy trauma often present with notable presenting ISS and other significant orthopaedic and multisystem injuries. As a result, the timelines for surgery are often delayed. Despite this good end outcomes can be achieved but can take a protracted course. Sub-group analysis indicates intra-articular fractures have worse outcomes and further procedures are often indicated. This is most commonly in the form of removal of metal work and arthrofibrolysis. A sub-specialist unit and experienced surgical approach is advocated whenever possible.
Disclosure: Nothing to declare
421 - A prospective cohort study of surgical outcomes following hip fracture in Zimbabwe
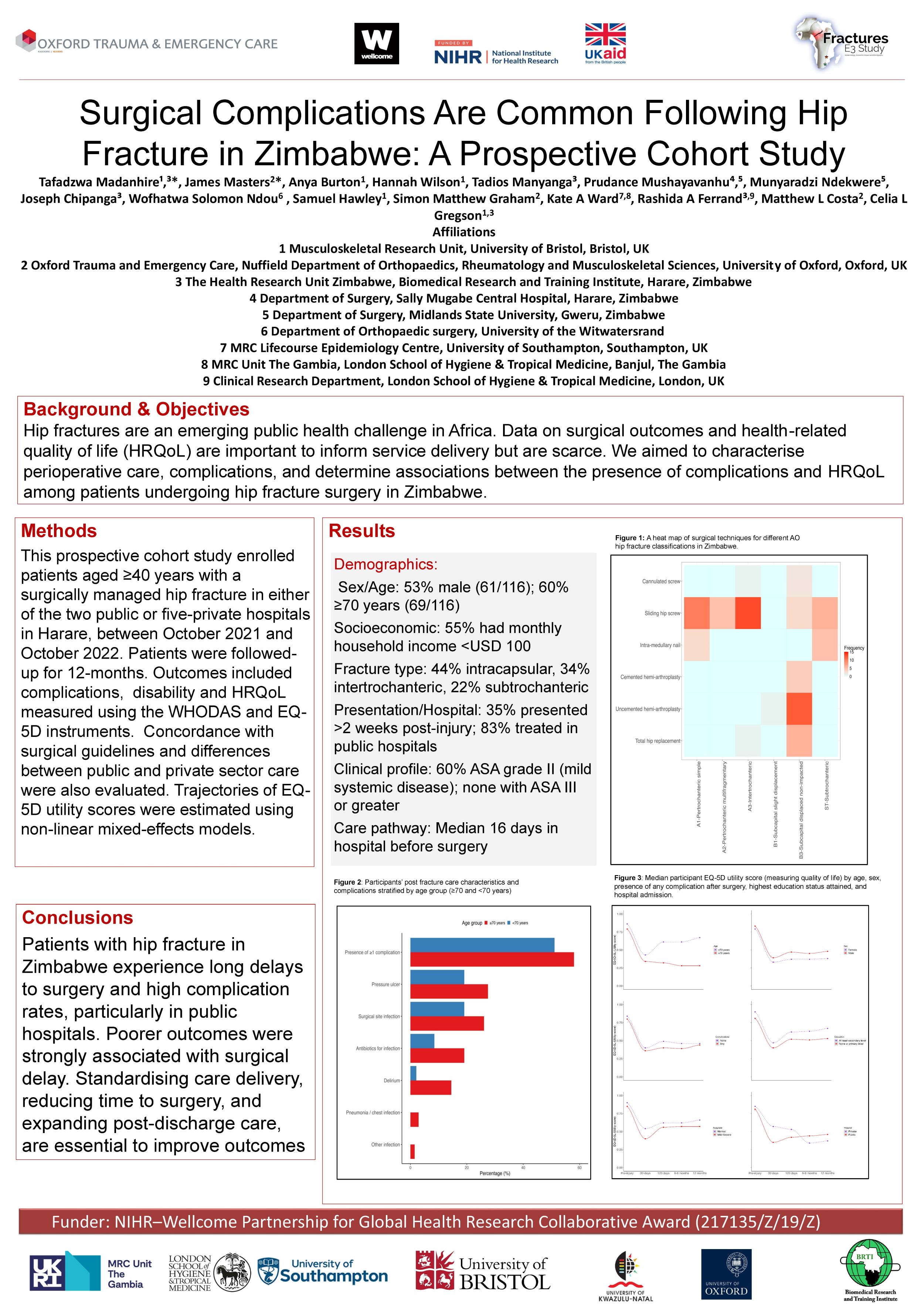
James Masters1, Tafadzwa Madanhire2, Anya Burton2, Hannah Wilson2, Tadios Manyanga3, Prudance Mushayavanhu4,5, Munyaradzi Ndekwere4, Kate Ward6, Rashida Ferrand7,3, Simon Graham1, Matthew Costa1, Celia Gregson2
1Oxford University, Oxford, United Kingdom. 2Bristol University, Bristol, United Kingdom. 3THRU Zim/BRTI, Harare, Zimbabwe. 4Sally Mugabe Central Hospital, Harare, Zimbabwe. 5Midlands State University, Gweru, Zimbabwe. 6Southampton University, Southampton, United Kingdom. 7London School of Hygiene and Tropical Medicine, London, United Kingdom
Aims: Hip fractures are an emerging public health challenge in sub-Saharan Africa. However, data describing surgical outcomes and health-related quality of life (HRQoL) in this setting are scarce. We aimed to characterise perioperative care, complications, and long-term outcomes among patients undergoing surgery for hip fracture in Zimbabwe.
Methods: This prospective cohort study enrolled patients aged ≥40 years with a surgically managed hip fracture in Harare between October 2021 and October 2022. Patients were followed for 12 months. Outcomes included surgical complications, disability, and HRQoL measured using the WHODAS and EQ-5D-5L instruments. Surgical concordance with international guidelines and differences between public and private sector care were also evaluated.
Results: Of 116 patients, 59.5% were aged ≥70 years, most (82.8%) were treated in public hospitals. Median time from injury to surgery was 25 days (IQR 10–45) including a median of 16 days (8-27) between admission and surgery. Postoperative stays were short (median 3 days). Over half (55.2%) experienced at least one complication, most commonly pressure ulcers (24.1%), surgical site infection (22.9%) and delirium (9.5%). Complications were associated with delayed surgery, prolonged admission, and female sex. Patients with complications reported lower HRQoL throughout follow-up. While private sector patients initially (at 30-days) showed better HRQoL and lower disability, by 12-months outcomes were worse than in public sector patients. Guideline-discordant surgery was not independently associated with poorer recovery.
Conclusion: Hip fracture patients in Zimbabwe experience high complication rates and long delays to surgery, particularly in the public sector. Although private care offered early postoperative advantages, these did not persist at 12 months. Poorer outcomes were strongly associated with surgical delay. Restructuring of the care pathway to standardise care, reduce time to surgery and expand post-discharge care are essential to improve recovery and equity in this setting.
446 - Safe calcaneal pin placement – review of a reproducible technique using anatomical landmarks without radiological guidance
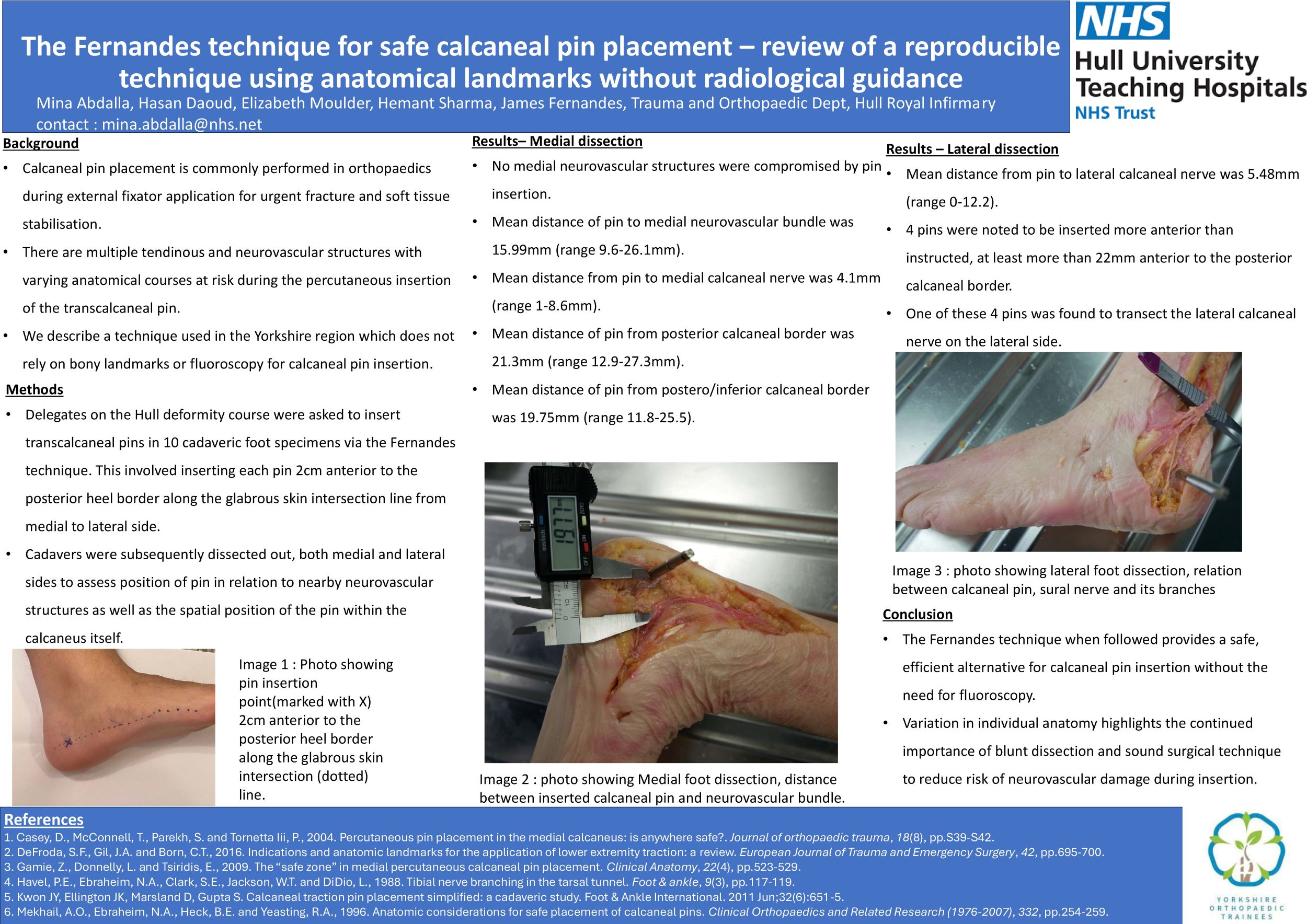
Mina Abdalla, Hasan Daoud, Elizabeth Moulder, Hemant Sharma
Hull Royal Infirmary, Hull, United Kingdom
Background: Calcaneal pin placement is commonly performed in orthopaedics during external fixator application for urgent fracture and soft tissue stabilisation. There are multiple tendinous and neurovascular structures with varying anatomical courses at risk during the percutaneous insertion of the transcalcaneal pin. We describe a technique used in the Yorkshire region which does not rely on bony landmarks or fluoroscopy for calcaneal pin insertion.
Methods: Delegates on the Hull deformity course were asked to insert transcalcaneal pins in 10 cadaveric foot specimens via the specific Yorkshire technique. This involved inserting each pin 2cm anterior to the posterior heel border along the glabrous skin intersection line from medial to lateral. Cadavers were subsequently dissected out, both medial and lateral sides to assess position of pin in relation to nearby neurovascular structures as well as the spatial position of the pin within the calcaneus itself.
Results: Mean distance of pin from posterior calcaneal border was 21.3mm (range 12.9-27.3mm). Mean distance of pin from postero/inferior calcaneal border was 19.75mm (range 11.8-25.5). Mean distance of pin to medial neurovascular bundle was 15.99mm (range 9.6-26.1mm). Mean distance from pin to medial calcaneal nerve was 4.1mm (range 1-8.6mm). No medial neurovascular structures were compromised by pin insertion. Mean distance from pin to lateral calcaneal nerve was 5.48mm (range 0-12.2). 4 pins were noted to be inserted more anterior than instructed, at least more than 22mm anterior to the posterior calcaneal border. One of these 4 pins was found to transect the lateral calcaneal nerve on the lateral side.
Conclusion: The Yorkshire technique when followed provides a safe, efficient alternative for calcaneal pin insertion without the need for fluoroscopy. Variation in individual anatomy highlights the continued importance of blunt dissection and sound surgical technique to reduce risk of neurovascular damage during insertion.
Disclosure: No disclosures to declare.
449 - A review of Outcomes of Distal Femoral Replacement for Trauma in a medium sized District General Hospital
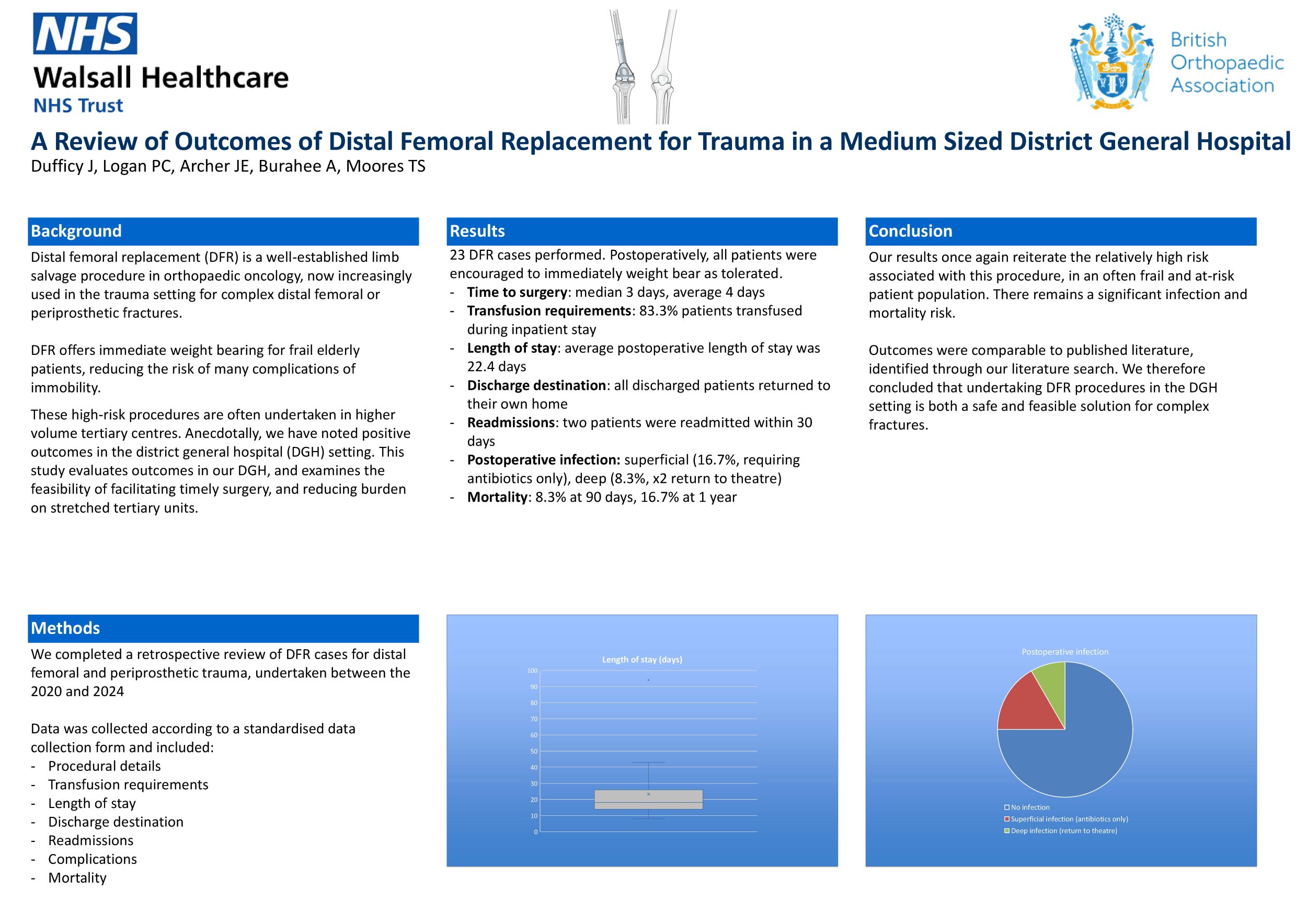
Peter Clark Logan, Jack Dufficy, James Edward Archer, Thomas Steven Moores
Walsall Healthcare NHS Trust, Walsall, United Kingdom
Background: Distal femoral replacement (DFR) is a well-established limb salvage procedure utilised in orthopaedic oncology. The indications have now expanded to include management of complex distal femoral or peri-prosthetic fractures. This procedure offers an opportunity for immediate weight bearing, reducing the risk of complications associated with immobility in this often frail and elderly patient cohort.
The primary objective of this study is to evaluate the outcomes of distal femoral replacement procedures performed for trauma in our district general hospital.
Methods: A retrospective review of patient records was conducted, encompassing distal femoral replacements performed for distal femoral fractures and periprosthetic fractures between 2020 and 2024. We have collected procedural data, hospital length of stay, discharge destination, readmissions, management of complications, and mortality.
Results: 23 cases of DFR were performed, all patients were allowed to weight bear as tolerated immediately, and all discharged patients returned to their own home. The average postoperative length of stay was 22.6 days. Of those who were discharged home, there were two 30-day readmissions. Two cases were complicated by postoperative deep infection (8.7%) and required further surgical intervention (DAIR & revision respectively). Four cases of superficial infection were identified which required antibiotics only (17.4%). There were two deaths within 90 days from operation (8.7%), and four (17.4%) within one year.
Conclusion: Distal femoral replacement performed in district general hospitals is an effective surgical solution for these complex fractures. We have been able to demonstrate the restoration of mobility in these patients, with outcomes comparable to those published in the tertiary centre setting. In the context of increasing incidence of distal femoral fragility fractures, and periprosthetic distal femoral fractures, management of selected cases locally may allow for prompt management by surgeons with appropriate skill sets and ease the burden on tertiary units.
Disclosures: The authors have no disclosures.
537 - Head, Shoulders, Knees and Toes - Missed Lower Limb Injuries in Major Trauma
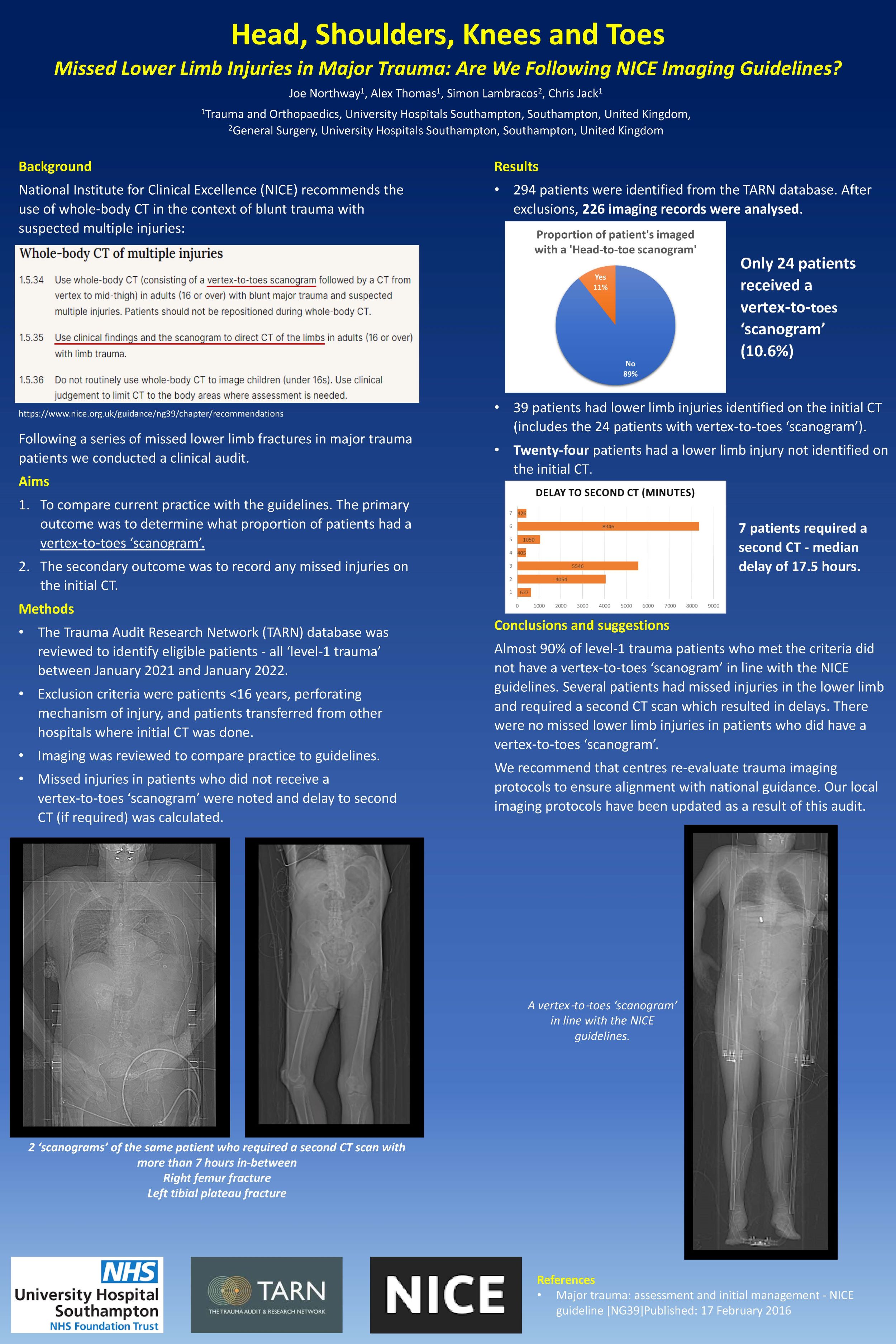
Joseph Northway1, Alexander Thomas2, Chris Jack2
1NUH, Nottingham, United Kingdom. 2UHS, Southampton, United Kingdom
Background: NICE recommends the use of whole-body CT in the context of blunt trauma with suspected multiple injuries. This should comprise of a vertex-to-toes scanogram followed by CT from head to mid-thigh. Clinical findings and scanogram results should guide further limb imaging. This study evaluated real-world compliance with these recommendations and their impact on the timely detection of injuries.
Methods: ‘Level-1 trauma’ patients were retrospectively identified from the TARN database between January 2021 and January 2022. Patients under 16 years old, with penetrating injuries, or transferred from other hospitals after initial imaging, were excluded. Imaging studies were reviewed for adherence to NICE guidance. Missed lower limb injuries and delays to secondary imaging were recorded.
Results: Of 294 cases, 226 met inclusion criteria. Only 24 patients (10.6%) received a vertex-to-toes scanogram. Twelve patients had CT scans that did not extend to the mid-thigh. Lower limb injuries were identified in 39 patients on initial imaging, 24 of whom had received the recommended scanogram. Among those without complete scanogram (n=202), 24 had undetected lower limb injuries, with 7 requiring further CT (median delay 17.5 hrs; maximum 139.1 hrs). Notably, no missed lower limb injuries occurred in patients who had undergone a complete vertex-to-toes scanogram.
Conclusions and Suggestions: Almost 90% of level-1 trauma patients were not imaged in line with NICE guidance, resulting in 24 missed lower limb injuries and diagnostic delays. No missed injuries occurred in patients who received a vertex-to-toes scanogram, highlighting its role in early and complete injury detection. These findings reinforce the importance of using scanograms to prevent harm through timely diagnosis and appropriate imaging. We recommend that centres re-evaluate trauma imaging protocols to ensure alignment with national guidance. To our knowledge, this is the first UK audit to assess real-world compliance with NICE trauma imaging standards in this way.
724 - Does early surgery reduce complications following closed ankle fractures? A retrospective cohort study
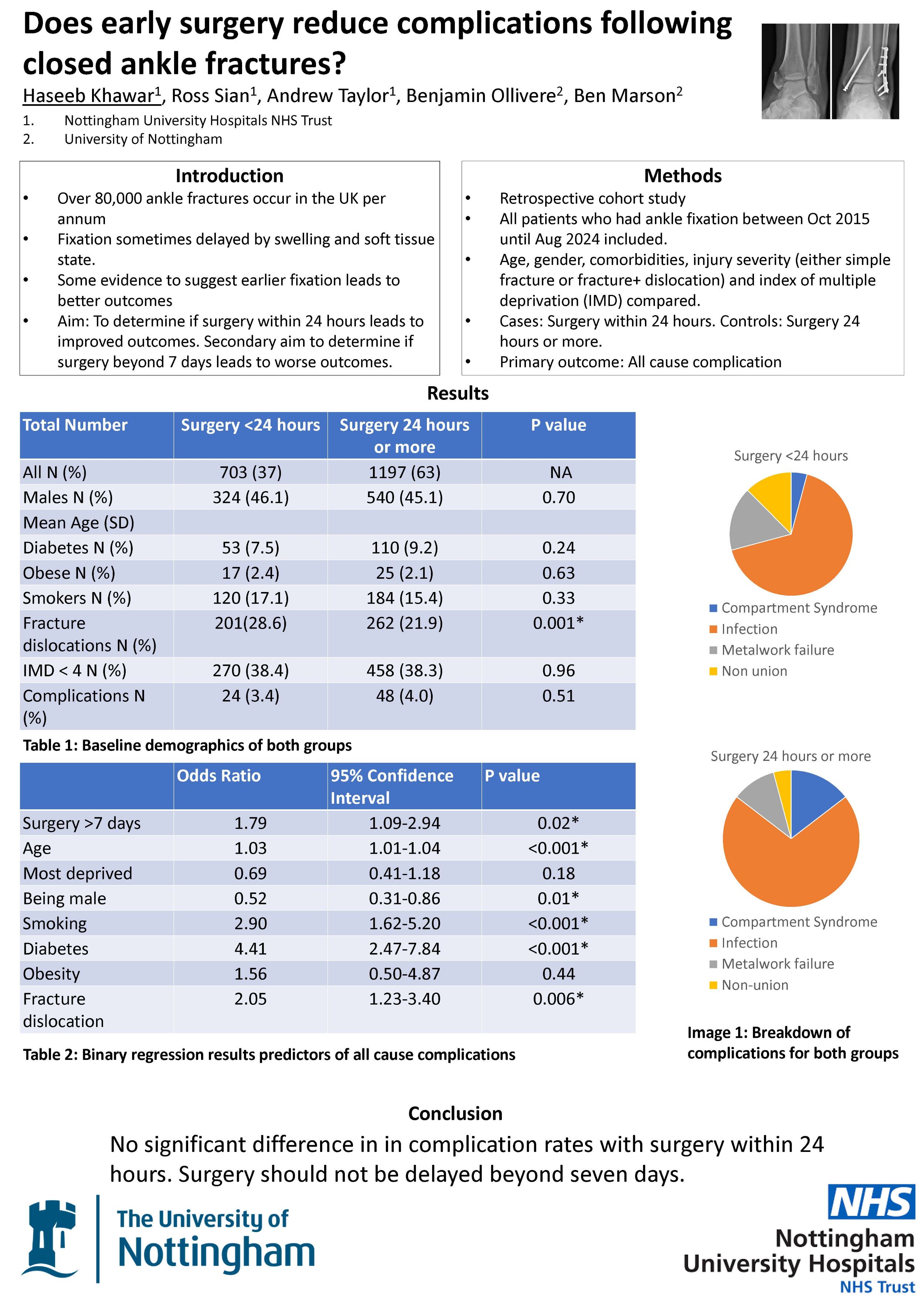
Haseeb Khawar1, Ross Sian2, Andrew Taylor1, Benjamin Ollivere1,3, Ben Marson1,3
1Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom. 2University Hospitals of Derby and Burton NHS Trust, Derby, United Kingdom. 3University of Nottingham, Nottingham, United Kingdom
Background: There is body of opinion that performing surgery for closed ankle fractures within the first 24 hours of injury may improve patient outcomes and reduce delays due to swelling. The aim of our study was to evaluate if fixation within 24 hours of injury is associated with improved all cause complication rate (including non-union, metalwork failure and infection). Secondary aim of our study was to determine if surgery beyond one week increases complication risk.
Methods: A retrospective study of 1,900 patients who had operative fixation for their closed ankle fracture between October 2015 and August 2024 was conducted. Age, gender, diabetes/smoking/obesity, severity of injury (either simple fracture or fracture dislocation) and indices of multiple deprivation (IMD) were compared for patients who had surgery within 24 hours (cases) versus those who had surgery after 24 hours (controls). The primary outcome was the rate of all cause complication. Two-tailed T test and Chi squared tests were performed to compare group metrics. Binomial regression analysis was performed to establish significant predictors of infection. P value <0.05 was considered statistically significant.
Results: 703 (37.0%) patients received surgery within 24 hours. There was no significant difference in age, gender, smoking/alcohol/obesity, diabetes status or deprivation between groups. 28.6% of cases had a more severe injury pattern vs 21.9% of controls (P<0.001). Complication rates were 3.4% in cases and 4.0% in controls (P=0.51). 623 (32.8%) had surgery after seven days. Regression analysis showed that surgery after seven days was predictive of complications (OR 1.79, 95% CI 1.09-2.94) after controlling for all other risk factors.
Conclusion: This study demonstrated no significant difference in the rate of complications in patients undergoing ankle fracture surgery within 24 hours of injury. Soft tissues should be allowed to settle. Surgery should not be delayed beyond seven days.
739 - A systematic review and meta-analysis of syndesmotic stability in posterior malleolar fractures
Siyoung Lee, Le Tien, Toby Jennison
University Hospitals Plymouth, Plymouth, United Kingdom
Introduction: Posterior malleolar fractures encompass a wide range of classifications, fracture configurations, and treatment techniques. It remains unclear whether the syndesmosis requires additional stabilisation when the posterior malleolus is treated surgically. The aim of this systematic review and meta-analysis was to determine whether syndesmotic instability—and thus the need for fixation—was influenced by the surgical treatment of the posterior malleolus.
Methods: A systematic review was conducted across multiple databases following PRISMA guidelines. All levels of evidence were included. A meta-analysis of proportions was performed using the Freeman–Tukey double arcsine transformation for non-comparative studies.
Results: Out of 1,889 initially identified papers, 26 studies were included in the analysis. Twenty-four studies, comprising 1,233 fractures where the posterior malleolus was fixed, reported that 213 cases (12.9%; 95% CI: 6.9%–20.2%) required additional syndesmotic stabilisation. Ten studies analysed 558 fractures where the posterior malleolus was not fixed, and among these, 320 (57.6%; 95% CI: 38.2%–75.9%) required syndesmotic fixation. Five studies assessed syndesmotic reduction, with a reported malreduction incidence of 5.3% (95% CI: 1.2%–11.1%). All but one fracture in the included studies progressed to union.
Conclusion: Fixation of the posterior malleolus provides syndesmotic stability in the majority of cases.
864 - Incidence and patterns of failure of Proximal Femoral Nails
Carlos Argerich, James Li, Sayed Shah, Rudra Prahbu, Niraj Vetharajan
UHB, Birmingam, United Kingdom
The use of proximal femoral nailing (PFN) for extracapsular neck of femur (NOF) fractures is increasing, particularly in frail, co-morbid populations. Given the limited national data, local audits are important for tracking outcomes. This study aimed to assess PFN failure rates and identify recurring failure mechanisms at a high-volume hip fracture center.
A retrospective review of all NOF fracture fixations using PFNs over one year was conducted. Data from 370 patients (average age 83; 69.5% female) were analyzed using electronic medical records, including imaging, complications, and subsequent procedures.
Fixation failure occurred in 12 patients (3.24%). Two main failure patterns were identified: lag screw cut-out and distal peri-implant fractures, each accounting for 41% of failures. Lag screw cut-outs were often linked to ineffective locking mechanisms, likely due to operator error and design flaws. Distal peri-implant fractures frequently occurred through the distal locking screws, suggesting that these screws may act as stress risers.
Less common failure modes included fractures of the distal locking screws themselves and displacement of greater trochanteric fragments during fracture compression.
The overall failure rate aligns with reported literature. The recurrence of specific failure patterns suggests possible technical issues with implant design and surgical technique. Further research is needed to explore whether these failures can be mitigated through design modifications or improved surgical training.
867 - Preoperative ultrasound versus intraoperative findings in evaluating nerve injury post supracondylar fracture in children: diagnostic accuracy and surgical correlation
Amin Abukar, Nimalesh Yogarajah, Kapil Sugand, Ashley Simpson, Anna Panagiotidou, Marco Sinisi, Michael Fox
Royal National Orthopaedic Hospital, London, United Kingdom
Background: Supracondylar fractures are associated with nerve injuries in 11-16% of cases. The nerve injury could result from the initial trauma or post fracture fixation. Decision to explore the nerve is based on a combination of clinical assessment, neurophysiology (NCS/EMG) with imaging. Pre-operative ultrasound scans (USS) could prove to be a useful adjunct in decision-making and expectant management.Aim: This was the first study to compare pre-operative USS and intraoperative findings in patients with nerve injury post-supracondylar fracture.
Method: 22 patients referred to peripheral nerve injury unit between December 2018-2024 were retrospectively reviewed. From examination of the medical records, pre-operative USS as well as intra-operative notes recorded fracture configuration, evidence of nerve injury and its integrity.
Results: Average age was 7 (range 5-11), the majority had Gartland 3 supracondylar fracture. 13 patients had median nerve only affected, 3 had ulnar nerve only affected while 6 had mixed nerve palsy. US scan had high sensitivity for detecting compression/thickening of nerve (0.81) followed by neuroma/swelling (0.67) and structural damage (0.65). US scan had a high specificity in ruling out entrapment of nerve within fracture site (0.94) as well as ruling out presence of neuroma/swelling (0.88).
Conclusion: US scan is a safe, inexpensive, accurate, readily available adjunct modality for evaluating nerve injuries post supracondylar fracture. Its high sensitivity in detecting nerve compression and thickening as well as high specificity in ruling out entrapment and neuroma supports its role in guiding decision making. Integration of US scan into clinical practice may enhance clinical assessment reducing need for unnecessary surgical intervention while ensuring timely intervention for nerve entrapment or damage. Further studies are warranted to assess efficacy in larger patient cohorts and establish protocols for its use.
