The Provision of Trauma and Orthopaedic Care During COVID-19: The Coventry Approach
By Nicola Mackay, Faiz Shivji, Clare Langley, Michael David, Farhan Syed, Anna Chapman, Pete Thompson, Richard King, Tim Spalding and The Coventry Trauma and Orthopaedics Team*
Department of Trauma and Orthopaedics, University Hospital Coventry and Warwickshire, Coventry, UK
Corresponding author e-mail: [email protected]
Published 05 May 2020
This article is dedicated to the memory of Leilani Dayrit, one of our orthopaedic ward sisters.
Abstract
The COVID-19 pandemic has resulted in the need for rapid reorganisation of trauma and orthopaedic services across the country. University Hospitals Coventry and Warwickshire NHS Trust is a busy Level One trauma facility with 35 consultants providing care over two sites. Elective procedures were stopped, and the department was reorganised continuing to provide major trauma care at University Hospital Coventry, plus ambulatory trauma care at the Hospital of St Cross in Rugby, normally our elective care centre. This paper details the rapid reorganisation of the department and changes to trauma provision, specifically to reduce the number of hospital attendances to patients therefore decreasing potential exposure to COVID-19 for both patients and healthcare professionals by utilising care pathways and web-based services.
Introduction
The COVID-19 pandemic has had a worldwide impact on health services. The NHS has rapidly focussed its resources to saving the lives of those infected with COVID-191. In order to do this, changes in the way each medical and surgical speciality is run has been necessary. Strategic departmental planning in co-ordination with individual Trust’s Major Incident Plans and revised standard operating procedures has occurred nationwide.
This account focuses on how the Trauma and Orthopaedic (T&O) department has adapted across two sites within University Hospital Coventry and Warwickshire NHS Trust (UHCW): University Hospital Coventry (UH Coventry) and the Hospital of St Cross in Rugby. The 2 sites serve a population of 900,000. UHCW is one of three Major Trauma (Level 1) units in the West Midlands and is a tertiary referral centre for orthopaedics, major trauma, neurosurgery, cardiothoracic surgery, hand surgery and plastic surgery. UH Coventry has approximately 1000 beds, including an Intensive Care/High Dependency Unit with 30 beds, and is the site of the Emergency Department (ED). The Hospital of St Cross is where the main elective orthopaedic unit is located, covering both inpatient and day case care, with high medical risk patients treated at UH Coventry.
Orthopaedic provision pre-COVID-19
The T&O department consists of 3 professors of orthopaedics and of rehabilitation, 2 associate professors, 35 consultants, 1 Associate Specialist, 4 staff grade doctors, 18 specialist registrars, 6 higher training fellows, 16 core trainees/foundation doctors and 7 advanced nurse practitioners (ANPs).
At UH Coventry there are 79 orthopaedic beds which look after approximately 500 neck of femur fracture patients per year in addition to general and major trauma admissions. The elective work carried out at the UH Coventry is reserved for complex revision arthroplasty or high-risk patients that are likely to need higher levels of care post-operatively. The adult trauma service is provided by 4 teams, with each team consisting of 4 consultants. A rolling on-call rota provides 24-hour consultant cover all 7 days of the week. There are new and follow-up general fracture clinics each day, although a virtual fracture clinic was due to start in March 2020. Alongside the general fracture clinics, acute upper limb and knee clinics run weekly to which patients can be booked in via primary care or general fracture clinic. There are separate Hand and Paediatric orthopaedic 24-hour on-call services. The Hand Unit is a tertiary referral centre consisting of a combination of orthopaedic and plastic surgeons, providing dedicated new hand trauma clinics 6 days a week, and dedicated day-case hand trauma lists 6 days a week. There are provisions for 24-hour access to trauma theatre with 1 main trauma list running daily 8am-8pm. In addition to this there are complex trauma lists, combined orthoplastic lists and subspecialty-specific lists.
Hospital of St Cross pre-COVID-19
The Hospital of St Cross in Rugby, 12 miles from Coventry, is the home of elective orthopaedic care for the Trust. It has an Urgent Treatment Centre (UTC) which is run by advanced nurse practitioners and supported by the ED consultants at UH Coventry. Normally there are no direct admissions from the UTC, and if inpatient trauma care is required, patients are transferred to UH Coventry. There are separate inpatient medical and orthopaedic wards. The 47 orthopaedic beds are normally filled with elective patients, and patients that require rehabilitation following orthopaedic surgery at UH Coventry. Daytime ward cover is provided by an ANP, GP speciality trainee and a trust grade orthopaedic surgeon. At night this is provided by a 'hospital at night' team comprising a medical junior doctor and ANP.
T&O departmental planning for COVID-19
UHCW NHS Trust planned for an influx of COVID-19 patients requiring high level of acute medical care and respiratory support. A strategy was needed to reconfigure services with the aim of liberating personnel and resources to bolster our ED, ICU and acute medical wards. This needed to be achieved without compromising patient care while minimising unnecessary patient follow-up and interaction with the hospital and potential risk of infection.
Following meetings at Trust and departmental levels, a COVID-19 T&O plan was devised. This involved stopping all elective surgery when the government highlighted this was necessary. Major Trauma and non-ambulatory trauma care were to remain at UH Coventry. The Hospital of St Cross became the site for the assessment and definitive management of ambulatory trauma. Detailed subspecialty pathways were to be developed to achieve the aim of minimising patient attendances. Initially it was not expected that the Hospital of St Cross would remain a COVID-19 free site but this became a later aim as the picture developed and workload became clear. A Standard Operating Procedure was created in the event of an inpatient at the Hospital of St Cross being found to have COVID-19, with the plan to transfer patients to UH Coventry for further treatment.
All junior doctor training rotations were suspended. All the foundation year doctors and most of the trainees in their early years of T&O training were redeployed. This meant that the remaining T&O trainees and subspecialist fellows, including those currently undertaking research, were reorganised onto a general trauma rota based either at UH Coventry or the Hospital of St Cross.
The 16 consultants normally on the trauma rota continued on the UH Coventry rota and the remaining consultants made up the Hospital of St Cross rota. Members of the team understood that if their colleagues suddenly became unwell or needed to self-isolate as per national guidelines, they may have to cover at short notice at either site.
Current organisation at UH Coventry during the pandemic
UH Coventry is still functioning as a level one trauma centre; however, the theatre capacity has been reduced to one 8am-8pm trauma theatre daily with an overnight CEPOD list for emergencies. This has allowed anaesthetists to be redeployed to assist in the care of COVID-19 patients.
A T&O assessment bay has been sent up on the UH Coventry orthopaedic ward for all potential neck of femur fractures and lower limb long bone injuries. Patients are triaged by the ED, appropriate radiographs requested, and sent to the assessment bay via the radiology department. Patients are seen directly by the T&O registrar, thereby bypassing the normal wait in ED. Trauma calls continue to be managed in the Resus bay by the designated trauma team.
The minor injury service at UH Coventry was closed, and all ambulatory trauma has now been redirected to the Hospital of St Cross. Neck of femur fracture patients can be considered for transfer to the Hospital of St Cross pre-operatively, if they show no signs of COVID-19 infection and deemed fit for surgery at that site, to try and decrease their chance of potential exposure to COVID-19. Low risk patients from UH Coventry may also be considered for transfer post-operatively if they show no signs of infection and have negative COVID-19 swabs within the prior 72 hours.
For the management of major trauma, our existing referral process has been modified in order to expedite and streamline referrals from surrounding trauma units (TU) and local emergency hospitals (LEH). This involves a consultant led referral from regional hospital to major trauma consultant on call with the management of some more complex injuries being undertaken locally following appropriate advice.
Non-blue light ambulance transfers from surrounding TU and LEH are coordinated following communication with the trauma and orthopaedic consultant on call, aiming to expedite transfers of stable trauma patients directly to the ward, with assigned trauma leads. ED remains available for patients who need assessment in the resuscitation area as a result of a blue light ambulance transfer.
Open fractures continue to be treated with a combined orthoplastics treatment algorithm that has been in place for some time. The management of fractures is modified such that all patients that require an aerosol generating procedure are deemed COVID-19 positive and appropriate PPE is used. A policy that surgery should be performed by the fastest surgeon is implemented recognising that training is not a current priority. Short cephalo-medullary nails are used to decrease operative time, and absorbable sutures are used to avoid unnecessary follow-up.
The paediatric T&O service is continuing to provide 24/7 care. Paediatric patients are treated in accordance with BOAST guidance for the Management of Children with Orthopaedic Trauma during the COVID-19 Pandemic2. This includes early senior decision making in the Children's ED to ensure the quality and timeliness of patient management. There has been an emphasis on manipulations under sedation rather than general anaesthetic in theatre for conditions such as supracondylar fractures, forearm and distal radius fractures, to reduce the impact on limited theatre capacity whilst ensuring appropriate reduction results. Use of casting materials such as soft cast and reinforced plaster of Paris backslabs to allow home removal by parents is encouraged, with a subsequent reduction of face-to-face follow-up appointments, utilising telephone consultations where possible. Parents are provided with links to the British Society for Children's Orthopaedic Surgery (BSCOS) video resources for advice on how to keep their children safe during the COVID-19 outbreak, as well as how to perform home removal of casts3.
Current organisation at the Hospital of St Cross during pandemic
The aim at the Hospital of St Cross is for all patients to have assessment and definitive non-operative management on the same day so as to avoid repeat visits to the hospital. Where operative treatment is required, we try to provide this at index presentation to reduce hospital visits and reduce exposure. A minor operations suite which includes appropriate lighting and a portable x-ray machine, has been setup in an adjacent bay to help achieve this. This is reserved for surgical cases that can be performed under local or tumescent (wide awake local anaesthesia no tourniquet, WALANT) anaesthesia. If surgery needs to be scheduled on another day due to limitations in capacity, appropriate surgeon availability or due to patient factors, then these patients are tested for COVID-19 and advised to self-isolate at home until surgery with supporting written advice provided. Direct admissions from the UTC under T&O became available, with operative treatment on trauma cases being performed at this site. Where possible, a non-operative approach to treatment is preferred as per the current BOAST guideline2.
To meets these aims, the T&O team have situated themselves in the UTC. All patients with limb injuries are initially seen by the ANPs then senior reviewed by T&O so a definitive treatment plan is given and initiated on the day. This means these patients no longer require a new patient fracture clinic appointment. A T&O registrar is based in the UTC 24-hours each day, in addition to a plastics registrar, general T&O consultant, and Hand consultant during daytime hours (0800-2000). If demand increases then the orthopaedic team (regardless of grade or seniority) is to step-up to the frontline to reduce numbers of patients congregating in the waiting area, again as a measure to reduce risk of exposure.
A comprehensive supply of braces for all limb injuries is available in the UTC, restocked by the orthotics department. Senior hand therapists and plaster technicians are available to support splint and cast application as well as to provide patient education at the index presentation as part of any definitive treatment. A key part of the organisation has been the creation of a UTC coordinator role, currently being filled by our senior hand surgery nurse.
Trauma care algorithms
Each subspecialty was tasked with writing their Coventry Orthopaedics Vital Information Documents specific for the management of T&O trauma patients in the COVID-19 pandemic. Specific ‘COVID’ acute knee, shoulder & elbow, foot & ankle, and hand guidelines were circulated to the department and uploaded to the intranet. These were written under the supervision of the lead for each subspecialty and included treatment pathways, online physiotherapy programs and contact details if patients had any ongoing concerns.
Knee injury C.O.V.I.D. guidelines (Table 1)
Where possible, all knee injuries are treated with injury-specific online physiotherapy with virtual or (rarely) face-to-face clinic review at 6-12 weeks, as decided by a consultant. Every patient is given a business card with two websites and QR codes (Figure 1) that direct the patient to an information website and physiotherapy website (www.uhcw.info). Infographics are available for common injuries such as meniscal tears, ACL ruptures, collateral ligament injuries, and patella dislocations.
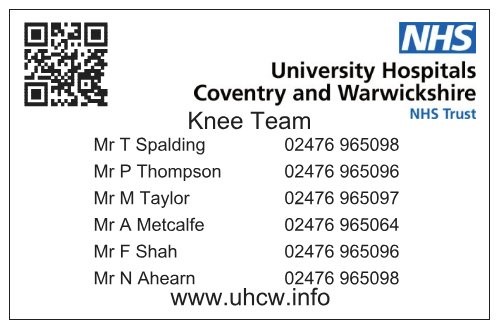
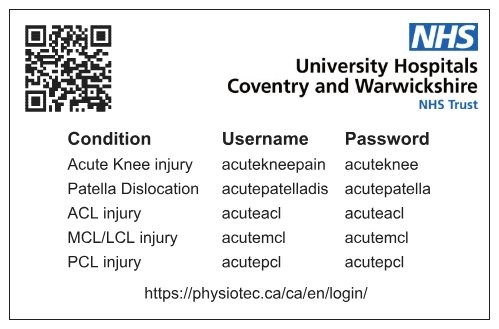
Figure 1: Knee Team business card
For knee injuries such as meniscal tears without locking or OA flares, standard advice is given, and general online physiotherapy recommended. NSAIDs and steroid injections are not given but patients are recommended to seek re-referral if not improving. Suspected ACL injuries are given an ACL brace (if functional instability present), online ACL physiotherapy and are directed to the online infographic. Non-urgent MRI scans are ordered and subsequently reviewed remotely, informing the patient by phone. Clinic review is booked for 3 months. LCL and MCL injuries follow the same pathway as ACL injuries, except the brace used and regimen differs. Reduced patella dislocations are given a hinged knee brace and online physiotherapy. Patella/quadriceps tendon ruptures, multi-ligament injuries, locked knees, and acute PCL injuries are all given braces where required and booked into the weekly acute knee clinic based at the Hospital of St Cross, where 3 'same-day' MRI slots have been allocated for use by the knee team, so assessment, diagnosis and management decisions can all be performed in a single visit. Operations are then planned on the trauma list if required.
Detail of the pathway is given in Table 1. Patients are advised of the nature of compromise to the normal pathway for handling knee injuries, but patients are informed that for all options the safety net is the physiotherapist or the consultant’s secretary, and that information is on the website (www.uhcw.info).
Table 1: Knee injury C.O.V.I.D. guidelines
|
INJURY |
MANAGEMENT |
|
General knee pain
|
Situation: Knee problem not fitting into below categories Management:
|
|
Multi-ligament knee injury |
Situation: Grossly unstable knee with multi-direction instability. May or may not be truly dislocated. Remember to assess NV status, ABPI if unsure. >0.85 Management:
|
|
Patella Tendon / Quads tendon Rupture |
Situation: inability to SLR, Palpable gap Management:
|
|
ACL |
Situation: Twisting injury with pop, Effusion and often can’t extend due to pain. Increase AP movement on Lachman Management:
|
|
LCL or MCL |
Situation: Unstable or pain on varus-valgus or just pain Management:
Full MCL regime:
If LCL, assess NV status, treat as potential multi-ligament injury, Apply TROM brace, discuss with knee team. |
|
PCL |
Situation: Direct fall or impact on proximal tibia. Loss of step-off feeling tibia to femur at 90. Management:
|
|
Locked knee |
Situation: Twisting injury with medial or lateral pain. Won’t go straight and not an MCL injury with pain on epicondyle. Management:
|
|
Patella dislocation |
Situation: Good history of patella dislocation, tender medial parapatellar border Management:
|
|
Osteochondral fragment |
Situation: Acute knee injury with bony fragment visible on X-ray with or without locking Management:
|
Shoulder and elbow C.O.V.I.D. guidelines (Table 2)
Clavicle fractures and acromioclavicular joint dislocations are treated non-operatively with a sling for comfort and online physiotherapy unless there is skin compromise. All shoulder and elbow dislocations have closed reduction performed in the UTC, but if unsuccessful these can be added to the trauma list. First time shoulder dislocations are all referred to physiotherapy. If there are any ongoing concerns with instability recognised by the physiotherapists a formal shoulder and elbow opinion in gained. In first-time shoulder dislocations with associated bony pathology an urgent outpatient CT scan is requested and followed up appropriately. All recurrent shoulder dislocations are referred to physiotherapy, and these only require discussion with a consultant if ongoing concern. Rotator cuff tears in patients under 60 years are assessed with an urgent outpatient ultrasound scan, referred to physiotherapy and operated upon where required. Undisplaced proximal humeral fractures are treated in a sling for 3 weeks and online physiotherapy with telephone follow-up with a physiotherapist. Displaced proximal fractures in patients under 65 years are discussed with a shoulder & elbow consultant to consider operative intervention.
Detail of the pathway is given in Table 2. Physiotherapy requests are vetted by the team for either face-to-face assessment or virtual appointments. Rehabilitation programs are available in written format or online at www.uhcw.info.
Table 2: Shoulder and Elbow C.O.V.I.D. guidelines
|
INJURY |
MANAGEMENT |
|
SHOULDER |
|
|
Clavicle fracture |
|
|
AC joint dislocations |
|
|
1st time shoulder dislocations |
|
|
1st time shoulder dislocations with bony involvement |
If Glenoid rim or bony Bankart fractures:
|
|
Recurrent dislocators |
|
|
Rotator cuff tears |
|
|
Proximal humerus fractures - undisplaced |
|
|
Proximal humerus fractures - displaced 2,3 and 4 part fractures |
Aged >65 years
|
|
Proximal humerus fractures - displaced 2,3 and 4 part fractures continued |
Aged <65 years
Contact S&E consultant if believe would benefit from surgery |
|
Humeral shaft fractures |
Concerns re: fracture morphology and possible surgery to be discussed with trauma service, not S&E service |
|
ELBOW |
|
|
Elbow dislocation - simple |
|
|
Elbow dislocation - complex |
|
|
Distal humeral fractures – extra articular |
|
|
Distal humeral fractures – intra articular |
|
|
Distal biceps rupture |
|
Foot and ankle C.O.V.I.D. guidelines (Table 3)
The new foot and ankle guidelines follow the same format as the acute knee and the shoulder and elbow guidelines aiming where possible to give patients a definitive treatment plan at their first clinical presentation in the UTC. The extended scope physiotherapists have made online rehabilitation programs on ‘Physiotec’ (https://physiotec.ca/uk/en) and patients are given a username and password for this on discharge from UTC.
Any patients presenting with non-specific atraumatic foot and ankle pain are given simple analgesia if required, broad advice (including information on supportive footwear) and a physiotherapy treatment plan. Ankle sprains and Weber A ankle fractures are managed with rest, ice and elevation. They are advised to weight bear as tolerated, given a rehabilitation plan and provided with a fixed angle walker boot. Weber B ankle fractures with no initial talar shift can weight bear in a fixed angle walker book and have a weight bearing X-ray at 1 week to determine stability. If there is talar shift on this X-ray surgical intervention is arranged. All displaced Weber B and Weber C fractures are booked for surgery immediately if swelling and capacity permits, or they are put on the department’s ankle pathway where surgery is performed at 5-7 days. Bimalleolar and trimalleolar ankle fractures are reduced in UTC and put on same pathway for surgical fixation. Pilon fractures have a pre-operative CT prior to surgical intervention. Achilles tendon injuries are managed in an Aircast® boot with serial removal of wedges over an 8 week period supervised by the physiotherapy team. Surgical intervention is offered to all Lisfranc injures. Calcaneal, metatarsal and toe fractures if closed injured are managed non operatively with appropriate orthotic appliances.
The full foot and ankle pathway is shown in Table 3, which also includes treatment guidelines for non-traumatic presentations such as diabetic foot problems and Charcot arthropathy.
Table 3: Foot and Ankle C.O.V.I.D. guidelines
|
INJURY |
MANAGEMENT |
|
General ankle pain, non-traumatic |
Situation: General foot and ankle pain with no concern for septic arthritis Management:
|
|
Ankle sprain |
Situation: Ankle pain following injury where X-ray demonstrates no bony injury Management:
|
|
Weber A ankle fracture |
Situation: Lateral ankle pain with confirmed Weber A fracture Management:
|
|
Weber B ankle fracture |
Situation: Need to determine if stable or unstable fracture, but unable to do this on day of injury Management: talar shift present
Management: No talar shift
|
|
Weber C ankle fracture |
Situation: Unstable ankle fracture Management:
|
|
Bimalleolar/Trimalleolar ankle or Pilon fracture |
Situation: Unstable ankle fracture Management:
** If skin threatened following attempted reduction after 8pm and cannot be dealt with at Hospital of St Cross, patient to be transferred to UH Coventry; if only minimal displacement without skin threat admit and case can be done the following morning on trauma list at Hospital of St Cross |
|
Achilles tendon injury |
Situation: Positive Simmond’s test + palpable gap +/- increased resting angle Management:
|
|
Calcaneal fractures |
Situation: Ensure no other injuries Management:
** If tongue type fracture with skin threat for theatre- DW on call consultant |
|
Potential Lis franc injury |
Situation: High energy injury exclude other injuries Management:
|
|
Metatarsal fractures |
Situation: Isolated metatarsal fractures Management:
|
|
Toe phalanx fractures |
Situation: If closed NV intact Management:
|
|
Toe dislocations |
Situation: Any toe dislocation Management:
|
|
Diabetic foot problems |
Situation: Refer to vascular team at UH Coventry, if not possible due to COVID crisis we accept patients that require urgent inpatient care such as IVAbx, I&Ds or debridement. DW on-call consultant Management:
|
|
Charcot arthropathy |
Situation: Swollen foot and ankle, painful or painless, warmth, erythema, positive Buergers test, X-ray Management:
|
Hand and wrist C.O.V.I.D. guidelines (Figure 2)
The hand team has consultant presence in the UTC between 8am-8pm daily to provide a one-stop service wherever possible. Splints and casts that can be removed at home by the patient are used as appropriate. Conservatively managed wrist fractures are put into a full below elbow removable cast, both written instructions along with an online video to demonstrate guide self-removal at home. Procedures that can be performed under local or tumescent anaesthesia are carried out in UTC such as exploration and closure of wounds, extensor tendon repairs, washout of animal bites and removal of foreign bodies. Vicryl rapide is used for wound closure rather than a non-absorbable suture to avoid the need for removal either in hospital or GP surgeries. Patients are treated in accordance with guidance published by the British Society for Surgery of the Hand (BSSH) on the management of hand injuries during the COVID-19 pandemic4.
Prior to the pandemic, the UHCW Hand Centre had already audited and embraced the philosophy of early discharge through the use of patient-initiated follow-up (PIFU). Business cards (figure 3) with simple advice, hand exercises and contact details had been produced. This was supplemented by their website (www.tinyurl.com/UHCWhand) that has been rapidly upscaled to include numerous patient information leaflets and videos to guide patients through their rehabilitation and promote self-care at home. Our hand therapy unit have worked side by side with us in this endeavour and provide further support through virtual and face-to-face appointments. All patients with hand or wrist injuries coming through the UTC are provided with a PIFU business card as a safety net to ensure they have a direct line of communication in case they run into trouble or need to arrange follow-up. The hand trauma pathway is shown in figure 2.

- All patients should book in via UTC reception for tracking reasons.
- Aim to treat injuries and provide sufficient advice so that patients do not need to return. Use removable splints/backslabs and absorbable sutures. Supply patient with spare dressings. Document history, examination and treatment using ‘Add note’ on CRRS. Recommended use of hand assessment proforma1.
- Give patient the UHCW Hand Centre business card which includes simple hand exercises, the UHCW Hand Centre web address and a contact number (02476 965072 – hand coordinator office) in case they need to get in touch regarding problems or need to arrange a follow-up visit.
- Keep the patient details on the shared drive for discussion at the trauma meeting the next morning (including plastics patients). Management plans will be checked and changes can be made if necessary.
- For help with a specific injury, refer to BSSH trauma triage tool which has been adapted to account for the Covid-19 pandemic: https://handinjurytriageapp.bssh.ac.uk.
- If you are still not sure what to do, contact the hand surgeon on call.
- Patient pathway:
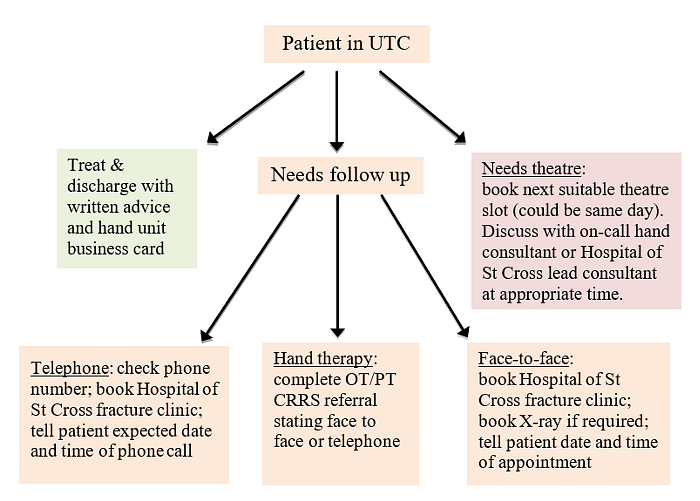
Figure 2: Hand and Wrist C.O.V.I.D. guidelines

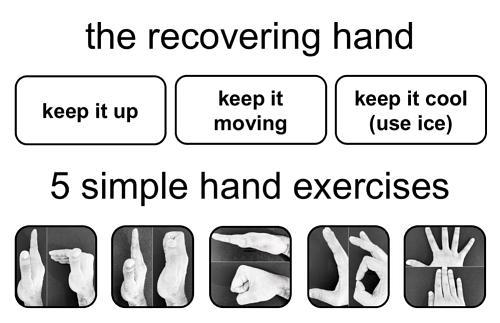
Figure 3: UHCW Hand Centre business card
Ongoing outcome monitoring
Currently the UTC in the Hospital of St Cross appears to be functioning well, and early feedback from the ANPs situated in the UTC, who tend to work relatively independently under normal conditions, is positive as they benefit and learn from collaborative working with the T&O doctors. The orthopaedic assessment bay on the T&O ward at UH Coventry has also facilitated early senior management plans for patients. Monitoring of activity, outcomes and these innovative pathways will continue throughout the COVID-19 pandemic. This will determine which aspects of the emergency planning stay in place and which return to normal.
Discussion
During a period of unprecedented demands, the T&O department at UHCW NHS Trust acted swiftly to reconfigure its service and provision of trauma care for the region. We repurposed our elective ‘cold’ site to provide high quality trauma care for those who need it, away from the busy central unit which treats the majority of COVID-19 cases. We have detailed the changes and innovations made. This process has been facilitated by strong leadership, clear aims, and collaborative working.
We believe patients have benefitted from early senior clinical management plans via frontline consultant presence, albeit in a different location. Trauma care was standardised via specialty-specific guidelines, reducing variation in treatment, and facilitating definitive management while minimising hospital visits and consequent exposure. Multimedia technology solutions have been embraced with patients being directed to websites providing injury-specific advice and rehabilitation guides, along with telephone consultations in the effort to reduce face-to-face follow-up and minimise COVID-19 exposure.
The T&O team working directly in the UTC essentially eradicates the need for new fracture clinic appointments and therefore may in the long-term be cost saving. However, the feasibility of staffing the UTC with registrars 24 hours a day is debatable due to the cost and implication on training. In addition, there will always be a need for fracture clinic appointments due to referrals from other primary care providers. The success at UH Coventry and the Hospital of St Cross should be balanced against the background of a lower demand for trauma services and the abolition of elective services during this pandemic.
In time the effect of COVID-19 on trauma and elective patient care will need to be determined by analysing the outcomes of patients. At the time of submission we are unaware of any patient experiencing a compromise in quality of care through implementation of this system, but we accept there has been an increased rate of non-operative treatment. This is understandable as the potential harm to patients of contracting COVID-19 is far more detrimental than a malunited fracture. However, in the long-term it is vital we assess if this approach leads to increased levels of corrective or salvage procedures.
The departmental changes which have occurred will likely have a substantial impact on orthopaedic registrar training. As a surgical speciality, the time spent in theatre is essential and this has been dramatically reduced due to the reconfiguration of services, the decreased number of patients presenting with injuries, and reduced operative management. In contrast, opportunities have been given to trainees to carry out service improvement projects, and to demonstrate flexibility, initiative and leadership skills. As a consultant such qualities are essential.
Over the coming months the Trust and T&O department will need to review service provision as the number of COVID-19 patients decreases. In particular, the management of significantly increased elective new patient clinics and surgical waiting lists will need to be addressed. Constant reassessment and analysis of practices will be important to facilitate optimum patient care. In order to do this communication between all departments within the Trust will be required to ensure the correct balance is established. It is also important that any permanent change in service provision following the COVID-19 pandemic is investigated with regard to potential gains and losses before implementation.
Limitations of this study
We recognise that this paper is specific for this geographic area. However, the principles of altering the structure of patient care based on the needs of a department and hospital remain the same. We hope this paper provides hospitals around the country with a potential method to manage both this current and any future crisis.
Conclusion
The COVID-19 crisis has provided an extraordinary challenge to the T&O department at UH Coventry and the Hospital of St Cross. Dramatic changes in rapid succession have occurred to reorganise the department. Working together as a team under a strong departmental lead has been essential. Streamlined care pathways and web-based services have been produced to reduce the number of face-to-face hospital visits. This decreased exposure to COVID-19 for both patients and healthcare professionals alike. Our approach could be utilised in other T&O departments.
References
- Thornton J. How Clinicians are leading service reconfiguration. BMJ. 2020;369:m1444
- British Orthopaedic Association (2020). Emergency BOAST: Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Available at: https://www.boa.ac.uk/resources/covid-19-boasts-combined.html.
- British Society for Children's Orthopaedic Surgery (2020). Covid-19 Resources. Available at: https://bscos.org.uk/covid19/resources.php.
- Hand Injury Triage App 2020, British Society for Surgery of the Hand (2020). Hand Injury Triage App. Available at: https://handinjurytriageapp.bssh.ac.uk/home.
*Coventry Trauma and Orthopaedics Team
T&O Consultants: Mr Nathanael Ahern, Mr Mateen Arastu, Mr Gevdeep Bhabra, Mrs Anna Chapman, Mr Stephen Cooke, Mr Wael Dandachli, Mr Michael David, Mr Vivek Dhukaram, Mr Stephen Drew, Mr Pedro Foguet, Mr Andrew Fowler, Professor Damian Griffin, Mrs Helen Hedley, Mr Chris Hill, Mr Matthew Jones, Professor Richard King, Mr Jakub Kozdryk, Ms Clare Langley, Mr Thomas Lawrence, Mr Andrew Mahon, Mr John McArthur, Mr Andrew Metcalfe, Mr Chetan Modi, Mr Sunit Patil, Mr Giles Pattison, Mr Darryl Ramoutar, Mr Housam Raslan, Mr Bryan Riemer, Mr Feisal Shah, Mr Robert Sneath, Mr Tim Spalding, Mr Farhan Syed, Mr Mark Taylor, Mr Peter Thompson, Mr Peter Wall, Miss Jayne Ward, Mr Daniel Westacott, Mr Richard Westerman, Mr Jonathan Young.
T&O Associate Specialist: Mr Asgar Ali
T&O Staff grades: Mr Khalil El-Bayouk, Mr Okpako Ikogho, Mr Ali Saad.
T&O registrars/fellows: Mr Imran Ahmed, Mr Firas Arnaout, Mr Tim Barlow, Mr Tom Cloake, Mr Vito Coco, Mr Christopher Downham, Mr Miguel Fernandez, Mr Kanai Garala, Mr Andrew Grazette, Miss Elizabeth Hedge, Miss Sarah Henning, Mr James Li, Miss Nicola Mackay, Mr Avi Marks, Mr James Masters, Mr James Miller, Mr Vlad Paraoan, Miss Olivia Payton, Mr Deepak Samson, Mr Alexander Schade, Mr Shafiq Shahban, Mr Faiz Shivji, Mr Mathew Weston, Mr Christopher Wilding.
Advanced nurse practitioners: Mrs Anna Baker, Mrs Lauren Beardmore, Miss Lucy Dalton, Mrs Filo Eales, Mrs Louise Fraser, Mrs Morag Green, Mrs Gail McCloskey, Mrs Suzanne Woodridge.
UTC co-ordinator: Mr Simon Dickens.
T&O management: Mr Alistair Nutting, Mrs Juliet Starkey, Mrs Elaine Taylor.
Senior nursing management: Mrs Sarah Hartley, Mrs Paula Seery, Mrs Chris Seddon.
