Identifying Modifiable Risk factors for Significant Paediatric Orthopaedic Trauma
By Tim Gardner, Mike Reidy and Simon Barker
Department of Trauma & Orthopaedics, Royal Aberdeen Children’s Hospital, Foresterhill, Aberdeen, Scotland, UK
Corresponding author e-mail: [email protected]
Published 29 July 2020
Introduction
During the uncertain COVID-19 era, healthcare services are stretched in ways never seen before. Orthopaedic services have had to adapt significantly to cope with unpredictable change on a regular basis, with elective surgeries necessarily suspended to make way for the pandemic1.
As lockdowns ease and administrations plan their return to ‘the new normal’, it is important to have information to help predict workload going forward. Royal Aberdeen Children’s Hospital (RACH) Department of Paediatric Orthopaedics provides secondary care to the 0-16yr age range in North-East Scotland, along with tertiary care to the North of Scotland and the Northern Isles. The significant paediatric injury burden from the population of the Grampian region is wholly directed to services at RACH.
This study sets out to examine pre-COVID-19 paediatric trauma presentations requiring orthopaedic follow-up, looking at incidence and causative factors, with an aim of providing information on modifiable factors that may be addressed to reduce workload prior to lockdown release.
Methods
Our region has a single large urban centre - the city of Aberdeen – population 224,000 (paediatric population: 32,000)2, several large towns and otherwise comprises a predominantly rural population totalling 668,000. All patients referred to Paediatric Orthopaedic Fracture clinics between 1st May 2012 – 31st April 2015 from the RACH Accident and Emergency Department were included in the study. All children undergoing radiographs for injury were subject to next day ‘Virtual Fracture Clinic’ review by a consultant paediatric orthopaedic surgeon. Any children thereby identified to have injury serious enough to merit orthopaedic review were also included in this study. Minor injuries dealt with wholly at community hospitals or by A&E staff were not included. For the majority of the study period from September 2012, children up to the age of 16 years were accepted in the paediatric fracture clinic in Aberdeen, whereas before this the age range was up to 14 years of age.
A data collection sheet was used in all Paediatric Fracture Clinics held in RACH. It recorded patient demographics and the injuries sustained, as well as notes from each fracture clinic attendance. It serves as the clinical note system for the clinic.
At the point of discharge, data from these sheets for the period under study was prospectively collated into a Microsoft Access® Database then exported to Microsoft Excel® for analysis. Accuracy and quality of data entry was monitored throughout. Injuries were grouped by ‘injury region’ – specific bones or joints, as well as the AO Classification3 of the fracture. Mechanism of injury categories were derived from the Accident and Emergency Department database. The database utilised the patient’s home postcode to categorize into Scottish Neighbourhood Statistics (SNS) Data Zones2, corresponding to ranks in the Scottish Index of Multiple Deprivation 2012. Data Zones throughout Scotland are ranked 1 – 6,205 (with 1 being most deprived and 6,205 being least deprived). Patients whose datazone fell into the NHS Grampian’s catchment area were then aggregated into Deciles to permit comparison of deprivation index with injuries sustained.
The SNS Data Zones were also used to group patients within NHS Grampian’s catchment area according to the Scottish Government 6-fold Urban Rural Classification4, in order to establish any trends by population density. Explanation of this classification can be seen in Table 1, along with a Total Child Population within NHS Grampian.
|
Class |
Description |
Population of Children within NHS Grampian (% breakdown of Total Child Population of NHS Grampian) |
|
Large Urban Areas – 1 |
Settlements of 125,000 or more people. |
32,026 (39.31%) |
|
Other Urban Areas – 2 |
Settlements of 10,000 to 124,999 people. |
10,935 (13.42%) |
|
Accessible Small Towns – 3 |
Settlements of 3,000 to 9,999 people and within 30 minutes’ drive of a settlement of 10,000 or more. |
6,823 (8.38%) |
|
Remote Small Towns – 4 |
Settlements of 3,000 to 9,999 people and with a drive time of over 30 minutes to a settlement of 10,000 or more. |
3,931 (4.83%) |
|
Accessible Rural Areas – 5 |
Areas with a population of less than 3,000 people, and within a 30-minute drive time of a settlement of 10,000 or more. |
19,643 (24.11%) |
|
Remote Rural Areas - 6 |
Areas with a population of less than 3,000 people, and with a drive time of over 30 minutes to a settlement of 10,000 or more. |
8,105 (9.95%) |
Results
Over the three-year sample period, 1,370 patients attended RACH Fracture Clinics. There were 828 boys (60%) and 542 girls (40%). These patients sustained 1,381 injuries (including 11 Polytrauma cases). 29 children attended for temporally distinct injuries within the study period. Annual attendance totals were 323 in 2012-2013, 513 in 2013-2014 and 533 in 2014-15 (In one patient the date of attendance was not recorded).
There is marked seasonal variation (Figure 1), with spring-summer being much busier than autumn-winter.
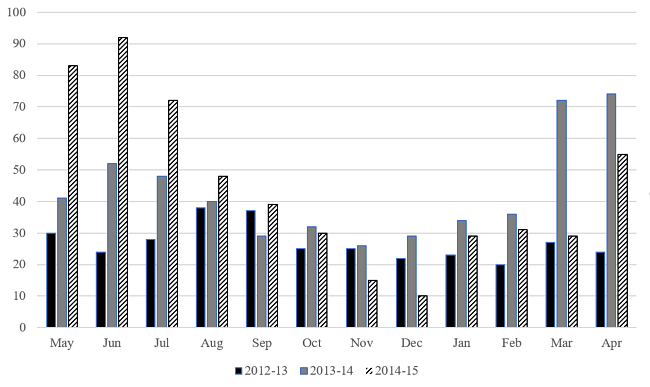
Figure 1: Presentations to Fracture Clinic over the three year sample period by month
The Modal age for presentation is 14 for boys and 10 for girls, and 14 when combined. This reflects the higher incidence in injuries of boys over girls (Figure 2). Around the age of 10, boys show a noticeable increase in incidence over the next four years, whilst girls show a steady decline. One patient had an unrecorded age and was excluded from this analysis.
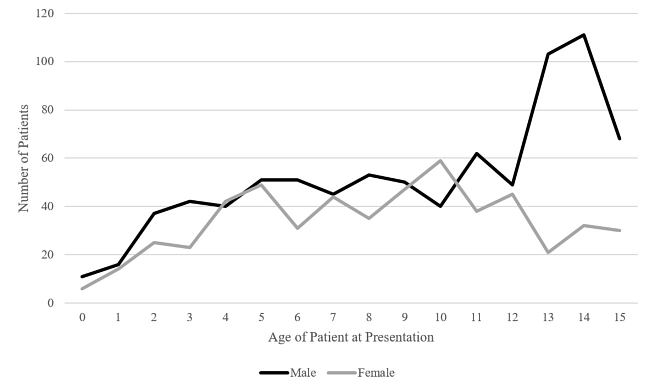
Figure 2: Presentation to Fracture Clinic by Age and Sex over the three year sample-period
Mechanism of injury results are shown in Table 2. The most common recorded mechanism was ‘Fall’, making up 50.78% of all male and 59.96% of all female mechanisms recorded. After ‘Other’ (including non-accidental injury and mechanisms that do not readily fit into a specific grouping), the second most common mechanism in males is ‘Sports’, and in females ‘Trampolines’, together making up around 20% of injuries in boys, and 13% of injuries in girls. Only one male patient was recorded as an assault, and 18 patients over the three year period were reported as being involved in a Road Traffic Accident/Collision (RTA/RTC).
|
|
Male (% of total) |
Female (% of total) |
||
|
Fall |
421 |
50.78% |
325 |
59.96% |
|
Sports |
118 |
14.23% |
19 |
3.51% |
|
Trampoline |
50 |
6.03% |
52 |
9.59% |
|
Bicycle |
43 |
5.19% |
20 |
3.69% |
|
Impact |
50 |
6.03% |
19 |
3.51% |
|
Skiing/Snowboarding |
33 |
3.98% |
12 |
2.21% |
|
Horse-Related |
0 |
0.00% |
10 |
1.85% |
|
RTA/RTC |
9 |
1.09% |
9 |
1.66% |
|
Assault |
1 |
0.12% |
0 |
0.00% |
|
Crush |
14 |
1.69% |
3 |
0.55% |
|
Other |
54 |
6.51% |
54 |
9.96% |
|
Not Described |
54 |
|||
|
Totals |
828 |
542 |
||
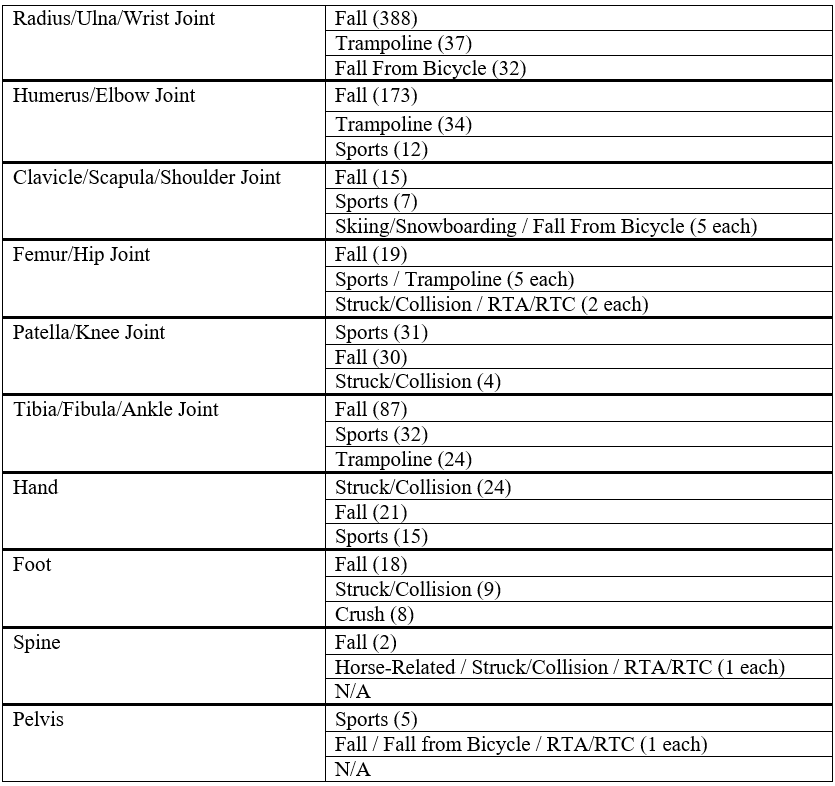
Sites of injury can be seen in Table 3, along with the common causative factors. Injuries to the forearm and wrist made up 40.04% of all fractures in children in the sample (Figure 3). Humerus/Elbow joint injuries are almost equivalent in prevalence to forearm/wrist injuries between ages 4-7; thereafter the incidence of injuries in this region falls with age. As children get older, injuries to the Femur/Hip Joint also become less common, whilst injuries to the Tibia/Fibula/Ankle Joint increase.
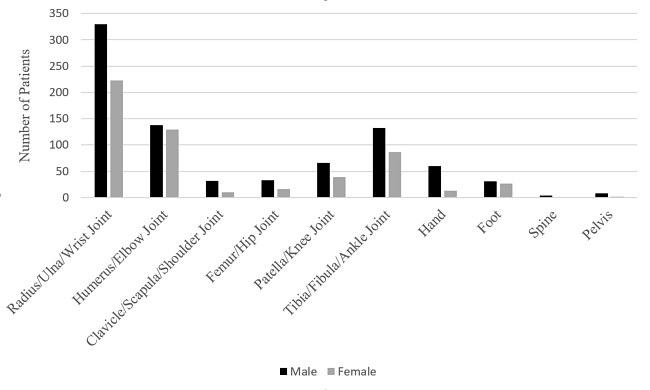
Figure 3: Sites of injury
Along with simple falls, causative factors which feature highly in all categories are trampolines and sports.
Table 3: Injury Sites, with 3 Most Common Mechanisms of Injury (number of patients)
1,344 patients were able to be grouped by SIMD 2012 Deciles. These show an even distribution of injuries through this geographical surrogate measure of deprivation in Grampian (Figure 4). When Decile 1 and 10 are compared (the poorest and wealthiest groups respectively), there is a statistically significant difference between presentation numbers (Z-Score = 2.0964, p = 0.03572), however the difference between any 2 consecutive groups is not significant.
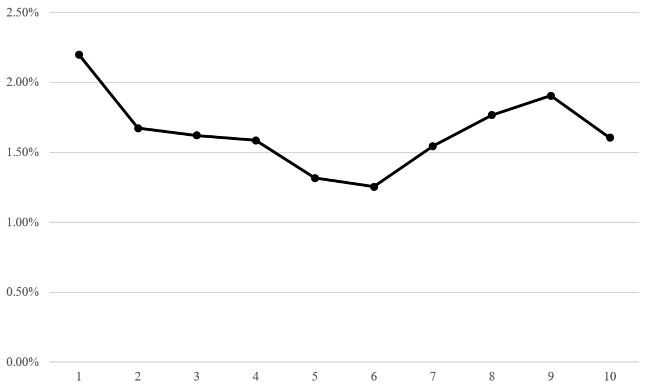
Figure 4: Percentage of Patients seen in Fracture Clinic between 1st May 2012 and 31st April 2015, per SIMD 2012 Decile.
When the same 1,344 Patients are grouped by the UR6 Description of Data zone (Figure 5), patients who live in UR6 Group 3 (Accessible Small Towns) have the highest chance of presenting to Fracture Clinic, with 2.21% of total children presenting during the three year sample group. There is no statiscally significant difference between any of the groups.
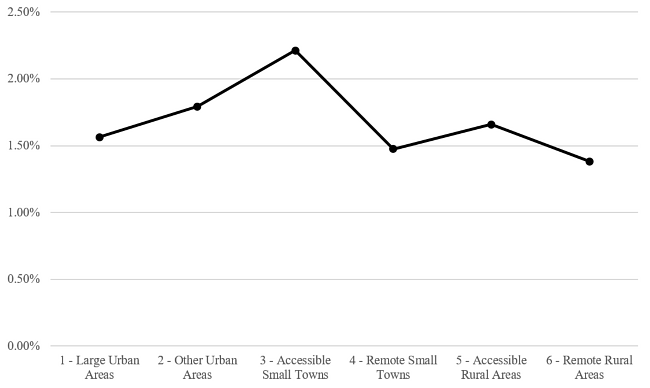
Figure 5: Percentage of Children Presenting to Fracture Clinic per UR6 Description.
Discussion
This study shows that, in normal times, sporting activity (10.0%) and specifically trampolines (a further 7.45%) play a key role in significant injury causation amongst paediatric patients. Effective interventions to limit/guide participation in these activities will therefore have a noticeable impact on the trauma caseload as normal service resumes. Neither deprivation nor rurality appear to have a significant differential impact on injury prevalence. Other studies looking at paediatric head injury5 and post-injury outcomes6 have shown a relationship with deprivation, as has a retrospective cohort study looking at the relationship between trauma and socioeconomic deprivation in adults7. Our study population perhaps takes into account the balancing effect of risk-taking behaviour in adolescents cutting across all socio-economic groupings, cancelling out any effects of deprivation. The effect of rurality appears to be less well-studied, and so it is difficult to compare our study with any others.
When looking at other epidemiological factors, age distribution in the study group demonstrates a typical adolescent peak in injury rates amongst boys in whom contact sport and risk-taking behaviour are traditionally more common. Paediatric orthopaedic services extending to the adolescent age group must therefore respond to a significant and disproportionate injury burden as competitive sports restart post-COVID-19. The increased theatre operating time burden in the adolescent group in whom remodelling is limited will likely further strain resources.
The unimodal distribution of humerus fractures peaking in younger boys and girls fits well with the findings of Rennie et al. (2007)8, who examined epidemiology of paediatric trauma a decade prior to this study. A comparison can also be made with the distribution of hand injuries and Tibia/Fibula/Ankle joint injuries found in this study; however, it is worth mentioning that other injuries do not seem to follow the same pattern, which may be skewed by the fact that a lot of injuries requiring simple management, such as undisplaced wrist fractures or clavicle fractures, do not merit orthopaedic clinic attendance and are therefore excluded from this cohort. When reviewing the data, it should be noted that as children grow, the decrease in Femur/Hip Joint injuries corresponds to an increase in Tibia/Fibula/Ankle joint injuries. Patella/Knee joint injuries seem to increase around the time when competitive sport is becoming more prevalent, supporting the contention that this may be an aetiological factor. Foot injuries do not follow a discernible pattern of distribution, demonstrating a wide range of aetiological factors.
Trampolines are well-known and studied as causes of significant orthopaedic injury in children9, and with commercial trampoline parks becoming more popular alongside family owned equipment, associated injuries continue to become more prevalent10,11. With redeployed staff and lack of available operative capacity1, the trauma burden is not insignificant, although reports confirm a drop in total number cases of up to half in paediatrics12. As lockdown eases13, it is probable that numbers will return to normal levels or higher, and it is important that trauma capacity increases accordingly to accommodate this. This will have an evident knock-on effect, potentially further delaying already overdue elective work .
BOAST and BSCOS guidelines14 have been adapted during lockdown to favour conservative management for more injuries, in order to rationalise available operative capacity. As children are spending more time at home, playing in the garden becomes a solace for both children and parents as a break from the monotony of indoors. It has been noted that trampoline injuries are becoming more common during lockdown15.16, potentially as a result of this. Multiple initiatives have been tried in the past to provide education on the risks of trampolines17,18, however they remain ever-increasing in popularity. Currently, the British Society of Children’s Orthopaedic Surgery have released advice videos particularly highlighting trampolines, along with monkey bars, as high-risk activities during the Coronavirus pandemic19. When used properly (one person at any one time, with protective sides attached, under supervision), they are relatively safe. However, multiple people without any side protection can result in dangerous energy transferred through ‘double-bounces’, projecting the lightest person high in the air with significant injury – resulting in the long-bone injuries that are seen in our study. Given that a $578.3 million growth in sales is predicted during the COVID-19 period20, realistically the trampoline is here to stay. There are inherent dangers however making trampolining safer must become a public health priority, focussing on deliverable messaging. This should include that safer trampolining should be supervised, only ever a single user at a time and always on trampolines with sides on.
Sports services have decreased during COVID-19 lockdown21, along with school closures. This will have an evident effect on the amount of organised competitive sport being played by children, however social sports continue to be played, mostly within the confines of social distancing. Any drop in the 10% contribution from sports-related injuries would have a palpable impact on caseloads going forward. However, sports obviously have a number of other health benefits, both physical and psychological, and rather than being discouraged, they should be performed in as safe a way as possible.
One weakness within this study was the injury mechanism categories, which proved to be insufficiently discriminatory but were constrained by the hospital systems. Falls, the largest single aetiological factor, is too broad a grouping to offer useful comparison and lacks any indication of the energy imparted from the fall. Going forward, it would be prudent to subdivide this category by height of fall as an index of the energy of the injury. The male predilection for ‘sports’ as a cause is reflected in the adolescent male injury peak, and is likely an underestimate, given some of the patients within the ‘falls’ cohort may have been playing sports informally; horse related and trampolining in girls also generate a significant sport-related subset.
Conclusion
When restarting services post-COVID-19, it is important to align this with the re-introduction of normal life for patients. This study shows that during non-pandemic times, around one in five injuries in children appears to have sports or trampolines as a causative factor. When looking at the risk vs. benefits of sports, there a wealth of health benefits that vastly outweigh the potential risks, as for the most part sports are played in a safe and sensible fashion. However, when looking at trampolines, then the risk vs. benefit argument is more challenging. If anything, trampoline use has gone up during lockdown, and vastly supersedes injury mechanisms such as road traffic accidents as a cause of paediatric trauma. It is neither rational nor pragmatic to restrict trampoline use, and so a UK-wide public health campaign is desperately needed to encourage people to use trampolines with a single person at any one time, with sides on, and under supervision. With the rates of injury from trampolines described here being so significant, an approach akin to that of speeding or smoking cessation would appear appropriate to both improve public safety and also help services cope with workload during these unprecedented times.
References
- Al-Jabir A, Kerwan A, Nicola M, Alsafi Z, Khan M, Sohrabi C, et al. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 1. Int J Surg. 2020 May 12;79:168-79.
- Aberdeen City Council (2014). 2012-based Population Projections Aberdeen City and Shire. Aberdeen, Scotland.
- Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and Dislocation Classification Compendium—2018. J Orthop Trauma. 2018;32(Suppl 1):S1-S170.
- Scottish Goverment (2012). Scottish Government Urban/Rural Classfication 2011-2012. Available at: https://www2.gov.scot/resource/0039/00399487.pdf.
- Trefan L, Houston R, Pearson G, Edwards R, Hyde P, Maconochie I, et al. Epidemiology of children with head injury: a national overview. Arch Dis Child. 2016;101(6):527-32.
- Okoroafor UC, Gerull W, Wright M, Guattery J, Sandvall B, Calfee RP. The Impact of Social Deprivation on Pediatric PROMIS Health Scores After Upper Extremity Fracture. J Hand Surg Am. 2018;43(10):897-902.
- Corfield AR, MacKay DF, Pell JP. Association between trauma and socioeconomic deprivation: a registry-based, Scotland-wide retrospective cohort study of 9,238 patients. Scand J Trauma Resusc Emerg Med. 2016;24:90.
- Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38(8):913-22.
- Black GB, Amadeo R. Orthopedic injuries associated with backyard trampoline use in children. Can J Surg. 2003;46(3):199-201.
- Chen M, Cundy P, Antoniou G, Williams N. Children bouncing to the emergency department: Changes in trampoline injury patterns. J Paediatr Child Health. 2019;55(2):175-180.
- Bhangal KK, Neen D, Dodds R. Incidence of trampoline related pediatric fractures in a large district general hospital in the United Kingdom: lessons to be learnt. Inj Prev. 2006;12(2):133-4.
- Christey G, Amey J, Campbell A, Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81-8.
- BBC News (2020). Scotland 'not far away' from eliminating coronavirus. Available at: https://www.bbc.co.uk/news/amp/uk-scotland-53195166. [Accessed July, 2020].
- British Orthopaedic Association (2020). Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. 2020; Available at: https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf. [Accessed July, 2020].
- Buddhdev P, Gille H, Ibrahim Y. The Paediatric Trauma burden of UK Lockdown - Early results in the COVID-19 era. The Transient Journal. May 2020; Available at: https://www.boa.ac.uk/resources/the-paediatric-trauma-burden-of-uk-lockdown-early-results-in-the-covid-19-era.html.
- Farrell S, Schaeffer EK, Mulpuri K. Recommendations for the Care of Pediatric Orthopaedic Patients During the COVID-19 Pandemic. J Am Acad Orthop Surg. 2020;28(11):e477-e486.
- PRNewswire (2017). Orthopaedic Surgeons warn parents and young children about the dangers of trampoliness. Available at: https://www.prnewswire.com/news-releases/orthopaedic-surgeons-warn-parents-and-young-children-about-the-dangers-of-trampolines-300490552.html. [Accessed July, 2020].
- Pediatric Orthopaedic Society of North America (2020). Orthokids: Trampoline and Bounce House Safety. Available at: https://orthokids.org/Safety/Trampoline-and-Bounce-House-Safety. [Accessed July, 2020].
- British Society for Children's Orthopaedic Surgery (2020). Keeping Your Kids Safe During The Coronavirus Pandemic. Available at: https://www.youtube.com/watch?v=32Yxa3rCKbU. [Accessed July, 2020].
- Globe Newswire (2020). Trampolines - World Market Trajectory & Analytics to 2027 with the Potential Impact of COVID-19. Available at: https://uk.finance.yahoo.com/news/trampolines-world-market-trajectory-analytics-112900443.html. [Accessed July, 2020].
- BBC Sport (2020). Lockdown measures: Anger as indoor sports facilities remain closed. Available at: https://www.bbc.co.uk/sport/53157769. [Accessed July, 2020].
