BODS/BOA Survey of impact of COVID-19 on UK orthopaedic practice and implications on restoration of elective services
By Bhanu Mishra1, Michael Shenouda2, P. Julian Owen3, BODS Collaborators and Bibhas Roy4
1Post CCT Shoulder Fellow, Manchester University Foundation Trust
2ST-8 T&O, North West London Rotation
3Consultant Trauma & Orthopaedic Surgeon, Cambridge University Hospitals NHS Foundation Trust
4Consultant Orthopaedic Surgeon, Manchester University Foundation Trust
We acknowledge the input of all BODS and BOA members who helped design the survey and then participated in it.
Published 09 October 2020
ABSTRACT
Aims: To assess the impact of COVID-19 on planned orthopaedic surgical practice and the implications on restoration of elective services.
Methods: An online survey of Orthopaedic Clinical Directors was conducted, by BODS (British Orthopaedic Directors Society) in conjunction with the BOA, addressing key questions in relation to planned joint replacement practice, with a focus on targets from NHS England’s (NHSE) third phase of response to the pandemic.
Results: Responses were received from 37% of Trusts and although representatives of all four home countries (England, Wales, Scotland and Northern Ireland) were surveyed, responses were received from England and Wales only.
More than half of responders had no access to ring-fenced elective orthopaedic beds, with over two-thirds reporting no access to operating as part of a network. The large majority (>80%) were not meeting the August 2020 targets of 70% of 2019 practice, and 75% considered that the 2020 targets were unlikely to be achieved. Scenario projections based on NJR data and the present survey suggest we would have to achieve between 143-168% of pre-COVID practice over the next 12-18 months in order to manage the additional caseload generated during the pandemic. 38% of responders were from Trusts/hospitals that had contacted all patients about the disruption to their care, while 8% were from ones that had contacted no patients and 54% had contacted some.
Conclusion: With current models of care, it is difficult to expect existing, and additional upcoming caseload of planned joint replacement care to be processed adequately. Recommended actions include continued utilisation of all available resources, such as independent sector facilities and regional or network collaborative models of care, the use of technology to facilitate care pathways and workflows across geographical boundaries. The variability in contact between Trusts and our/their patients is a concern and since this survey the BOA has published advice for surgeons relating to communication and a statement for patients. NHSE has also produced resources.
Introduction
The COVID-19 pandemic put significant strain on global healthcare systems including the UK. Healthcare workers rapidly altered their professional responsibilities to meet hospital needs while surgeons witnessed dramatic changes in their practices with a decline in elective surgery to 5% of 2019 levels1. An estimated 516,000 planned operations were cancelled in the UK during the initial wave of the pandemic2. This has led to overburdening of elective orthopaedic waiting lists, especially joint replacement surgery, which had already been on the increase prior to the pandemic. Joint replacement operations are some of the most successful life-improving procedures and significant delay can lead to deterioration of physical, mental and social health3-5. 56.8% of patients surveyed prefer to continue with planned surgical care upon resumption of elective orthopaedic services6.
As we moved into phase three of the NHS response to the pandemic, NHSE provided guidance, recommendations and targets to facilitate the NHS priorities from August 2020, which included accelerating the return of non-COVID health services7. The targets in relation to recovering the maximum elective activity possible between now and winter, included an aim to achieve at least 80% of last year’s overnight electives and outpatient/day-case procedures in September, and 90% in October 20207. In phase three, NHSE also advised that “every patient whose planned care has been disrupted by COVID-19 receives clear communication about how they will be looked after, and who to contact in the event that their clinical circumstances change”7.
This paper aimed to assess current practice against these targets, while also addressing some of the interlinked factors that contribute to the successful achievement, or otherwise, of these targets. We also address the key implications of the survey findings on the restoration of elective services in orthopaedic surgery.
Methods
An online survey of Orthopaedic Clinical Directors was conducted with a range of multiple choice, numerical answer, and free text questions. The form was sent to all clinical directors via mobile and email communication on 20th August 2020 and left open for 10 days.
Questions were chosen to address four broad categories:
- Access to appropriate operating facilities
- Current elective arthroplasty practice, in consideration with NHSE target
- Surgical patient prioritisation and communication
- Training opportunities.
These categories were considered vital for recovery of elective services while future-proofing against further COVID-19-related lockdowns. Questions were asked in relation to elective arthroplasty practice, taken as a proxy for overall elective orthopaedic practice, as such cases constitute a significant proportion of orthopaedic practice in a typical UK department.
Responses were anonymised and aggregate data analysed for each question. Due to the variable response rate from different regions and the uncertainty as to whether these responses were representative, data analysis by region was not undertaken.
The authors were satisfied that the range and geographical spread of responses was likely to present a meaningful overall representation of the national picture in orthopaedic elective care. Furthermore, because wide variation was found in the results, even where results are not fully representative of the national picture they provide a valuable insight into the variability that is occurring and highlighted later in the report.
Results
A total of 56 responses were received, representing a 37% response rate. Although representatives of all four home countries (England, Wales, Scotland and Northern Ireland) were surveyed, responses were received from England and Wales only. Full survey results are presented below by category.
1. Access to appropriate operating facilities
52% of responders reported not having access to ringfenced elective orthopaedic facility at present, with 27% describing no plans to consider such a facility within 6 months (Figure 1).
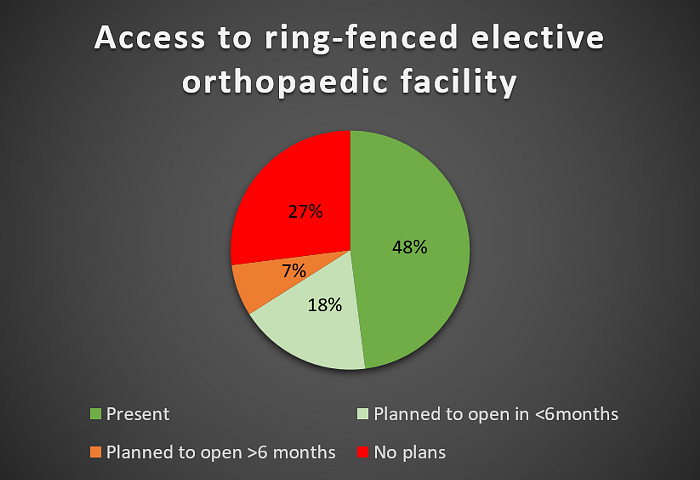
Figure 1
Only 31% of responders reported having access to operating facilities as part of a regional network, with the vast majority of the remainder having no plans to open or become part of such a network in the next 6 months (Figure 2).
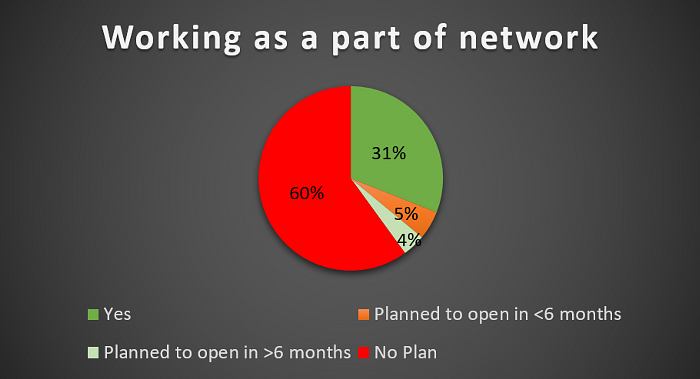
Figure 2
2. Current elective arthroplasty practice, considered against NHS-E targets
At the time of questioning (August 2020), only 18% of responders were achieving the NHSE target of 70% of 2019 practice in August. Only 11% were achieving the September target of 80% of 2019 practice. 75% of responders reported current practice as 50% or less compared to pre-COVID pandemic (Figure 3). The median reported value for current practice was 35% of 2019 caseload. The responses ranged from 0% (5 trusts) to 100% (1 trust).
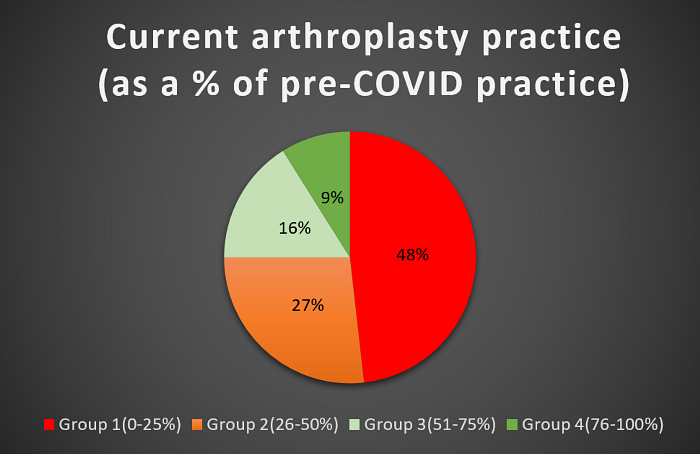
Figure 3
Projecting over the next six months, 90% of responders expected that they would be able to achieve more than 50% of pre-COVID arthroplasty practice by March 2021. However, only 64% of responders expected to achieve more than 75% (Figure 4). The median value for expected March 2021 practice was 80% of pre-COVID caseload.
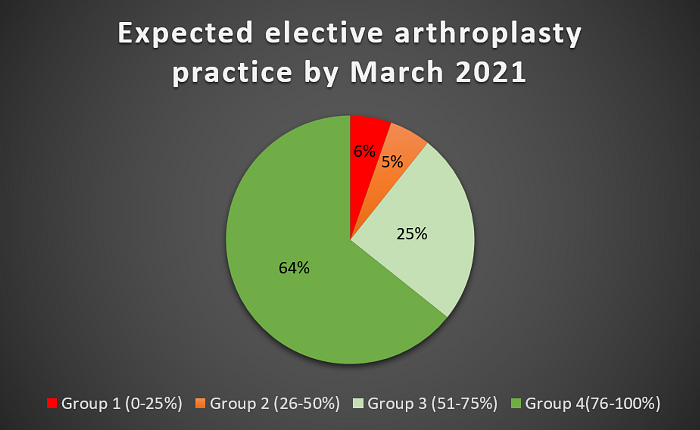
Figure 4
Only 27% of responders felt the August to October NHS-E targets were likely to be achieved – with 73% believing these targets were unlikely or highly unlikely to be achieved.
3. Surgical patient prioritisation and communication
38% of responders reported that within their department, all patients whose planned care had been disrupted by COVID-19 had received information about plans for continuing care and who to contact if their clinical circumstances changed, as per NHSE guidance. Only 8% reported contacting no patients regarding the disruption of their planned care, (Figure 5).
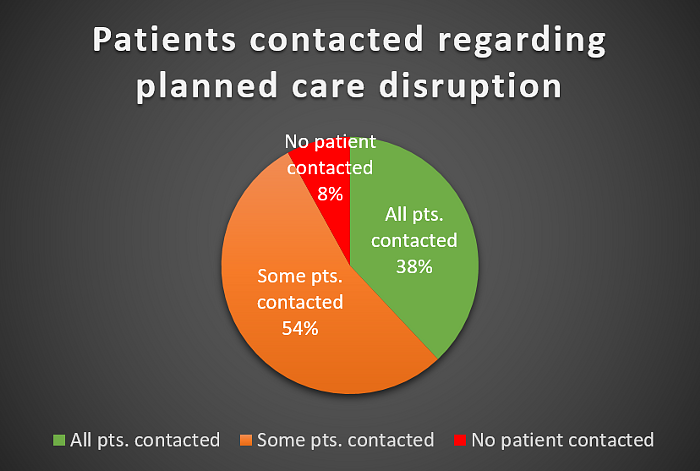
Figure 5
In terms of surgical prioritisation of Priority level 4 patients (surgery that can be delayed for more than three months), 65% of responders reported prioritising patients based on a combination of waiting list order, clinical urgency and being low risk for COVID-19 (Figure 6).
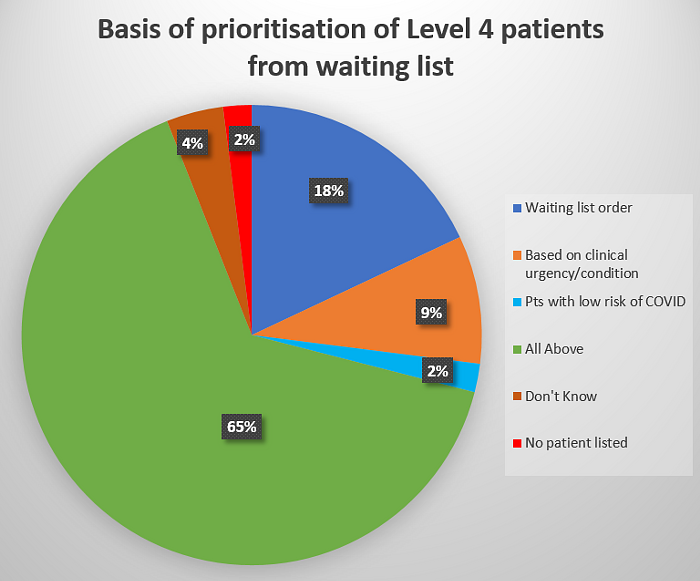
Figure 6
4. Training opportunities
Only 20% of responders reported currently providing sufficient training opportunities for trainees on elective arthroplasty surgery, with 18% unable to provide any training opportunities for such cases, (Figure 7).
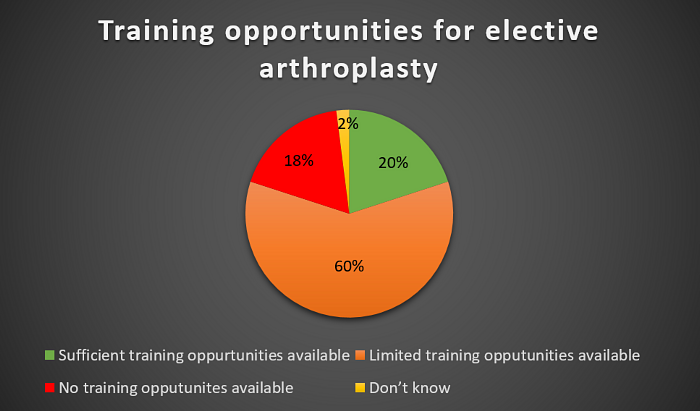
Figure 7
Discussion
Implications of findings
The findings of the present survey highlight some key implications for elective surgical recovery during and after the COVID-19 pandemic. While the survey assessed mostly clinical directors’ present experience regarding only elective arthroplasty surgery, we consider these a proxy for all elective orthopaedic practice, given their large contribution to overall levels of elective orthopaedic surgery. We obtained a response from just over a third of the Trusts in the country. As such, the data should be used with caution to create models of the entire UK Orthopaedic practice.
The latest NHSE and NICE guidelines on arranging planned care in hospitals and diagnostic services state that there should be minimum cross-contamination between teams and sites8. This objective is much more attainable if hospital trusts have access to ring-fenced elective facilities – ideally on a separate site from the acute hospital setting, with appropriate and regular testing of both patients and healthcare professionals. Furthermore, in relation to orthopaedic planned care, BOA guidance on re-starting non-urgent trauma and orthopaedic care published on 15th May 2020 highlighted the importance of establishing COVID free 'green' pathways and integrated care systems beyond individual hospitals or Trusts, for the medium and long-term delivery of orthopaedic services8.
Our survey findings show that a large proportion of responding trusts have neither access to a ring-fenced orthopaedic facility nor access to operating as part of a network model. A high proportion also report that they expect to have neither option in the coming six months. This has huge implications for planned care recovery, with waiting lists likely to soar further for those that cannot access such facilities. Access to appropriate 'green' pathways is imperative in order to: reduce risk of perioperative COVID-19 infection and hence reduce COVID-19-related complications8, avoid the need for COVID-19 infection prevention methods that otherwise slow down surgery and increase PPE required, and improve patient confidence in their safety around the time of surgery. Developing access to such pathways, either as individual trusts or as part of a network, remains a key priority to facilitate planned care recovery. This is likely to be an even greater priority given the impending second wave and possible further lockdown restrictions.
Some respondents provided comments, for example, in relation to the difficulties they have faced in establishing green pathways:
|
“The discussed solutions for major conurbations like London & Manchester are simply not feasible in an area like [ours] where the hospitals are 40 miles apart. […] We have developed a COVID-19 secure pathway for elective surgery but current staffing allows us only one elective in-patient theatre per day qv four pre COVID-19. The situation is dire! “Limited by anaesthetist provision and loss of two theatres to endoscopy. Loss of weekend initiative work due to pay issues with nursing staff.” “The need for a green pathway has made it difficult to run efficient service on the same site as all acute services. We also have to do some specialty trauma through elective theatres so on those days we have to shut theatres to elective admissions because of the separation required by the green pathway.” “Hospital layout hinders more green capacity. Trauma is busier and theatres less efficient. Double the number of trauma lists required. Concern that our ring-fenced orthopaedic ward will be lost due to winter pressures not least because we will not be able to fill it with cases due to the lack of theatre space.” “Combination of challenges, no one thing.” |
The survey also demonstrates the extent of recovery required to meet NHSE’s targets of 70% of normal activity in August, 80% in September and 90% by October 2020. The majority of responders were not even close to these targets, with most indicating these were deemed unlikely to be achievable, and many also indicating that recovery of planned care surgery to >80% of pre-COVID practice may take at least six months, if not longer. As we discuss later, the additional work generated during the pandemic means we will have to operate at significantly higher capacity than 100% of pre-COVID practice – simply replicating prior processes will no longer be sufficient. New models of care, achieving above-normal levels of activity, will be required to clear the additional caseload and return to waiting list times that are acceptable to both patients and clinicians alike.
NHSE’s guidelines surrounding COVID-19 recommend that “every patient whose planned care has been disrupted by Covid-19 receives clear communication about how they will be looked after, and who to contact in the event their clinical circumstances change.”7 . Few responders’ trusts were achieving this, and it is a measure that all surgeons should now undertake to ensure all patients receive communication including an indication as to when their planned care will take place. Patients can also then be given the opportunity to discuss their symptoms further with their surgeon should this be desired. We highlight that since the survey was undertaken, both the BOA9,10 and NHSE11 have published resources to support patient communications.
Furthermore, NHSE guidelines recommend that “clinically urgent patients should continue to be treated first, with next priority given to the longest waiting patients, especially those breaching or at risk of breaching 52 weeks by the end of March 2021”7. Utilising appropriate technology to facilitate the above can significantly help in the recovery of planned care procedures, by allowing close management and efficient coordination of waiting lists, providing appropriate communication and information to patients remotely, and undertaking COVID-19 risk assessments and harm reviews for those patients approaching 52-week breach.
Finally, the reduction in training opportunities is also a concern. While reduced caseload will inevitably lead to a reduction in training opportunities, as we facilitate elective care recovery, it is vital that training opportunities are restored concurrently, ensuring that training the workforce of the future is not impacted further. In addition, the trainee workforce could be a valuable resource in utilising all available facilities and increasing the number of cases that can be operated on, by facilitating lists for senior trainees, with the relevant competence and experience, to perform cases under appropriate supervision.
Projected scenario modelling
In order to estimate the full impact of the pandemic on elective arthroplasty caseload, we modelled some of the most likely scenarios in the next six months, based on 2019 elective arthroplasty NJR data12 and the current state of the pandemic in the UK. In particular, we attempt to project the required levels of practice, as a percentage of 2019 practice, in order to attempt to clear the additional arthroplasty caseload generated during the pandemic.
In order to do this, the following assumptions were made:
- 2019 NJR data recorded 200,434 arthroplasty cases (excluding trauma cases) – averaging 16,703 cases nationwide per month12.
- This monthly figure is used for projecting 'normal' arthroplasty practice.
- 50% of normal joint replacement work was performed in March 2020.
- No joint replacement work was performed from April – July 2020.
- 35% of normal joint replacement work was performed in August 2020 (based on estimates from present survey).
- 20% of normal joint replacement work in 2019 (1st Jan 2019 – 31st Dec 2019) was performed through waiting list initiative or extra theatre session (3rd session of the day) lists.
Scenario 1: Maximum practice achievable from September 2020, with no further COVID-19 related reductions in activity.
While this scenario is rather optimistic, and in fact highly unlikely, this was considered to be the best-case scenario. In this case, an additional 86,020 arthroplasty cases must be performed in the next year, meaning 143% of pre-COVID practice is required just to clear the additional caseload generated during the pandemic.
Scenario 2: Gradual increase in practice over the coming months as follows: 40% September, 50% October, 60% November, 70% December 2020; 80% January, 90% February, 100% March 2021; no further COVID-19-related reductions in activity.
This is a more plausible scenario, particularly with the present rise in COVID-19 cases and predictions that cases will not reduce before early 2021. In this case, an additional 121,097 cases will require arthroplasty surgery by the time normal practice is resumed in March 2021. We would therefore need to operate at 160% of pre-COVID practice for a year from April 2021 to clear the additional case load generated.
Scenario 3: Gradual increase in recovery with slowdown in November-December 2020, associated with potential second wave impact on planned care procedures. Assumed operative caseload of 40% September, 50% October, 50% November, 50% December 2020; 60% January, 70% February, 80% March 2021.
This is probably the most realistic current projection, given the most recent restrictions announced on 22nd September 2020. In this scenario, an additional 136,129 cases will require arthroplasty surgery based on the reduced cases performed during the pandemic. An increase to 168% of 'normal' pre-COVID practice would be required for a year from April 2021 to clear the additional caseload.
Scenario 4: Same recovery as per scenario 3, but with increasing utilisation of theatre capacity by increasing to 3 session lists (12h instead of 9h) on Mondays to Thursdays across all facilities and adding a further two-session list on a Saturday.
In this case, and with the assumption that 20% of cases had been performed on extra session lists previously, the total operative capacity could be increased by a further 22% from 54 to 66 hours per week. If this could be achieved, we would have to practice at 156% of 'normal' pre-COVID levels for a year from April 2021 to clear the additional caseload generated during the pandemic.
In all modelled scenarios, the rate of practice is only to clear additional caseload generated during the pandemic and return to pre-COVID waiting list levels. However, pre-COVID levels of arthroplasty practice were not meeting demand, as demonstrated by rising waiting lists. As these models demonstrate, the NHS faces a mammoth task to deal with the increased workload generated during these unprecedented times.
This has significant social and economic implications, with joint replacements being some of the most successful life-improving procedures, allowing often otherwise healthy patients to continue working where appropriate and/or also continuing their social responsibilities, such as caring for friends and family. Beyond joint replacement surgery, it is likely that the same implications apply for other orthopaedic and non-orthopaedic planned care.
Conclusions and recommendations
We obtained a response from just over a third of the Trusts surveyed. As such, the data should be used with caution to create models of the entire UK Orthopaedic practice but, nevertheless, with current and pre-COVID models of care, it is difficult to expect the existing and additional new caseload of planned joint replacement patients to be operated on in a timely fashion. NHSE targets are expected to be difficult, if not impossible, to achieve; even then it will not be enough to deal with the waiting list load. Additional resources are required to facilitate recovery. Recommendations include an increase in ring-fenced 'green' pathway elective orthopaedic facilities, regional or network collaborative models of care to facilitate maximal efficiency, and continued utilisation of independent sector facilities. Additionally, the use of cloud-based technology to facilitate care pathways and workflows across geographical boundaries will ensure care continues to be delivered safely and independent of individual Trust-restricted systems. Realistic target-setting is essential as is honest communication with patients to set realistic expectations.
References
- Diaz A, Sarac BA, Schoenbrunner AR, Janis JE, Pawlik TM. Elective surgery in the time of COVID-19. Am J Surg. 2020;219(6):900-2.
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020. May 12. [Online ahead of print.]
- Zhang L, Lix LM, Ayilara O, Sawatzky R, Bohm ER. The effect of multimorbidity on changes in health-related quality of life following hip and knee arthroplasty. Bone Joint J. 2018;100-B(9):1168-74.
- Thewlis D, Bahl JS, Fraysse F, Curness K, Arnold JB, Taylor M, et al. Objectively measured 24-hour activity profiles before and after total hip arthroplasty. Bone Joint J. 2019;101-B(4):415-25.
- Scott CEH, Turnbull GS, Powell-Bowns MFR, MacDonald DJ, Breusch SJ. Activity levels and return to work after revision total hip and knee arthroplasty in patients under 65 years of age. Bone Joint J. 2018;100-B(8):1043-53.
- Chang J, Wignadasan W, Kontoghiorghe C, Kayani B, Singh S, Plastow R, et al. Restarting elective orthopaedic services during the COVID-19 pandemic. Bone & Joint Open. 2020;1(6):267-71.
- NHS England (2020). THIRD PHASE OF NHS RESPONSE TO COVID-19. Available at: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/07/Phase-3-letter-July-31-2020.pdf.
- National Institute for Health and Guidance (2020). COVID-19 rapid guideline: arranging planned care in hospitals and diagnostic services. NICE guideline [NG179]. Available at: https://www.nice.org.uk/guidance/ng179.
- British Orthopaedic Association (2020). A message from the British Orthopaedic Association to people waiting for joint replacement and other orthopaedic surgery. Available at: https://www.boa.ac.uk/uploads/assets/0150529d-1fa2-4741-9510d875e4c1a1d0/Patient-statement-re-elective-restart-Sept20-FINAL.pdf.
- British Orthopaedic Association (2020). BOA viewpoint on communications with waiting list patients and those approaching surgery. Available at: https://www.boa.ac.uk/uploads/assets/8afaf96e-b1e8-40d7-b08efb2a4625f4f5/Message-to-surgeons-about-patient-delay-FINAL.pdf.
- NHS England (2020). Clinical Validation of Surgical Waiting Lists: framework and support tools. Available at: https://www.england.nhs.uk/coronavirus/publication/validating-waiting-lists-framework.
- National Joint Registry (2020). Summary of key facts about joint replacement during the 2019 calendar year. Available at: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20AR%20Summary%20key%20facts%202019.pdf.
